Translate this page into:
Inadvertent Central Arterial Catheterization: An Unusual Cause of Ischemic Stroke
Address for correspondence: Dr. Nakul Katyal, Department of Neurology, University of Missouri, Columbia, MO, USA. E-mail: Katyal.nakul@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Central venous catheter (CVC) insertion is extensively utilized in Intensive Care Units for evaluation of hemodynamic status, administration of intravenous drugs, and for providing nutritional support in critically ill patients. Unfortunately, CVC use is associated with complications including lung injury, bleeding, infection, and thrombosis. We present a patient with an acute ischemic stroke from an inadvertently placed CVC into the right common carotid artery. A 57-year-old male presented to our institution for left hemiplegia and seizures 2 days after a CVC was placed. He was found to have a right frontal ischemic stroke on computed tomography (CT). CT angiography noted that the catheter was arterial and had a thrombosis around it. He was started on a low-dose heparin infusion. A combination of cardiothoracic surgery and interventional cardiology was required to safely remove the catheter. Central arterial catheterization is an unusual cause for acute ischemic stroke and presents management challenges.
Keywords
Acute ischemic stroke
central venous catheterization
seizure
INTRODUCTION
Central venous catheters (CVC) are used extensively in critically ill patients to provide parenteral nutrition, intravenous drugs, and to monitor hemodynamic status.[1] However, significant complications are known to occur with CVC insertion.[1] These include pneumothorax, hemothorax, local hematoma, vascular injury, thrombosis, embolism, and catheter disruption.[1] Direct arterial injury is a rare complication and occurs in < 1% of catheter insertion.[1] Erroneous arterial catheterization rarely can result in clot formation, neurological deficits, and stroke.[1]
We report a case of ischemic stroke that developed secondary to clot propagation from inadvertently placed emergent CVC into the right common carotid artery. We describe the case and review literature on this unusual cause of ischemic stroke and underlying management of this rare complication associated with central venous line insertion Institutional Board Review approved the submission of this case report.
CASE REPORT
A 57-year-old male was admitted to an outside hospital with S-T elevation myocardial infarction (MI). During his admission at the outside facility, he developed acute hypotension and required emergent central venous access through right subclavian vein for vasopressors. He was stabilized at the outside facility. Two days later, he was noted to have acute left hemiplegia and right gaze deviation. Transfer to our facility as an acute stroke activation was arranged. En route, he had a focal seizure and was intubated for airway protection. In the emergency department, he had a Glasgow coma scale score of 10 (E: 4, V: 1, M: 5). He was opening eyes spontaneously. He had a right gaze deviation. He was localizing the right lower and upper extremities but was plegic on the left hemibody. He had a cluster of seizures and was started on levetiracetam and propofol infusion. Computed tomography (CT) of the head showed loss of gray-white matter differentiation in the right frontal lobe and a right frontal hypodensity [Figure 1a]. CT angiography (CTA) of the head was negative for large vessel occlusion. His CTA of the neck, however, showed a catheter extending from the right side of neck into the right common carotid artery with tip located in the arch of the aorta with the presence of a thrombosis [Figure 1b-d]. He was not eligible for tissue plasminogen activator and/or neurointervention because of recent history of MI and no major intracranial vessel occlusion or thrombosis. Given the catheter-associated thrombosis, the decision was to initiate heparin infusion. Heparin infusion was started at a goal of 1.5–2x patient's baseline partial thromboplastin time. In the neurosciences Intensive Care Unit, the heparin was continued. Cardiothoracic surgery and interventional cardiology were consulted for the removal of catheter. After management options were discussed with family, they chose the interventional endovascular procedure instead of open thoracotomy for removal.
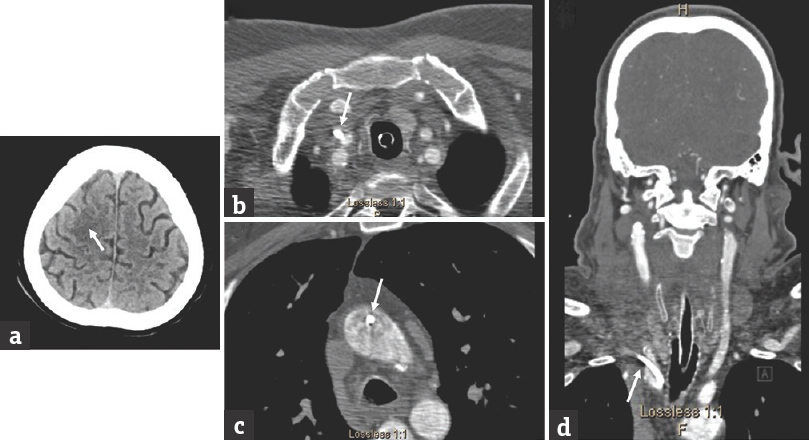
- Computed tomography and computed tomography angiography. A right frontal hypodensity consistent with acute ischemic stroke is seen (a, arrow). Axial computed tomography angiography images show the central arterial catheter entering the right common carotid (b, arrow) and tip in the arch of the aorta (c, arrow). The coronal computed tomography angiography image shows the central arterial catheter in the right common carotid artery (d, arrow)
On poststroke day 5, cardiothoracic surgery and interventional cardiology performed a hybrid endovascular procedure for removal of the central line. Angiographic guidance was used as part of the procedure. Using the femoral access, a pigtail catheter was introduced into the arch of aorta. An arch angiogram was performed, which did not reveal any clot in arch vessels. An incision was made in the right supraclavicular area, which was later extended to the carotid sheath. The right common carotid artery was identified and was carefully encircled with vessel loops. Further dissection occurred to the thoracic inlet where the inadvertently placed catheter was identified in the right common carotid artery at the bifurcation of the right subclavian artery. Circumferential stitches were placed around the right subclavian and common carotid arteries in a horizontal manner. The catheter was removed in a sterile fashion using the endovascular approach. After catheter removal, repeat angiography was negative for contrast extravasation outside of the vascular structures. The patient was continued on heparin infusion postprocedure. Magnetic resonance imaging confirmed the right frontal ischemia without hemorrhagic transformation. Over the next few days, he markedly improved on neurological examination, was extubated, and eventually discharged to rehabilitation center on a combination of aspirin (81 mg) and warfarin (international normalized ratio: goal 2–3) for 30 days and was advised to follow up with outpatient neurology after 4 weeks.
DISCUSSION
Our case highlighted a rare presentation of ischemic stroke occurring due to clot propagation from a subclavian venous catheter that was inadvertently placed into the right common carotid artery extending into the arch of aorta.
Multiple studies have reported the development of clot formation in and around venous catheters.[1] Incidence of thrombus formation varies from 8% to 63% in patients with CVC catheters.[1234] Incidence with arterial catheters is largely unknown. Direct arterial injury occurs in < 1% of catheter insertion and is generally recognized instantaneously due to pulsatile flow of arterial vessel.[567] Recognition can be difficult in critically ill patients with hypotension and/or hypoxia.[567] Hurwitz and Posner reported two patients who developed clinical and pathological evidence of embolic infarction in the left carotid and left vertebral distributions, after inadvertent arterial puncture during attempts to catheterize the left subclavian vein.[8] In addition, prolonged arterial catheterization can result in clot formation, neurological deficits, and stroke, as we have reported.[567]
Studies have reported benefits of using ultrasound-guided line insertion to minimize the risk of arterial injury.[91011] Reuber et al.[12] reported the study of four patients, who developed stroke following carotid artery injury secondary to erroneous internal jugular venous cannulation using landmark technique. Three out of four patients showed the evidence of intimal injury and thrombus formation. In two of the patients, stroke was observed 24 h after initial insult. This study advocated the use of ultrasound-guided line insertion over landmark technique to minimize the risk of arterial injury.[12] A meta-analysis of prospective randomized trials of internal jugular vein and subclavian vein cannulation studies comparing ultrasound-guided and landmark insertion techniques found a decreased risk of placement failure (relative risk: 0.32, 95% confidence interval [CI]: 0.18–0.55%) and complications during catheter placement (relative risk: 0.22, 95% CI: 0.1–0.45%) with the use of ultrasound.[12] However, despite all these techniques, the wire may traverse the vein and enter the artery, which may not be appreciable on ultrasound, particularly if it occurs below the level of the clavicle where visualization with ultrasound is difficult.[13] Landmark technique has been reported to have higher complications and lower success rate as compared to ultrasound-guided technique.[14] Xu and Zhang reported 94% first puncture success rate with subclavian artery landmark-based technique for superior vena cava catheterization.[15] However, this technique had 4% incidence rate of arterial puncture.[15] The landmark-based technique is beneficial in emergency settings requiring instant central line access, as ultrasound-guided placement can be time-consuming. In addition, the use of subclavian venous central access has a lower infection risk compared to other central sites.[16] Analysis of pressure waveform and/or gravitational flow using pressure transduction can effectively confirm the venous placement of CVC and has shown to reduce incidences of inadvertent arterial cannulation.[1317] Similarly, analysis of arterial blood gas from aspirated blood may provide confirmation arterial catheterization if both pO2 and SpO2 are high.[1318] Postprocedure chest X-ray further verifies venous placement.
The two most commonly employed techniques for removal of misplaced CVC are mechanical removal of catheter and application of direct pressure and surgical exploration, repair, and catheter removal.[19] A retrospective study of 11 patients with inadvertent arterial catheterization compared utility of both these techniques.[19] Two out of 11 patients were managed with mechanical pulling of catheter followed by direct pressure application, whereas in the remaining nine patients, catheter was removed by surgical exploration.[19] Of the two patients treated with mechanical pulling, one patient developed pseudoaneurysm whereas another patient developed stroke after pulling out catheter.[19] No new complications were observed in patients who were managed surgically.[19] In eight out of nine patients managed surgically, surgery was performed within 3 h of diagnosis.[19] Surgery was delayed in one patient by 12 h after diagnosis.[19] This study concluded that surgical management was the most effective and safest treatment option for removal of misplaced arterial catheters.[19] The insertion site in our patient was behind the clavicular head preventing us from being able to apply mechanical pressure.
Mechanical pulling of catheter may be beneficial in patients who are not on anticoagulation and in conditions where artery is accessible for manual compression.[19] Manual compression is common after endovascular procedures. Distal common carotid artery may be accessible to manual compression against the vertebral column, but the overlying bony structure precludes effective external pressure to tamponade the vessels proximally such as innominate artery and subclavian artery.[19] Surgical management is generally beneficial in such circumstances.[19] Brown reported a case where a misplaced arterial catheter was removed using surgical approach.[20] Angiogram showed significant clot formation around catheter.[20] A 10 g thrombus and catheter were removed surgically >72 h after insertion.[20]
Anticoagulation remains a challenging issue in managing patients with central line thrombosis in setting of an acute ischemic stroke given the high risk of hemorrhagic conversion in these patients.[21] However, anticoagulation may be necessary in preventing further clot propagation, thus benefits outweigh the associated risk in such circumstances. Choice of anticoagulation can be challenging. The Warfarin–Aspirin Symptomatic Intracranial Study trial compared the efficacy of warfarin versus aspirin in patients with angiographically documented 50% intracranial stenosis.[21] Warfarin was found to be associated with significantly higher rates of adverse events and provided no benefit over aspirin.[21] The Warfarin–Aspirin Recurrent Stroke Study compared the efficacy of warfarin with aspirin for the prevention of recurrent ischemic stroke among 2206 patients with a noncardioembolic stroke.[21] No significant differences were seen between the two treatment groups for prevention of recurrent stroke or death (warfarin, 17.8% and aspirin, 16.0%).[21] The use of anticoagulation in acute ischemic stroke has largely been abandoned.
The American College of Chest Physicians (ACCP) recommends 3–5 days of anticoagulation therapy before removal of a catheter in patients who have developed a catheter-related thrombosis and no longer require a central access.[2223242526] The length of time a patient should be anticoagulated following removal of the CVC is debatable.[2223242526] Some physicians advocate anticoagulation for 3 months after catheter removal, while others suggest shortened course depending on the patient and the severity of the clot.[2223242526] For patients with catheter-related thrombosis who continue to require central venous access, the catheter can be left in place and anticoagulation therapy initiated.[2223242526] Current recommendations include initial anticoagulation for several days, with unfractionated heparin or low molecular weight heparin, followed by at least 3 months of anticoagulation with a Vitamin K antagonist or low molecular weight heparin.[2223242526] ACCP recommends continued anticoagulation therapy at a prophylactic dose until the catheter is removed.[2223242526] This recommendation must be individualized in patients with acute ischemic stroke and risk for hemorrhagic transformation of the infarcted brain.
CONCLUSION
Our case highlights a rare presentation of ischemic stroke from an inadvertently placed subclavian venous catheter into the right common carotid artery. We also discuss the management of this complication. Management required an individualized approach including the use of low-dose heparin infusion and surgical removal of the central arterial catheter. Ultrasound-guided central line insertion and/or confirmation with transduction may significantly minimize the risk of arterial injury.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Central venous line and acute neurological deficit: A case series. J Tehran Heart Cent. 2014;9:186-90.
- [Google Scholar]
- Paradoxical emboli after central venous catheter removal. Ann Oncol. 2000;11:885-6.
- [Google Scholar]
- Thrombosis: The major Hickman catheter complication in patients with solid tumor. Chest. 1989;95:71-5.
- [Google Scholar]
- Venous access: A prospective, randomized study of the Hickman catheter. Surgery. 1984;95:303-8.
- [Google Scholar]
- Vascular complications of central venous catheter placement: Evidence-based methods for prevention and treatment. J Cardiothorac Vasc Anesth. 2014;28:358-68.
- [Google Scholar]
- Complications of catheters: Tunneled and nontunneled. Adv Chronic Kidney Dis. 2012;19:188-94.
- [Google Scholar]
- Cerebral infarction complicating subclavian vein catheterization. Ann Neurol. 1977;1:253-4.
- [Google Scholar]
- Ultrasound-guided cannulation of the internal jugular vein. A prospective, randomized study. Anesth Analg. 1991;72:823-6.
- [Google Scholar]
- Ultrasound guidance for placement of central venous catheters: A meta-analysis of the literature. Crit Care Med. 1996;24:2053-8.
- [Google Scholar]
- Ultrasonic locating devices for central venous cannulation: Meta-analysis. BMJ. 2003;327:361.
- [Google Scholar]
- Pressure waveform monitoring during central venous catheterization. Anesth Analg. 2009;109:2030-1.
- [Google Scholar]
- Stroke after internal jugular venous cannulation. Acta Neurol Scand. 2002;105:235-9.
- [Google Scholar]
- Ultrasound-guided subclavian vein catheterization: A systematic review and meta-analysis. Crit Care Med. 2015;43:1498-507.
- [Google Scholar]
- Landmark-guided subclavian vein catheterization by palpating the subclavian artery. Am J Emerg Med 2017:pii: S0735-6757(17) 30680-0.
- [Google Scholar]
- Intravascular complications of central venous catheterization by insertion site. N Engl J Med. 2015;373:1220-9.
- [Google Scholar]
- Confirmation of endovenous placement of central catheter using the ultrasonographic “bubble test”. Indian J Crit Care Med. 2015;19:38-41.
- [Google Scholar]
- High oxygen saturation does not always indicate arterial placement of catheter during internal jugular venous cannulation. Anesthesiology. 1985;62:372-3.
- [Google Scholar]
- Arterial misplacement of large-caliber cannulas during jugular vein catheterization: Case for surgical management. J Am Coll Surg. 2004;198:939-44.
- [Google Scholar]
- Inadvertent prolonged cannulation of the carotid artery. Anesth Analg. 1982;61:150-2.
- [Google Scholar]
- The warfarin-aspirin symptomatic intracranial disease study. Neurology. 1995;45:1488-93.
- [Google Scholar]
- A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med. 2001;345:1444-51.
- [Google Scholar]
- Management of occlusion and thrombosis associated with long-term indwelling central venous catheters. Lancet. 2009;374:159-69.
- [Google Scholar]
- Antithrombotic therapy in neonates and children: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition) Chest. 2008;133:887S-968S.
- [Google Scholar]
- Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition) Chest. 2008;133:454S-545S.
- [Google Scholar]
- Deep vein thrombosis associated with central venous catheters – A review. J Thromb Haemost. 2005;3:2409-19.
- [Google Scholar]






