Translate this page into:
Intracranial Rosai Dorfman disease
Address for correspondence: Dr. T. M. Anoop, Department of Medical Oncology, Regional Cancer Centre, Thiruvananthapuram, Kerala - 695 011, India. E-mail: dranooptm@yahoo.co.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 30-year-old man presented with gradual loss of vision, headache and behavioral changes since 1 year. The patient had left temporal hemianopia initially and later developed complete loss of vision and bilateral optic atrophy. No lymph nodes were palpable. Systemic examination revealed unilateral pleural effusion.
Magnetic resonance imaging (MRI) of the brain showed a dural-based lesion seen in the frontal region involving the anterior half of the sagittal sinus with calcification [Figure 1]. The patient underwent bifrontal craniotomy with excision of tumor with sinus and falx. Postoperatively, he developed extradural hematoma formation. A limited parietal craniotomy and hematoma evacuation was performed. Postoperative MRI showed residual lesion of size 6.5 cm × 6 cm × 4.4 cm attached to the falx. Histopathologically, the lesion was composed of sheets of large foamy histiocytes admixed with lymphoplasmacytic cells. Emperipolesis was noted. Immunohistochemistry was positive for S100 and Kp-1 + and negative for LCA, CD 1a, CD5, C Kit and MIB 10%. A diagnosis of non-Langerhans cell histiocytosis–Rosai Dorfman disease (RDD) was considered. Computed tomography (CT) of the chest showed collapse consolidation of right lung with multiple pulmonary nodules on both lungs. Bone marrow examination and immunoglobulin assay were normal.
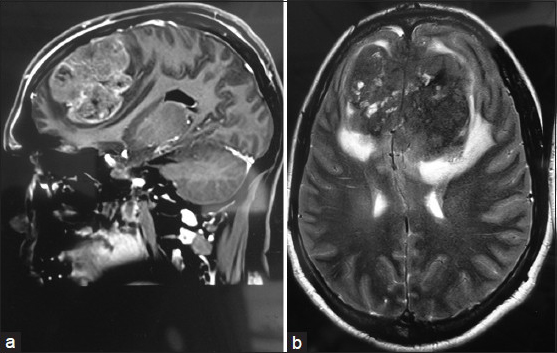
- (a-b) Magnetic resonance imaging of the brain of an intracranial Rosai Dorfman disease patient showing a dural-based lesion seen in the frontal region involving the anterior half of the sagittal sinus with calcification
The patient responded to oral prednisolone 60 mg/day and was put on steroid maintenance. During his last visit, he had improvement in pleural effusion but no change in vision.
Sinus histiocytosis with massive lymphadenopathy, also known as RDD, is a rare histiocytic proliferative disorder of unknown etiology. It usually presents with painless cervical lymphadenopathy with or without extranodal manifestations.[1]
Intracranial involvement of this disease is extremely rare,[2] and intracranial involvement with bilateral optic atrophy is rather rare. The most common imaging appearance of intracranial RDD is a dural-based enhancing mass, mimicking a meningioma. The MRI characteristics of this intracranial dura-based space-occupying lesion are very similar to that of meningioma.
The differential diagnosis of the imaging findings includes meningioma, eosinophilic granuloma, lymphoproliferative disorder, plasma cell granuloma and dural-based metastasis.
Hui Zhu et al. described similar imaging features of the central nervous system (CNS) in RDD, like an extraaxial, well-circumscribed, dura-based mass, isodense or hyperdense on CT, isointensity on T1-weighted imaging and isointensity with hypointensity on T2-weighted imaging. Typical representation of hypointensity within isointensity on T2-weighted or FLAIR image can suggest the diagnosis of RDD.
Histopathology is essential for diagnosis, and when total removal is achieved, the outcome is generally good. Involvement of the CNS in RDD appears to have a good prognosis, particularly in the absence of nodal disease. In a review of follow-up data of 43 patients with RDD, most patients (58%) were alive with disease.[2] Only two patients (4.7%) had died. No death was reported as a result of isolated intracranial RDD.[3]
Various treatment modalities such as surgery, steroids, chemotherapy and radiation therapy have been tried. Surgical resection has been found to be most effective.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Sinus histiocytosis with massive lymphadenopathy: A newly recognized benign clinicopathological entity. Arch Pathol. 1969;87:63-70.
- [Google Scholar]
- Rosai- Dorfman disease isolated to the central nervous system: A report of 11 cases. Mod Pathol. 2001;14:172-8.
- [Google Scholar]
- Isolated intracranial Rosai-Dorfman disease (sinus histiocytosis with massive lymphadenopathy) AJNR Am J Neuroradiol. 2003;24:515-8.
- [Google Scholar]





