Translate this page into:
Intracranial hemorrhage in a patient coinfected with dengue and leptospirosis
Address for correspondence: Dr. Tanmoy Ghatak, Rammohan Pally, Arambagh Hooghly, West Bengal - 712 601, India. E-mail: tanmoyghatak@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
The incidence of coinfection with leptospirosis and dengue is increasingly being reported.[1] But, intracranial hemorrhage (ICH) has never been reported in such coinfections, though neurological manifestations and even ICH are reported independently in dengue and leptospirosis.[234] We report a case of a young male having coinfection with severe dengue and leptospirosis who developed ICH in the course of disease.
A 40-year-old male was admitted to our intensive care unit (ICU) with history of high grade continuous fever and generalized body ache since 5 days along with hematochezia and oliguria for 1 day. He was nonalcoholic and previous medical records and history was not suggestive of diabetes or hypertension. On admission, patient was conscious (Glasgow coma scale 14/15), pale and icteric. He had a heart rate of 120 beats/min, blood pressure of 106/70 mmHg, and respiratory rate of 34 breaths/min. Petechial lesions were present on lower limbs. Investigations revealed hematocrit of 39%, platelets 38,000/mm3, with deranged renal (creatinine 6.2 mg/dl, urea 108 mg/dl), and hepatic function (total bilirubin 8.2 mg/dl, ALT 342 IU, AST 230 IU). Dengue NS1 antigen test was positive. Patient's respiratory and hemodynamic status deteriorated within few hours of admission and he required tracheal intubation, dialysis, vasopressor support, and mechanical ventilation. Although the blood, tracheal aspirates, and urine cultures were sterile, empirical antibiotics (initially beta lactams with beta lactamase inhibitors and then carbapenems) had to be initiated due to the continuously high procalcitonin levels (maximum 12 ng/dl) and rapidly worsening clinical condition. Multiple blood and blood product transfusions were required to stabilize the hematocrit and correct the ongoing bleeding. Within first 3 days, his hemodynamics, liver and renal functions started improving along with reduced vasopressor requirements. In the meantime, leptospira IgM ELISA (LeptoTek DriDot, Organon Teknika, Netherlands) was also found to be positive. However, during the observation period following cessation of sedation, the patient was found unresponsive to painful stimulus. His pupils were bilaterally constricted and reacted very sluggishly to light. After ruling out metabolic causes, we injected intravenous naloxone to reverse the cumulative narcosis by fentanyl (9 mg infused over last 72 h). Following which, we observed that on painful stimulus, there was deviation of the angle of mouth toward right and his left pupil was 4.0 mm sluggishly reacting to light while the right pupil was 3 mm and reacting. In the background of the existing coagulopathy, we suspected ICH as the probable diagnosis. Aggressive cerebroprotective measures like head up, hypertonic saline, hyperventilation was initiated and sedation was restarted. An urgent magnetic resonance imaging (MRI) head revealed a left frontoparietal hematoma of size 2 × 2 cm with mild perilesional edema with no midline shift [Figure 1]. There was no evidence of any basal or sulcal exudates. MRI arteriogram showed no vascular anomaly or aneurysmal rupture. Both neurological and neurosurgical opinion was in favor of conservative management.
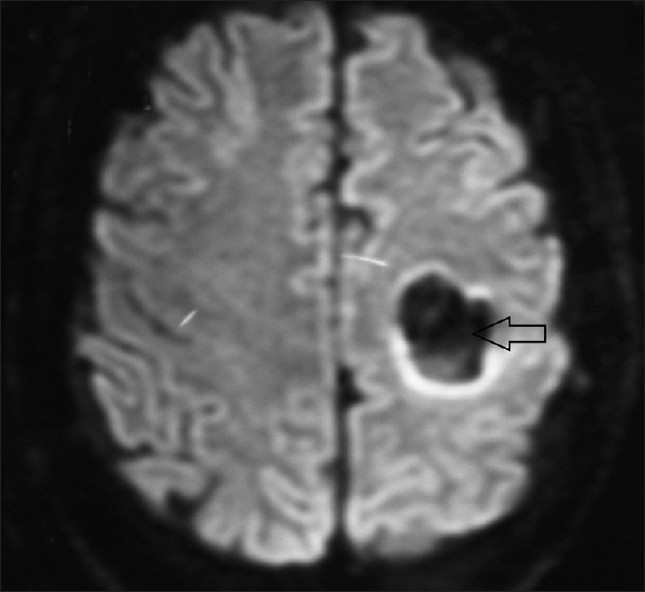
- Magnetic resonance imaging head showing left frontoparietal hematoma (arrowed) with mild perilesional edema without midline shift
Tracheostomy was performed in view of long-term ventilation. He, however, developed ventilator-associated pneumonia and his septic shock worsened. Despite the optimal organ supportive measures his multi-organ dysfunction continued to worsen and he succumbed to the illness after 10 days of ICU stay.
Hypertension and amyloid angiopathy are the common causes of ICH apart from ruptured vascular aneurysm and coagulopathy.[5] Spontaneous ICH with coinfection may be due to thrombocytopenia, liver dysfunction, and cerebral arteritis caused by the leptospira.[67] Severe leptospirosis can cause generalized endothelial dysfunction due to release of proinflammatory cytokines.[7] Interestingly, antibody against dengue virion also acts on the endothelium and as a result causes destruction of hemostatic system.[8] Endothelial dysfunction initiates bleeding manifestation especially with thrombocytopenia or platelet functional abnormalities.[9]
To our knowledge, this is the first reported case of ICH in severe dengue and leptospira coinfection. Delayed emergence in our case is not only due to anesthetic agent's overdose, but also due to an intracerebral event like ICH in the background of coinfection. We feel, in our case, cerebral blood vessel arteritis by leptospira and endothelial dysfunction due to synergistic action of both the organisms are responsible for spontaneous ICH. In our case, we agree, a number of other factors like liver dysfunction, thrombocytopenia as well as platelet functional abnormality could also have played a role.
This case tells about the importance of bedside pupillary examination and awake, responding to verbal commands, responding to pain, unresponsive charting during reversal of narcosis and in patients with delayed emergence (>24 h). It should be noted that as severe coinfection like dengue and leptospirosis can increase a chance of ICH together by targeting endothelium, so, any sensorium deterioration with disease severity should be diligently investigated.
References
- Leptospirosis: Experience of a tertiary care hospital in northern India. Natl Med J India. 2011;24:78-80.
- [Google Scholar]
- Skin rash, headache and abnormal behavior: Unusual presentation of intracranial haemorrhage in dengue fever. BMJ Case Rep 2010 2010:pii. bcr06.2009.1949
- [Google Scholar]
- Prospective case-control study of encephalopathy in children with dengue hemorrhagic fever. Am J Trop Med Hyg. 2001;65:848-51.
- [Google Scholar]
- Activation of the coagulation cascade in patients with leptospirosis. Clin Infect Dis. 2008;46:254-60.
- [Google Scholar]
- High serum nitric oxide levels in patients with severe leptospirosis. Acta Trop. 2006;100:256-60.
- [Google Scholar]
- Vascular endothelium: The battlefield of dengue viruses. FEMS Immunol Med Microbiol. 2008;53:287-99.
- [Google Scholar]
- Role of the endothelium in viral hemorrhagic fevers. Crit Care Med. 2002;30:S268-73.
- [Google Scholar]





