Translate this page into:
Is Freehand Technique of Pedicle Screw Insertion in Thoracolumbar Spine Safe and Accurate? Assessment of 250 Screws
Address for correspondence: Dr. Raju Venkatesh, 2, Palaniyappan Street, Kanthakonar Layout, Kavundanpalayam, Coimbatore - 641 030, Tamil Nadu, India. E-mail: tharunvenkatesh@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Pedicle screw fixation is one of the widely used procedures for instrumentation and stabilization of the thoracic and lumbar spine. It has the advantage of stabilizing all the three columns in single approach. Various assistive techniques are available to place the pedicle screws more accurately but at the expense of increased exposure to radiation, prolonged surgical duration, and cost.
Objective:
The objective of this study is to determine the accuracy and safety of pedicle screw fixation in the thoracolumbar spine using freehand surgical technique.
Materials and Methods:
We evaluated all patients who underwent pedicle screw fixation of the thoracolumbar spine for various ailments at our institute from January 2016 to December 2017 with postoperative computed tomography scan for placement accuracy. We used Gertzbein classification to grade pedicle breaches. Screw penetration more than 4 mm was taken as critical and those less than that were classified as noncritical.
Results:
A total of 256 screws inserted in T1–L5 vertebrae were included from 40 consecutive patients. Six screws were excluded according to selection criteria. The mean age was 39 years. Trauma (36 patients) was the common reason for which the pedicle screw fixation was done followed by degenerative disease (2 patients) and tumour (2 patients). A total of ten pedicle screw breaches (4%) were identified in eight patients. Among these, three critical breaches (1.2%) were occurred in two patients which required revision. The remaining seven breaches were noncritical and kept under close observation and follow-up.
Conclusion:
Pedicle screw had become the workhorse of posterior stabilization of the spine. Based on external anatomy and landmarks alone, freehand technique for pedicle screw fixation can be performed with acceptable safety and accuracy avoiding cumulative radiation exposure and prolonged operative time.
Keywords
Accuracy
freehand technique
pedicle screw breach
thoracolumbar spine
INTRODUCTION
The pedicle screw traverses all three columns of the spine. It acts as a strong bridge across these columns and provides strong fixation even in three column disruption. Boucher[1] was the first to use pedicle screws and subsequently popularized by Roy-Camille et al.[2] Inserting pedicle screw remains technically demanding with a long learning curve. Hence, many techniques have evolved to facilitate safe and accurate screw placement.[345] Freehand technique based on external bony landmarks is one of the reliable and safe procedures. Reducing radiation exposure is the main advantage of this technique. The aim of this study was to evaluate the accuracy and safety of freehand technique.
MATERIALS AND METHODS
Forty patients who required pedicle screw fixation of the thoracolumbar spine for various ailments admitted from January 2016 to December 2017 were enrolled for our study. After thorough evaluation, pedicle screws were inserted using freehand method by five neurosurgeons. Whenever fluoroscopic guidance was used for placement in certain circumstances those screws were excluded from the study. Accuracy of the placement of pedicle screws was evaluated with postoperative computed tomography (CT) scan. Gertzbein classification was used to grade pedicle breaches. Further, anterior cortical breach of the vertebral body was measured similarly. Screw penetration >4 mm was taken as critical because of their proximity to vital structures. Screw penetration <4 mm that remains within safe zone was classified as noncritical.
Surgical technique
After meticulous exposure, fluoroscopy was used for level localization and to assess the spinal alignment. The muscle dissection was performed adequately to palpate the transverse process. The intersection formed by the bony confluences of the transverse process, pars interarticularis, and the mammillary process of the lumbar vertebrae was chosen for pedicle entry site.[6] Likewise, the center of the triangle formed by the medial border of the transverse process, the lower border of the superior articular facet, and the pars interarticularis in the thoracic spine was selected for pedicle entry.[6] An awl or drill was used to create a hole at the pedicle entry. The advancement of the pedicle probe should be smooth and consistent with the bony feel and should follow the trajectory that parallels the superior endplate. Then, the pedicle sound was used to identify any breach which was an important step in freehand technique. Following the assessment of the integrity of the tract with a feeler, a “tap” was used before inserting the pedicle screw [Figures 1 and 2].
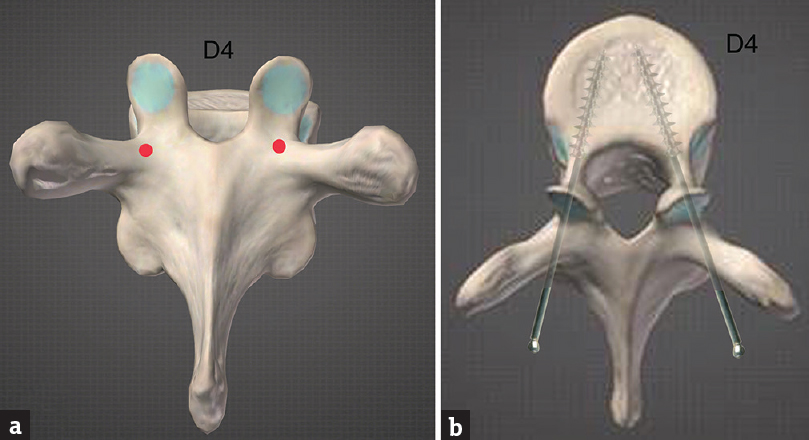
- (a) Thoracic entry point at D4. (b) Trajectory of screw
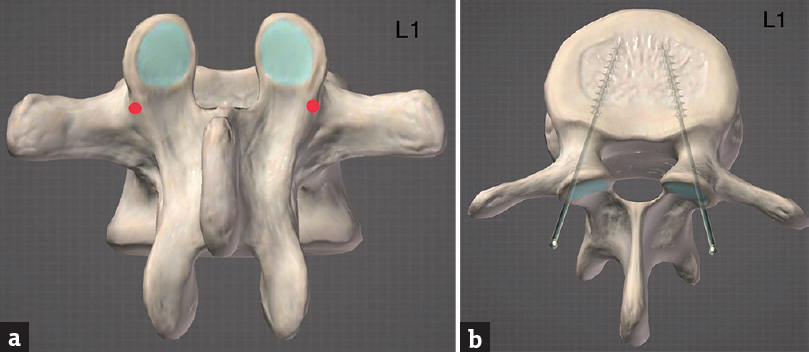
- (a) Entry point at L1. (b) Trajectory of screw
Data collection
We prospectively reviewed all the pedicle screws that were inserted by the freehand technique in the thoracic and lumbar spine at our institute from January 2016 to December 2017. The screw insertions were done by five neurosurgeons independently using external landmarks as guidance. Patients’ age, sex, and the indication for which pedicle screw fixation was done were collected. Intraoperatively during the pedicle probing if any cortical violation suspected, fluoroscopy guidance was sought and, if necessary, the screw was repositioned satisfactorily. Such fluoroscopically assisted screws were excluded from the study. The objective evaluation of the accuracy of pedicle screw insertion was done by CT scan done within 24 hours postoperatively. The presence and extent of cortical breach by any misplaced screw were analyzed and revision was done in all critical breaches.
RESULTS
A total of 256 thoracolumbar pedicle screws were placed in forty patients. Out of which, 6 screws were excluded as fluoroscopy was used in difficult situation. Mean age at the time of surgery was 39 years. Trauma (36) was the most common cause followed by tumor (2) and spondylolisthesis (2) for which pedicle screws were inserted. In total, 250 screws were analyzed for placement accuracy [Table 1 and Figure 3].
| Pedicle number | Number of screws inserted (%) |
|---|---|
| T1 | 4 (1.6) |
| T2 | 2 (0.8) |
| T3 | 4 (1.6) |
| T4 | 4 (1.6) |
| T5 | 4 (1.6) |
| T6 | 6 (2.4) |
| T7 | 4 (1.6) |
| T8 | 8 (3.2) |
| T9 | 16 (6.4) |
| T10 | 28 (11.2) |
| T11 | 36 (14.4) |
| T12 | 36 (14.4) |
| L1 | 28 (11.2) |
| L2 | 32 (12.8) |
| L3 | 20 (8) |
| L4 | 12 (4.8) |
| L5 | 6 (2.4) |
| Total | 250 (100) |
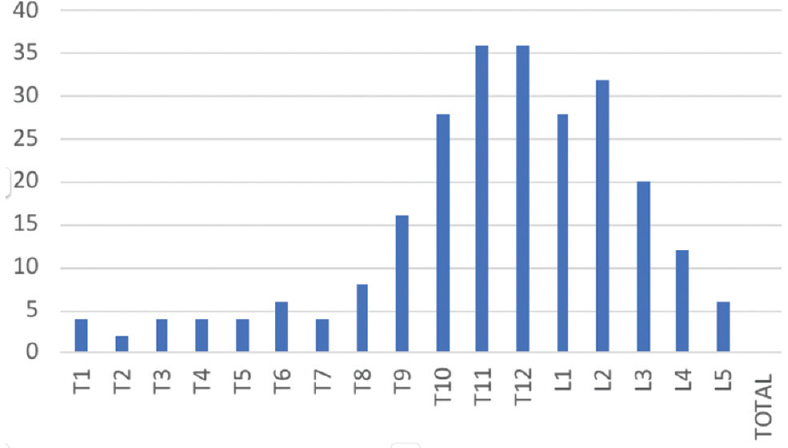
- Bar diagram showing pedicle screws distribution from T1 to L5
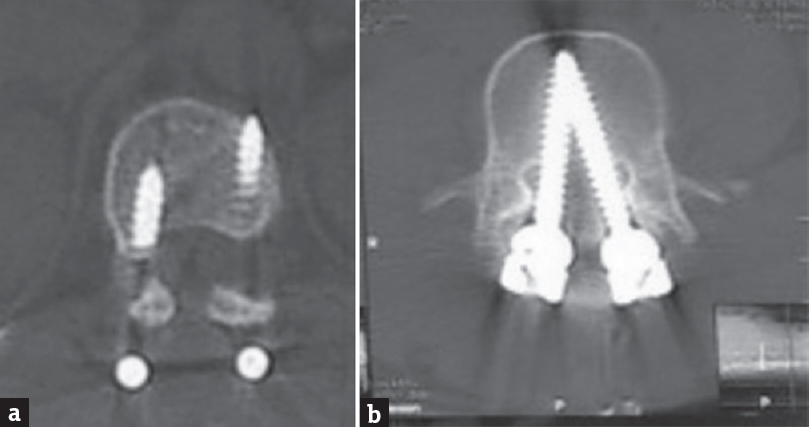
Totally 10 out of 250 screws (4%) were found to breach the pedicle or the vertebral body cortex on postoperative CT evaluation. These breaches occurred in 8 out of 40 patients (20%). The breach incidence was significantly more frequent for thoracic pedicle (7 screws) than in lumbar pedicle (3 screws). Considering the direction of breach, 3 were medial, 4 were lateral, and 3 were anterior. The breaches were further classified as critical and noncritical depending on the length of displacement of the screw. A pedicle breach >4 mm in any direction was considered as critical because of their close proximity to vital structures. Two patients with suboptimal placement of the screw were advised revision surgery to correct the malpositioned screw [Table 2 and Figures 4, 5].
| Pedicle number | Screws Inserted | Number of breaches | Percentage | Medial | Lateral | Anterior |
|---|---|---|---|---|---|---|
| T1 | 4 | 0 | 0 | 0 | 0 | 0 |
| T2 | 2 | 0 | 0 | 0 | 0 | 0 |
| T3 | 4 | 0 | 0 | 0 | 0 | 0 |
| T4 | 4 | 0 | 0 | 0 | 0 | 0 |
| T5 | 4 | 1 | 10 | 1 (noncritical) | 0 | 0 |
| T6 | 6 | 0 | 0 | 0 | 0 | 0 |
| T7 | 4 | 0 | 0 | 0 | 0 | 0 |
| T8 | 8 | 0 | 0 | 0 | 0 | 0 |
| T9 | 16 | 0 | 0 | 0 | 0 | 0 |
| T10 | 28 | 4 | 40 | 0 | 2 (noncritical) | 2 (noncritical) |
| T11 | 36 | 1 | 10 | 0 | 1 (noncritical) | 0 |
| T12 | 36 | 1 | 10 | 0 | 0 | 1 (noncritical) |
| L1 | 28 | 0 | 0 | 0 | 0 | |
| L2 | 32 | 1 | 0 | 0 | 1 (critical) | 0 |
| L3 | 20 | 0 | 0 | 0 | 0 | 0 |
| L4 | 12 | 2 | 20 | 2 (critical) | 0 | 0 |
| L5 | 6 | 0 | 0 | 0 | 0 | 0 |
| Total | 250 | 10 | 100 | 3 | 4 | 3 |
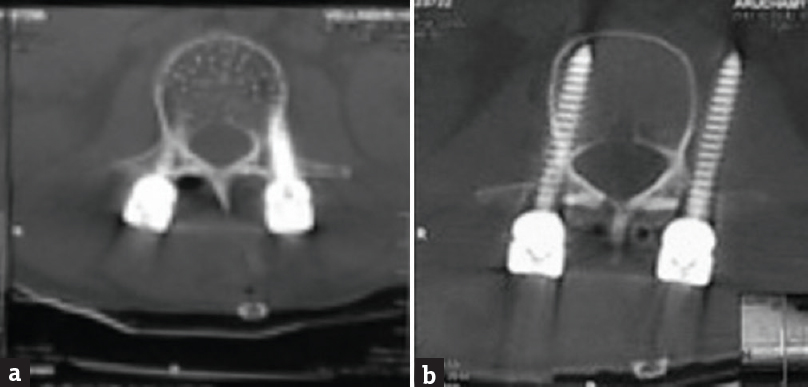
- (a) Noncritical lateral breach. (b) Critical lateral breach
- (a) Noncritical anterior breach. (b) Critical medial breach
DISCUSSION
Posterior spine stabilization with the pedicle screws had seen a great change in technique and accuracy over the past decades. If entire screw remained within the cortices of each respective pedicle, it was considered as accurately placed. Trauma was the most common reason for which pedicle screws were used. The maximum number of screws were inserted in the lower dorsal spine. The thoracolumbar junction was one of the most common sites affected by trauma.[7]
Based on the postoperative follow-up CT scans in 40 patients, 4% incidence of cortical breach was noted in our study which occurred in 8 patients. The incidence of breach was significantly higher in the thoracic pedicle (2.8%) than in the lumbar pedicle (1.2%). High number of traumatic fractures at lower dorsal and thin pedicle size of the dorsal spine may be the reason for this. Rate of malpositioning of pedicle screw ranged from 1.2% to 28.8% in different series. Malpositioned screws diminish the potential strength of the construct. The presence of thicker cortical wall on the medial side of the pedicle and the surgeon's tendency to keep pedicle probe laterally to avoid spinal cord injury due to medial violation results in higher number of lateral pedicle breaches. Parker et al.[6] noted that breaches in thoracic spine (2.5%) were common than in the lumbar spine (0.9%) and were more often in the lateral direction (61.3%) than in the medial (32.8%) or superior (2.5%) direction. Although CT is the most accurate investigation in detecting the breach, its sensitivity varies from 76% to 86% and specificity 75% to 88%.[89] Inferior wall violations are the most difficult to detect on CT scans.[8]
Rampersaud et al.[10] reported that spine surgeons were exposed to 10–12 times more radiation during fluoroscopically assisted pedicle screw insertion. This is primarily due to increased energy required to fluoroscopically image the thoracolumbar spine. Most of the spine surgeons were exposed to radiation above the limit of the permissible whole-body dose of 5000 mrem per year considering the levels of radiation exposure documented in this study. The current guidelines recommend continuous monitoring for whom the radiation exposure is >10% of the maximum permissible annual whole-body dose.[1011]
In the study conducted by Kim et al.[12] (2004) for the safety of freehand pedicle screw placement, they had a 6.2% of moderate cortical perforation (2–4 mm) as compared to 2.8% in our study and 1.7% critical medial wall perforation which was less (1.2%) in our study.
Fisher et al.[13] (2006) evaluated accuracy and safety of pedicle screw placement in the treatment of unstable thoracic spine fractures in which 201 pedicle screws were inserted in 23 patients from T1 to T12. Postoperative CT scan analysis confirmed that 133 (66.20%) screws were fully contained, and the remaining 68 (33.8%) screws violated the pedicle wall inclusive of critical and noncritical breaches.
The acceptable degree of pedicle breach in various directions is still controversial as it has varied in different studies. Gertzbein and Robbins[14] believed that the “safe zone” for allowable medial breach was 4 mm in relation to the intradural contents [Table 3]. From CT myelogram performed, they demonstrated that 2 mm of the epidural space with 2 mm of subarachnoid space existed from T10 to L4 level. They reported that 81% of their screws were placed within 2 mm of medial border of pedicle and 6% had 4–8 mm of canal encroachment, out of which 2 of them developed temporary neurological deficit. Belmont et al.[15] (2002) were of the opinion that acceptable limit was 2 mm for medial wall breach and 6 mm for lateral wall breach. In our study, we considered that 4 mm is the safest limit in all directions including anterior vertebral cortex because vital structures lie beyond this distance.[16]
| Grade | Breach distance (mm) |
|---|---|
| 0 | 0 (no breach) |
| 1 | <2 |
| 2 | 2-4 |
| 3 | >4 |
Aorta is at the risk of iatrogenic injury due to significant anterior cortex breach, one of the major life-threatening complications in thoracic than lumbar vertebrae particularly when spine is deformed. According to Vaccaro et al.[16] anterior cortical breach that occurs in thoracic spine while inserting the right side pedicle screw injures the azygos vein, inferior vena cava or segmental vessels whereas descending aorta or segmental vessels injury occurs on left-sided anterior cortical breach. These structures are often found at a distance of 4-5 mm from anterior vertebral cortex.
Our results with <2% of critical breach document that it is possible to place thoracolumbar pedicle screw accurately in safe manner without the use of other intraoperative methods/devices. We emphasize that everyone should master the skills of intraoperative assistance which may sometime be the only bailout procedure available at times of need. Surgeons must use their best judgment skills to create the safest environment while placing the pedicle screws.
The major limitation associated with the insertion of thoracic pedicle screws is a potential risk of damage to neurovascular structures. The freehand technique of pedicle screw insertion, when performed in a stepwise and consistent sequential manner is an accurate, safe and reliable method with fewer complications.
CONCLUSION
Pedicle screw had become the workhorse for posterior stabilization of the spine. Various technique such as fluoroscopy and navigation are available to place the pedicle screws in more accurate manner. These assisted techniques could be more useful in the mid-thoracic and in the deformed spine. However, selection of a technique should be individualized according to the merit of the case and surgeon's expertise. With the help of anatomical landmarks alone, freehand insertion of pedicle screws can be carried out with acceptable safety and efficacy avoiding cumulative radiation exposure and prolonged operative time. The freehand pedicle screw insertion would be very useful in rural practice where often fluoroscopy could be a luxury.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Plating of thoracic, thoracolumbar, and lumbar injuries with pedicle screw plates. Orthop Clin North Am. 1986;17:147-59.
- [Google Scholar]
- Stereotactic navigation for placement of pedicle screws in the thoracic spine. Neurosurgery. 2001;48:771-8.
- [Google Scholar]
- Computer-assisted fluoroscopic navigation of pedicle screw insertion: An in vivo feasibility study. Acta Orthop Scand. 2004;75:730-5.
- [Google Scholar]
- Comparative results between conventional and computer-assisted pedicle screw installation in the thoracic, lumbar, and sacral spine. Spine (Phila Pa 1976). 2000;25:606-14.
- [Google Scholar]
- Accuracy of free-hand pedicle screws in the thoracic and lumbar spine: Analysis of 6816 consecutive screws. Neurosurgery. 2011;68:170-8.
- [Google Scholar]
- Incidence of clinically diagnosed vertebral fractures: A population-based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res. 1992;7:221-7.
- [Google Scholar]
- Accuracy of computed tomography in assessing thoracic pedicle screw malposition. J Spinal Disord Tech. 2004;17:367-71.
- [Google Scholar]
- Comparison of computerized tomography and direct visualization in thoracic pedicle screw placement. J Neurosurg. 2002;97:223-6.
- [Google Scholar]
- Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine (Phila Pa 1976). 2000;25:2637-45.
- [Google Scholar]
- Advanced image guidance for the placement of thoracic pedicle screws. Sem Spine Surg. 2002;14:58-65.
- [Google Scholar]
- Free hand pedicle screw placement in the thoracic spine: Is it safe? Spine (Phila Pa 1976). 2004;29:333-42.
- [Google Scholar]
- Accuracy and safety of pedicle screw fixation in thoracic spine trauma. J Neurosurg Spine. 2006;5:520-6.
- [Google Scholar]
- Accuracy of pedicular screw placement in vivo . Spine (Phila Pa 1976). 1990;15:11-4.
- [Google Scholar]
- Accuracy of thoracic pedicle screws in patients with and without coronal plane spinal deformities. Spine (Phila Pa 1976). 2002;27:1558-66.
- [Google Scholar]
- Placement of pedicle screws in the thoracic spine. Part II: An anatomical and radiographic assessment. J Bone Joint Surg Am. 1995;77:1200-6.
- [Google Scholar]






