Translate this page into:
Infratentorial Epidural Abscess Secondary to Furunculosis: Case Report and a Review of the Literature
Address for correspondence: Dr. Ricardo Horacio Menéndez, Department of Neurosciences, Hospital Aleman, Pueyrredon 1640, 1118AAT, Buenos Aires, Argentina. E-mail: rhmenendez@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The authors describe a case of infratentorial epidural abscess caused by community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) in a patient with a recent history of cutaneous furunculosis. This 29-year-old male presented with an occipital headache associated with fever, vomiting, and neck stiffness. Admission magnetic resonance imaging showed a retrocerebellar epidural abscess. Antimicrobial therapy was started, and the patient underwent craniectomy for evacuation of the abscess. Cultures of the surgical specimen were consistent with CA-MRSA. Postoperatively, the patient's condition improved with the resolution of symptoms, and he was discharged home with indication of 6 weeks of antibiotic therapy. Furunculosis is a very rare cause of intracranial epidural abscess but should be considered as a source of infection in an immunocompetent patient.
Keywords
Community-associated methicillin-resistant Staphylococcus aureus
furunculosis
infratentorial epidural abscess
INTRODUCTION
Epidural abscess is an uncommon form of intracranial suppuration and represents about 2% of all intracranial infections. In general, the sources of intracranial suppuration are otogenic infections, paranasal sinusitis, penetrating trauma, or cranial surgery.[12] Whereas the spinal epidural abscess from cutaneous source occurs and has been frequently reported in medical literature,[3] hematogenous spread from cutaneous skin infections to cranial epidural space is extremely rare. To our knowledge, ours is the first case of infratentorial epidural abscess from skin lesions in a previously healthy patient.
CASE REPORT
A 29-year-old male immunocompetent patient was referred to our hospital presenting with progressive headache, fever, and vomiting which he had been suffering for a few days before admission. He denied drug abuse or alcohol. His past medical history was only remarkable for a recent furunculosis on both legs that had been treated with oral clindamycin 3 weeks before surgery. Drainage of the furuncles had not been required.
On initial physical examination, the patient presented with neck stiffness. He had no neurological deficit. Laboratory findings included a white blood cell count of 27,000 cells per mm3, with 81% neutrophils, 7% lymphocytes, and 12% monocytes. The erythrocyte sedimentation rate was 43 mm/hour.
Gadolinium-enhanced T1-weighted images revealed a left retrocerebellar epidural hypointense collection with dural contrast enhancement [Figure 1a]. T2-weighted and diffusion-weighted imaging showed the collection as a high-intensity area [Figure 1b and c]. Magnetic resonance venography revealed left lateral-sinus thrombosis [Figure 1d].
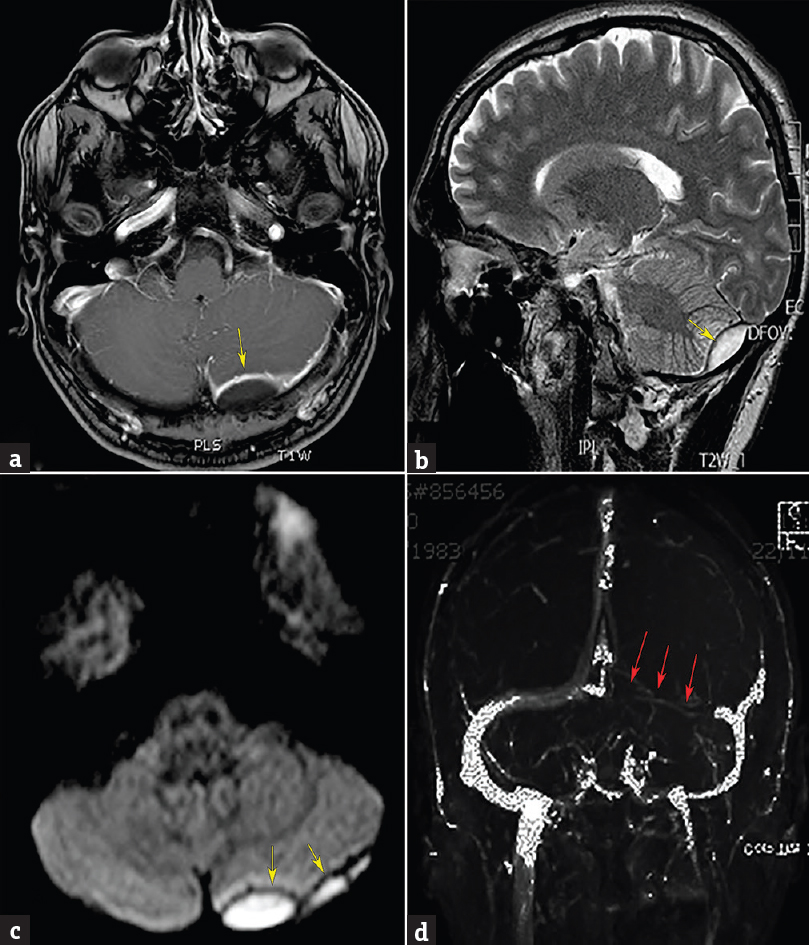
- Admission axial postcontrast T1-weighted magnetic resonance image (a) revealing an enhancing left retrocerebellar epidural abscess. Sagittal T2-weighted (b) and diffusion-weighted (c) images showing the collection as a high-intensity area (yellow arrows). (d) Magnetic resonance venography demonstrating left lateral sinus thrombosis (red arrows)
Computerized tomography (CT) scan showed no evidence of sinusitis or otomastoiditis, and an examination performed by an ear–nose–throat physician was normal. Echocardiogram showed no abnormalities suggestive of endocarditis. A chest CT scan of the patient was normal.
Empiric antibiotic therapy (vancomycin, metronidazole, and ceftriaxone) was initiated, and the patient received surgical treatment. Left suboccipital craniectomy and evacuation of the epidural empyema were performed. Collection of epidural purulent material and exudates were found over the dura mater, with no signs of bone infection. Pus was examined for aerobic and anaerobic bacteria. Cultures of the surgical specimen were consistent with community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA). The strain was sensitive to amikacin, gentamicin, erythromycin, clindamycin, ciprofloxacin, co-trimoxazole, rifampicin, vancomycin, and linezolid and resistant to oxacillin, ampicillin-sulbactam, and cefalotin, with disc diffusion testing. The minimal inhibitory concentration of isolated strain against vancomycin was determined using E-test and was 1 mg/L. After surgery, the treatment was switched to linezolid + rifampicin. The patient had an uneventful postoperative recovery with no neurologic deficits, and his headache and neck stiffness were totally alleviated. A peripherally inserted central catheter line was placed, and the patient was discharged on postoperative day 8 with an indication of 6 more weeks of antibiotic therapy. Thrombosis of the lateral sinus was treated with low-molecular-weight heparin for 6 weeks and then continued with acenocoumarol for 6 months postoperatively. There were no complications related to the anticoagulant therapy. Magnetic resonance imaging (MRI) showed no epidural empyema, and the patient had no evidence of infection or thrombosis for 6 months postoperatively.
DISCUSSION
Intracranial epidural abscess is the third most common focal intracranial infection, apart from the brain abscess and subdural empyema.[4] It takes place in the space between the inner skull table and dura mater. The intracranial dura mater forms the inner lining of the skull and is directly adherent to the bone. Thus, under normal circumstances, there is no actual epidural space. Epidural abscess requires that the firmly adherent dura be dissected off the bone. Organisms usually spread into the potential epidural space by direct extension from a contiguous focus of infection or by inoculation during trauma or neurosurgery.[1] Direct extension of infection from the middle ear by osteomyelitis and erosion of the bone barriers is the most common cause of epidural infratentorial pyogenic collections.[2] Our patient had no previous history of cranial surgery, trauma, or obvious contiguous infection. The cranial bone showed no evidence of osteomyelitis.
CA-MRSA had increased through time as a cause of skin and soft-tissue infections since the early 1990s when the first reports were published.[5] Isolated involvement of the cranial epidural space through the bloodstream from a distant soft-skin infection is extremely rare. We reviewed the cases of CA-MRSA with central nervous system involvement and could find only two reports of nonnosocomial intracranial epidural abscess not from a contiguous source, but from distant soft-tissue infections. Lo et al. reported a CA-MRSA epidural frontal abscess in a 21-year-old female with recent furunculosis and possible endocarditis.[6] Higashiyama et al. reported a case of epidural abscess caused by CA-MRSA in a previously healthy 25-year-old female who had suffered from subcutaneous infection a few weeks earlier.[7] The primary lesion was thought to be the skin lesions in these two cases, and both of them took place in the supratentorial space.
Diagnosis was based on clinical findings, medical imaging, and abscess cultures. MRI accurately demonstrated the extent of infection. Abscess typically exhibited hyperintensity on T2-weighted images, hypointensity on T1-weighted images, and restricted diffusion. Unlike previous reported cases, blood cultures were negative, and the echocardiography did not show signs suggestive of endocarditis.
Successful treatment of an intracranial epidural abscess requires a combination of drainage procedure and antibiotic therapy. Empiric antibiotic therapy should be chosen based on the probable origin of the infection. With CA-MRSA increased frequency, empirical association of an antimicrobial agent with activity against CA-MRSA strains may be necessary in this clinical entities.[89] Typically recommended duration of 4–6 weeks of antibiotic therapy is extended to 8 weeks or longer in the presence of osteomyelitis.[10]
In conclusion, this is the first report of an isolated intracranial epidural abscess involving the posterior fossa, originated not from a contiguous source but from a distant skin infection. Hematogenous spread from skin infections to intracranial epidural space is extremely rare but should be taken into consideration in a patient with a history of furunculosis. This report also highlights an emerging problem of CA-MRSA infections in previously healthy patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors are indebted to Dr. Elisa Estenssoro and Noemi Schneck for English editing of the manuscript.
REFERENCES
- Cranial extradural empyema in the era of computed tomography: A review of 82 cases. Neurosurgery. 1999;44:748-53.
- [Google Scholar]
- Bacterial spinal epidural abscess. Review of 43 cases and literature survey. Medicine (Baltimore). 1992;71:369-85.
- [Google Scholar]
- Brain abscess, subdural empyema, and intracranial epidural abscess. Curr Infect Dis Rep. 1999;1:166-71.
- [Google Scholar]
- A multistrain cluster of methicillin-resistant Staphylococcus aureus based in a native community. Can J Infect Dis. 1990;1:121-6.
- [Google Scholar]
- Missed epidural brain abscess after furunculosis. Am J Emerg Med. 2008;26:522.e3-4.
- [Google Scholar]
- Epidural abscess caused by community-associated methicillin-resistant Staphylococcus aureus strain USA300 in Japan. J Infect Chemother. 2010;16:345-9.
- [Google Scholar]
- Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med. 2005;352:1436-44.
- [Google Scholar]
- A twelve-year review of central nervous system bacterial abscesses; presentation and aetiology. Clin Microbiol Infect. 2003;9:803-9.
- [Google Scholar]
- The surgical management of infections involving the cerebrum. Neurosurgery. 2008;62(Suppl 2):519-30.
- [Google Scholar]






