Translate this page into:
Intracranial Hemorrhage in a Young Woman: An Unusual Initial Presentation of Undiagnosed Choriocarcinoma
Address for correspondence: Dr. S. K. Jain, Department of Neurosurgery, SMS Medical College, Jaipur - 302 004, Rajasthan, India. E-mail: shashi_neelu@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Choriocarcinoma is an uncommon tumor. Undiagnosed choriocarcinoma initially presenting with intracranial hemorrhage in an apparently healthy female is rare and presents a diagnostic difficulty. The authors report a case presenting as intracranial hemorrhage of unsuspected choriocarcinoma. As the measurement of beta-human chorionic gonadotropin (β-hCG) would have helped in the preoperative diagnosis, estimation of serum β-hCG levels is suggested in the diagnostic workup of a female of reproductive age group when radiological investigations are inconclusive. Craniotomy and excision of tumor followed by chemotherapy and radiotherapy may improve the outcome.
Keywords
Beta-human chorionic gonadotropin
choriocarcinoma
initially presenting
intracranial hemorrhage
INTRODUCTION
Choriocarcinoma is a tumor of trophoblastic tissue, which usually follows molar pregnancy and less commonly term pregnancy, ectopic pregnancy, or spontaneous abortion.[1] It metastasizes to lung, liver, and, less frequently, brain.[2] Intracerebral hemorrhage (ICH) as an initial manifestation in an apparently healthy female is a rare presentation and presents a diagnostic difficulty.[13] The authors present the case summary of an adult female who presented with intracranial hemorrhage. Clinical history and initial investigations were inconclusive regarding the etiology of hemorrhage.
CASE REPORT
A 32-year-old female had sudden-onset severe headache associated with vomiting. The patient was admitted in the emergency department. On admission, computed tomography (CT) brain was performed, which revealed a hemorrhagic lesion in the right parieto-occipital region [Figure 1a]. The patient was then referred to the neurosurgery department for further management.
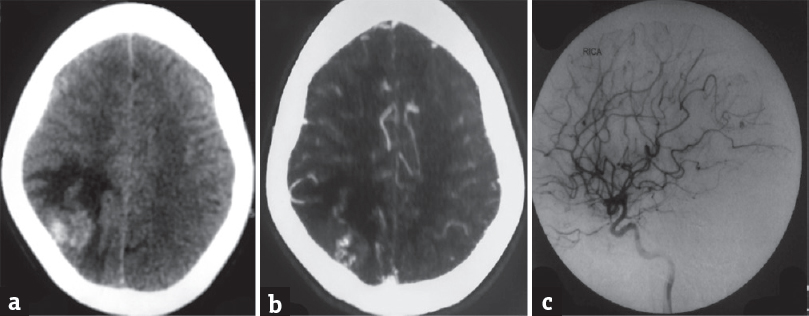
- Noncontrast computed tomography showed a heterogeneously hyperdense lesion in the right parieto-occipital lobe with surrounding edema (a). Computed tomography angiogram showed slight heterogeneous enhancement with few vascular channels within the lesion (b). Digital subtraction angiography brain showed mild blush in the right parieto-occipital region and no evidence of aneurysm or arteriovenous malformation (c)
On admission to the neurosurgery unit, the patient's Glasgow Coma Scale score was 15/15, and the patient had no neurological deficit. The patient was married and had two children. The patient had a medical termination of pregnancy 2 years back. At the time of admission, the patient's last menstrual period was 15 days back. No other significant history was present. Chest X-ray revealed no abnormality. Ultrasonography (USG) abdomen revealed chronic calculus cholecystitis. No other abnormality was detected on abdominal USG. Antiepileptics and antiedema measures were started.
On the basis of clinical presentation and CT brain findings, a working diagnosis of the vascular lesion was made. A CT angiogram brain was performed, which did not reveal any vascular etiology [Figure 1b]. Cerebral digital subtraction angiography (DSA) was then performed, which did not show any arteriovenous malformation (AVM) or aneurysm [Figure 1c]. A contrast magnetic resonance imaging (MRI) brain with MR spectroscopy (MRS) was performed, which revealed a hemorrhagic lesion [Figure 2a]. MRS findings were inconclusive possibly due to hemorrhage [Figure 2b]. No abnormality was detected on contrast-enhanced CT (CECT) abdomen and chest.
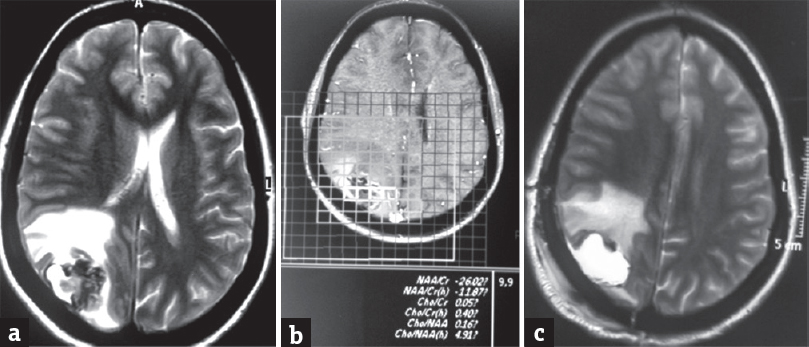
- Preoperative T2 magnetic resonance imaging brain revealed a lesion in the right parieto-occipital lobe, which is hypointense with peripheral hyperintensity on T1, heterogeneously hypointense on T2 and fluid-attenuated inversion recovery, blooming on Fast Field Echo imaging and patchy peripheral restriction on diffusion-weighted imaging, suggestive of hemorrhage (a). Magnetic resonance spectroscopy revealed reduced peak of all metabolites in the region of the lesion (b). T2 magnetic resonance imaging brain postoperative showed postoperative changes and some residual tumor (c)
A craniotomy was planned with the aim of achieving a tissue-based diagnosis and gross total excision of the lesion. The craniotomy was performed, which revealed a superficial cortical lesion with areas of hemorrhage. No feeding vessels or unexpected hemorrhage were encountered during the procedure. Gross total excision of the hemorrhagic lesion was performed. The patient had uneventful intraoperative and postoperative course. Postoperative contrast MRI was performed, which showed some residual tumor [Figure 2c].
Histopathological examination and immunohistochemistry revealed choriocarcinoma [Figure 3]. Serum beta-human chorionic gonadotropin (β-hCG) level was estimated on postoperative day 4, which was found to be highly elevated [Table 1]. The case was discussed in the institute's tumor board meeting regarding further management, and chemotherapy was started. The patient received cisplatin, etoposide, and bleomycin combination chemotherapy and whole-brain radiotherapy. The patient is without any neurological deficit at 4-month follow-up, with serum β-hCG values within reference interval [Table 1].
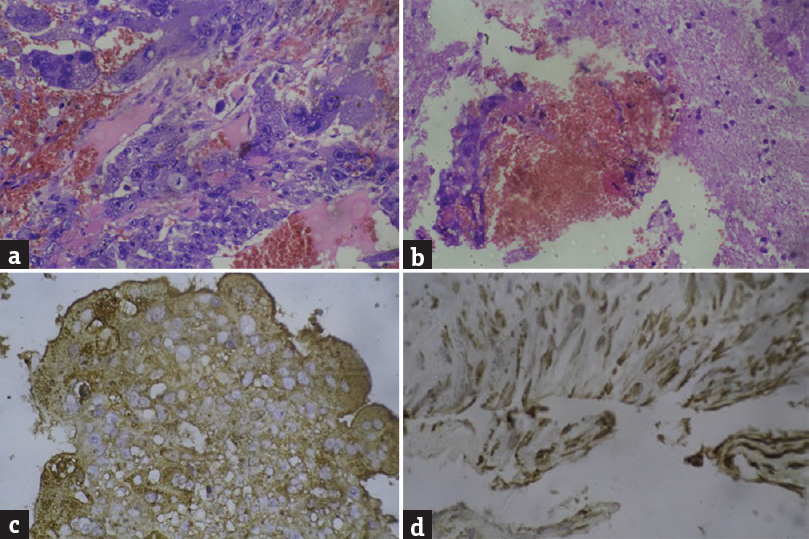
- Histopathological examination (H and E, ×20) showed malignant trophoblasts and syncytiotrophoblasts with areas of hemorrhage and brain tissue (a and b). Immunohistochemistry for beta-human chorionic gonadotropin (×40) showed diffuse and strong positivity in malignant cells (c). The proliferative index is markedly increased with Ki-67 (×100) in approximately 80%–90% of tumor cells (d)
| Time after surgery | Level in mIU/ml |
|---|---|
| At postoperative day 04 | 243538.9 |
| At four months follow up | 2.2 |
DISCUSSION
Diagnostic workup of a nontraumatic hemorrhage is a frequently performed exercise in neurosurgical practice. Stroke, aneurysm, AVM, and tumoral hemorrhages commonly present with nontraumatic ICH. In a published case report of choriocarcinoma, the authors emphasized the difficulty encountered in making a diagnosis in cases with intracranial hemorrhagic metastasis.[3] In the present case, CECT, MRI, and DSA ruled out aneurysm, AVM, and cortical venous thrombosis, which are possible common causes in a young woman, but failed to suggest an etiological diagnosis.
In a study from India, Suresh et al. reported ten cases of unsuspecting choriocarcinoma metastasizing to brain.[4] In agreement with this study, accurate diagnosis can only be made after resection of blood clots. This highlights the necessity for craniotomy and subsequent submission of specimen (blood clots) for histopathological examination. Suction evacuation should not be used in the removal of ICH in cases when tumor hemorrhage is suspected as it may lead to loss of tumor tissue.
β-hCG levels are known to have diagnostic as well as prognostic value.[1] In the present case, clinical history, chest X-ray, and USG abdomen study did not raise suspicion for primary malignancy. In the authors’ opinion, routine use of β-hCG in the diagnostic algorithm in cases of ICH is not recommended. However, in a young woman of reproductive age group, β-hCG estimation may be beneficial, especially when other common causes are excluded based on the clinical history and other investigations or tumor hemorrhage is suspected.
Choriocarcinoma is an aggressive but chemosensitive tumor, which may present as brain metastasis. Cerebral metastasis is considered a poor prognostic factor and combination chemotherapy is advocated.[5] In a study, Xiao et al. presented a single-institute experience in the management of patients with brain metastasis from gestational trophoblastic neoplasia. In their study, on univariate analysis, craniotomy was a favorable prognostic factor.[6]
CONCLUSION
Choricarcinoma is a rare tumor and initial presentation as intracranial hemorrhage presents a diagnostic difficulty. Serum β-hCG estimation may help in preoperative diagnosis in reproductive age group females. Suction should not be used for the removal of ICH when tumor hemorrhage is suspected. Craniotomy followed by chemotherapy and radiotherapy may improve outcome in a patient with brain metastasis of choriocarcinoma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Unusual clinical presentations of choriocarcinoma: A systematic review of case reports. Taiwan J Obstet Gynecol. 2017;56:1-8.
- [Google Scholar]
- Spontaneous intracerebral haemorrhage as initial presentation of gestational choriocarcinoma in a young woman: A case report and review of literature. Internet J Pathol. 2009;10:2.
- [Google Scholar]
- Metastatic choriocarcinoma presenting as multiple intracerebral haemorrhages: The role of imaging in the elucidation of the pathology. J Neurol Neurosurg Psychiatry. 1998;65:939-41.
- [Google Scholar]
- Intracranial haemorrhage resulting from unsuspected choriocarcinoma metastasis. Neurol India. 2001;49:231-6.
- [Google Scholar]
- Choriocarcinoma with brain, lung and vaginal metastases successfully treated without brain radiation or intrathecal chemotherapy: A case report. Gynecol Oncol Rep. 2017;20:97-9.
- [Google Scholar]
- Management and prognosis of patients with brain metastasis from gestational trophoblastic neoplasia: A 24-year experience in Peking Union medical college hospital. BMC Cancer. 2015;15:318.
- [Google Scholar]






