Translate this page into:
Impairments in Quality of Life and Cognitive Functions in Long-term Survivors of Glioblastoma
Address for correspondence: Dr. Arivazhagan Arimappamagan, Department of Neurosurgery, National Institute of Mental Health and Neurosciences, Bengaluru, Karnataka, India. E-mail: arivazhagan.a@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The incidence of long-term survival in glioblastoma (GBM), i.e., >3 years, ranges from 3% to 5%. Although extensive research is performed in novel therapies for prolonging survival, there is a scarcity of research focusing on the impact of tumor and treatment on cognitive, psychological, and social status of survivors. This study is an attempt to look into this poorly addressed important issue.
Materials and Methods:
Nine patients (six adults and three children) with GBM who had survived >3 years were included in the study. The quality of life (QOL) functions were assessed with the World Health Organization QOL Questionnaire BREF questionnaire. The neuropsychological assessment was done using the National Institute of Mental Health and Neurosciences neuropsychology battery for adults and children. The scores were compared with normative data.
Results:
The physical and psychological health-related QOL of long-term GBM survivors were affected considerably due to fatigue, poor quality of sleep, inability to concentrate, presence of depression, financial burden with impaired personal and social relationships (P < 0.05). Different domains of cognitions such as motor speed (P = 0.0173), mental speed (P = 0.0022), sustained attention (P = 0.0001), long-term memory (P = 0.0431), mental flexibility (P < 0.05), and planning and executive functions (P < 0.05) were significantly impaired affecting personal, social, and professional lives.
Conclusion:
The health-related QOL and cognition are significantly impaired in GBM long-term survivors. As the incidence of long-term survival is very less, there is a need for larger multicenter studies to come up with definitive results, which in turn can help in formatting the rehabilitative and support programs for these patients.
Keywords
Cognitive functions
glioblastoma
long-term survival
quality of life
INTRODUCTION
Despite multimodal aggressive treatment of glioblastoma (GBM), comprising surgical resection, local radiotherapy (RT), and systemic chemotherapy, the median overall survival time after diagnosis remains still in the range of 12–15 months only. Modest 2%–4% increases in incidence have been shown in the last 10–20 years, with minimal improvements in 2-year GBM survival from 3% to 6%.[1] A small fraction of GBM patients survive for >36 months, which constitutes 2%–5% of all GBM patients.[2] These patients are referred to as long-term survivors. Some of the studies have earlier considered >18 months of survival as long-term survival.[3] The long-term survival of >3 years in a study by Scott et al. was only 1.8%.[4] Recent studies have demonstrated that survival in GBM has significantly improved with overall survival reaching 27.2% at 2 years, 16.0% at 3 years with RT, and temozolomide (TMZ) chemotherapy.[5]
The adjuvant RT and chemotherapy can also have significant effects on the quality of life (QOL). Further, the involvement of brain by the disease and surgery can also result in varied neurological deficits in either motor or cognitive domain. The QOL and cognitive deficits, especially in long-term survivors are important aspects which have not been studied extensively till date. Although the neurological outcome may be good at discharge following surgery, neuropsychological tests may reveal an array of cognitive defects disabling patients in their daily routine life. The QOL is a complex entity that originates from the interaction between a person's values and expectations and his/her actual experience.[6] QOL is defined as a multidimensional concept consisting of at least social, psychological, and physical phenomena.[7] Cognitive impairment is an outstanding sign of patients with brain tumors and constitutes the main domain of their QOL.[891011] QOL is affected by a number of social, emotional, financial, physical, and neurological factors. Modification of these factors may improve QOL.
As the median survival of GBM is expected to get better with more aggressive novel therapies in the future, the cohort of patients surviving beyond 3 years is expected to increase. The real issue is the notable scarcity of research on the QOL and cognitive outcomes in patients with GBM. An awareness and evaluation of these issues are essential to provide a wholesome care for these patients, in addition to medical therapy. The objective of the present study is to evaluate the impact on QoL and cognitive functions in the long-term survivors of GBM.
MATERIALS AND METHODS
The clinical data of patients of GBM who underwent surgical management at our institute from January 2006 to September 2011were reviewed. The patients who have survived for >3 years from the time of diagnosis (long-term survivors) were included for the study. Patients with preexisting psychiatric disorders or other preexisting cognitive or behavioral disorders were excluded from the study. The histopathological review of slides was done for confirmation of diagnosis. The QOL of the patients were evaluated in detail using the World Health Organization QOL Questionnaire BREF version (WHOQOL-BREF). The cognitive functions of the patients were evaluated using the National Institute of Mental Health and Neurosciences (NIMHANS) neuropsychological battery for adults and children, as appropriate and Vineland Social Maturity Scoring Scale in patients who were not in the physical or mental state to undergo detailed psychological examination. All patients gave consent for participating in the study. This study was approved by NIMHANS Ethics Committee. The assessments of all the patients were done in the hospital setting.
Quality of life assessment
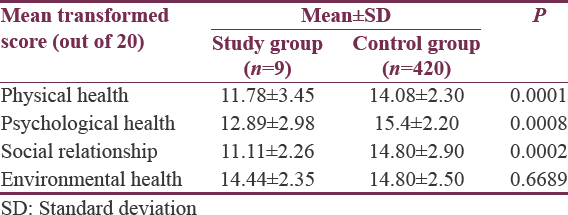
The QoL of long-term survivors of GBM patients was assessed by the WHOQOL-BREF questionnaire, which consists of 30 questions which finally determine the QOL in four domains, namely, physical health, psychological health, social relationship, and environmental health. The transformed scores of each domain were compared with the normative data from the WHO international field trial report.[12] From the international field trial report, the normative data of field trial conducted in Chennai (Madras), India, in 420 normal healthy individuals was selected as reference control values. The means of transformed scores of both case and control groups were compared by t-test. The P < 0.05 was considered as statistically significant.
Description of National Institute of Mental Health and Neurosciences neuropsychological battery tools
For neuropsychological evaluation of patients, the selected tools from NIMHANS neuropsychological battery were used.[13]
The motor speed was tested with the finger tapping. Mental speed was tested by the Digit Symbol Substitution test, which is a test for visuomotor coordination, motor persistence, sustained attention, and response speed. The color trail test was used for focused attention. Category fluency was tested using the animal naming test (ANT). The verbal working memory was tested using the N back tests. The visual working memory was tested by Spatial Span test forward and backward versions. The Tower of London (TOL) Test was used to test planning. Rey's test was used for auditory verbal learning and memory test (AVLT) and complex figure test for visual learning and memory. The method of testing in each test and the neuropsychological testing scores which were compared with the normative data have been published in NIMHANS neuropsychological battery manual.[13] The Student's t-test was used to calculate the significance.
RESULTS
Out of 717 patients with GBM, 254 were not contactable. Out of 463 patients who were contactable, 452 patients had expired due to the disease. We had a total of 11 patients who were surviving for >3 years. During the follow-up, one patient died before evaluation and one patient failed to respond to further communication. Therefore, nine patients were evaluated for QOL and cognitive status.
Clinical details of patients
Out of total nine long-term survivors of GBM, six patients were adults and three were children. Four were females and five were males. The age ranged from 11 to 60 years, with mean adult age was 41.34 years and mean age of children was 13 years. The clinical details of all the patients are as shown in Table 1. All the patients underwent surgical resection of tumor followed by adjuvant chemotherapy and radiation therapy. All the adult patients had received adjuvant RT and chemotherapy. Patients usually had received 54 Gy in fractions and 5–6 cycles of TMZ chemotherapy. One patient had received only two cycles of chemotherapy. All the children had received only RT. The treatment details are provided in Table 1. The patients clinical condition, pre- and post-operative Karnofsky performance scores have been provided in Table 1.
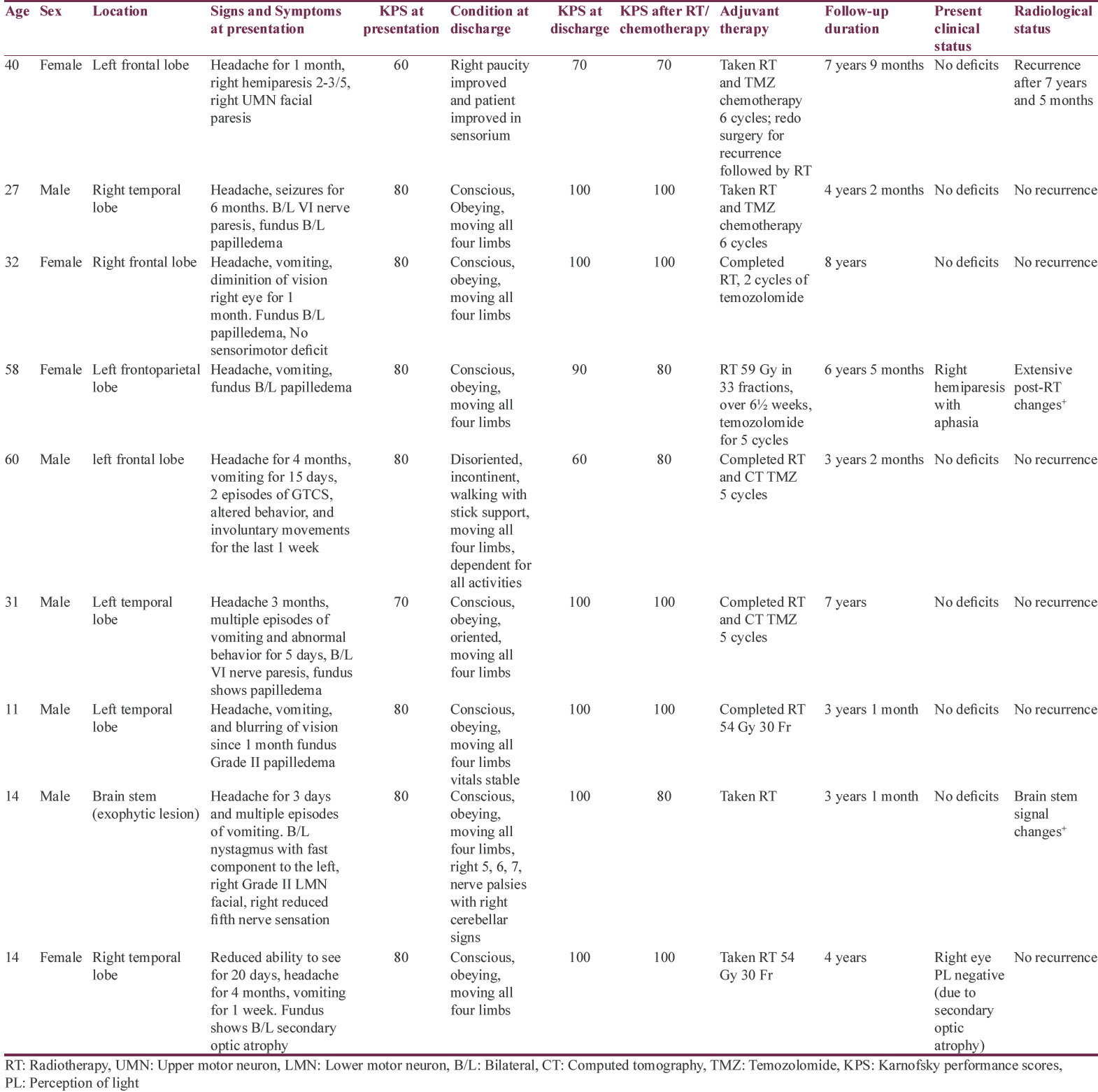
Eight out of nine patients did not have recurrence during the follow-up period. One patient, a 40-year-old female (patient number 1) had recurrence of the left frontal GBM after 7 years of diagnosis and treatment. She had undergone resection of the recurrence followed by adjuvant chemo-RT. The duration of survival ranged from 3 to 8 years. The mean overall survival of all patients was 62 months.
Quality of life of long-term glioblastoma survivors
The physical and psychological health were significantly impaired in patients with GBM. In addition, social life was affected in these patients. The physical health domain of QOL showed that patients had a significant amount of fatigue and impaired quality of sleep. Six patients (66.67%) had significant lack of energy during daily routine activities, and 4 (44.44%) patients had significant restricted mobility with one patient being wheelchair bound. In psychological health assessment, out of nine patients, eight patients were not able to enjoy life the way they wanted to. Seven (77.778%) patients had their QOL affected significantly so that they were able to enjoy life only to moderate amount or a little and they did not find their life meaningful to a significant extent. Eight (88.88%) patients reported that they were not able to concentrate in their work to significant extent. Five patients (55.56%) expressed mild to moderate degree of negative feelings such as depression, anxiety, despair, or blue mood. In the assessment of social relationships, 7 (77.78%) patients were not satisfied with their personal relationships. Most of the adults were also not satisfied with their sexual life. They were also dissatisfied to some extent with the social support from their friends and family. In environmental health assessment, 8 (88.89%) patients expressed a feeling of uncertainty and loss of safety in their life to moderate amount as well as not feeling the environment healthy. Most of the patients thought they did not have enough money according to their needs. The mean of transformed scores of all the domains as compared to normals are significantly different in all domains [Table 2].
Cognitive outcome in adult long-term glioblastoma survivors
Out of six adults, one patient (patient number 4) was significantly disabled both physically as well as psychologically with gross cognitive decline and she was not in a clinical condition to undergo detailed assessment.
Finger tapping in the right hand was significantly impaired on analysis. All patients being right handed, the impaired motor speed on the right side irrespective of location of lesion suggests generalized impaired motor function in these patients. The visuomotor coordination, motor persistence, sustained attention, and response speed were significantly impaired in these patients. On Color Trail Test, two patients took significantly more time than controls (P = 0.0001). This result suggests impairment of mental flexibility in addition to sustained attention, perceptual thinking, and simple sequencing. On ANT, the patients were able to tell an average of 13 names in a minute which was quite similar to controls without any significant difference, indicating that the category fluency was not impaired. Both verbal and visual working memories were not impaired. On “TOL” test, the impairment in ability of planning was significant. In the AVLT, long-term memory was significantly affected in GBM survivors. Visual learning and visual working and recent memories were not affected in the GBM survivors [Table 3].
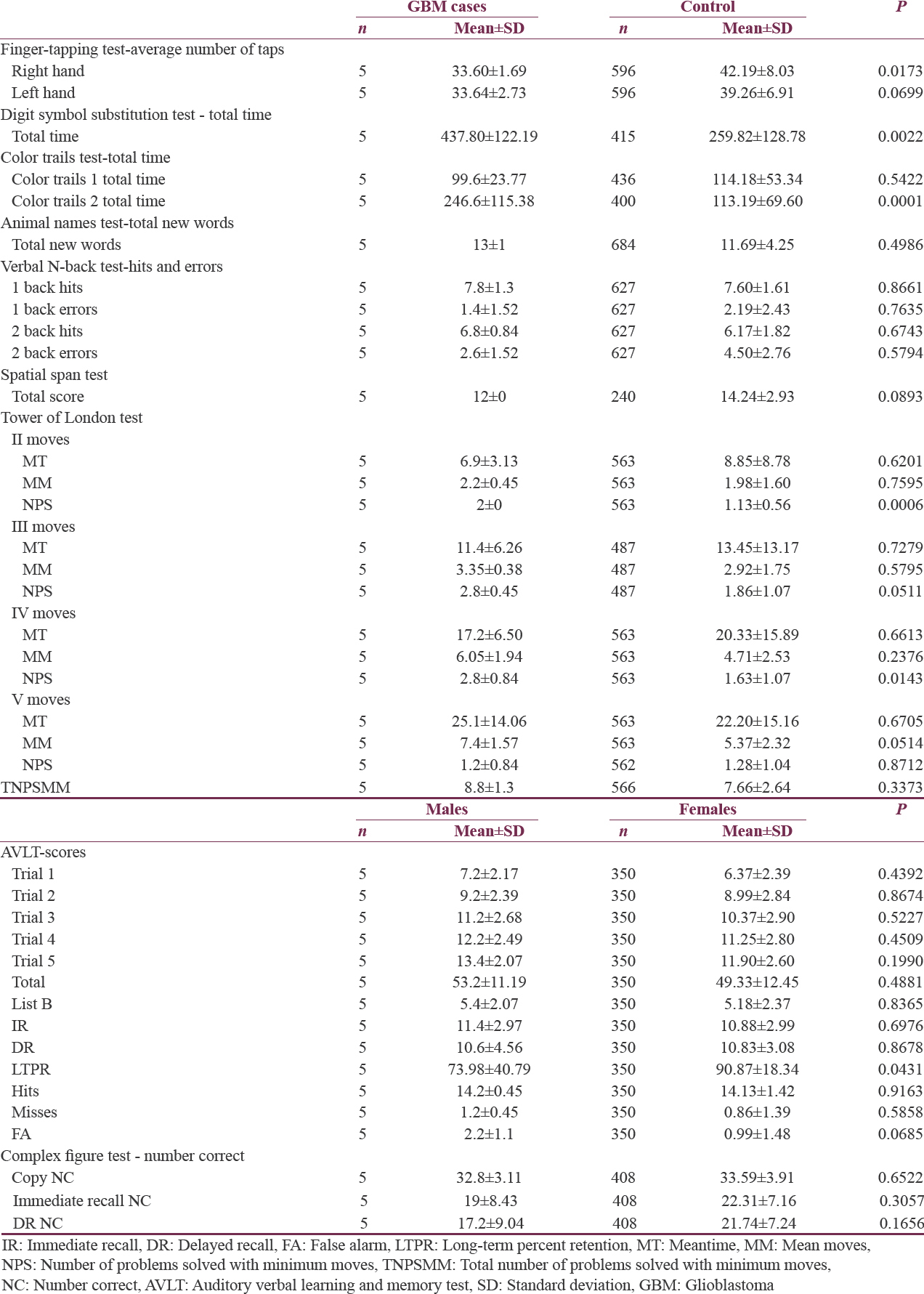
Hence, we noted that adult long-term survivors of GBM had impaired motor speed on dominant side, impairment in mental speed, focused attention, planning ability, and long-term memory as compared to normal healthy individuals.
Cognitive outcome in pediatric long-term glioblastoma survivors
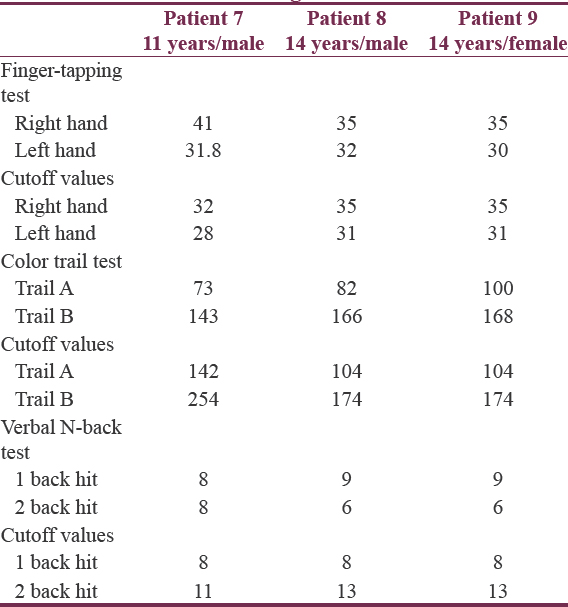
As the normative cognitive data were separate for pediatric population, the children with GBM, who are surviving beyond 3 years after diagnosis could not be included in the analysis along with the adult patients. Since there were only three patients in test group, it was plausible only to compare the test value with the normative cutoff scores for the particular age. Hence, detailed statistical analysis was not possible in pediatric age group.
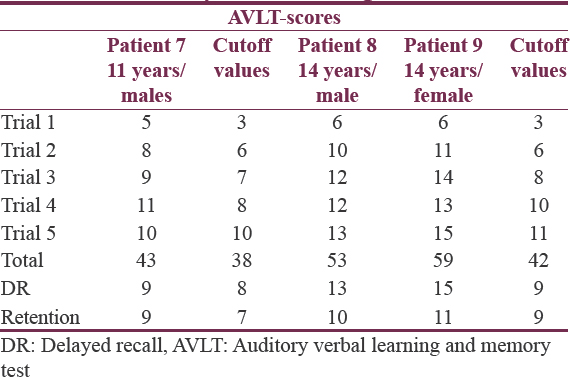
There was no impairment in motor function on either side with normal preserved attention span in these patients. The lower 2 back score in these patients was suggestive of impairment of verbal working memory [Table 4]. The AVLT was used to assess the verbal learning and memory. For all the three children, the scores were above the cutoff values suggesting no deterioration in verbal learning capacity and verbal memory [Table 5]. In addition, the intelligence quotient (IQ) was calculated for these children. The IQ of three patients ranged from 107 to 127, demonstrating that the overall cognitive functioning in children was not affected.
DISCUSSION
The development of brain tumor itself can result in significant physical disabilities, predominantly associated with the specific tumor locations in eloquent areas, impairment of cognitive skills and memory. The effects of surgical resection of the tumor, RT, and chemotherapy can compound the effects on QOL and cognitive abilities of these patients, although increasing the period of survival after cancer diagnosis.
In the present study, all patients, except one, had independence in activities of their daily living despite the impairments caused by tumor and its treatment. The physical health domain of QOL showed that the patients had a significant amount of fatigue and impaired quality of sleep. Six patients (66.67%) had a significant lack of energy during daily routine activities, and 4 (44.44%) patients had significant restricted mobility with one patient being wheelchair bound. This study noted that patients had significant impairment of physical QOL. Similarly, fatigue is reported to be the most common symptom in patients with brain tumors in general.[14] Steinbach et al. showed in long-term survivors of GBM that these patients were unable to work and participate in everyday and social activities due to fatigue.[15]
Loss of self-esteem and depression are important psychological morbidities prevailing in patients with cancer. The fear of uncertainty and prolonged treatment and follow-up required in the disease management affect the general mood of the patients. Overall, patients had significant impairment of psychological aspect of QOL in this study. Similar studies have reported significant amount of depression in high-grade glioma patients and also in long-term survivors of GBM.[314151617]
The present study revealed that patients had significantly impaired personal and social relationships. They were also dissatisfied by the support they get from their family members and friends. The high-grade gliomas not only affect the QOL of the patient but also that of the family members and caretakers, thus acting as a double-edged sword. In a study by Janda et al., it was found that even the QOL of the caregivers of brain tumor patients was also affected significantly.[18] That adds to the impairment of quality of social life of patients. Taphoorn et al. found similar results related to impairments in QOL in patients diagnosed to have GBM.[19]
Compared to the Western countries, the social fabric and culture in India assure a good amount of social support to the patients with medical illness. The prevalence of joint family system and predominantly patriarchal type of family setup ensures the availability and willingness of the caregivers to take care of the patients. Despite that, we noticed that patients with GBM have a significant extent of impairment in social relationships.
The feeling of future uncertainty and lack of safety were also the factors affecting the quality of living environment, also the financial burden adding to the misery. Hahn et al. also reported that patients with primary malignant brain tumors found their lives hopeless with significant amount of depression and confusion.[17] In a study conducted in Austria by Flechl et al.,[20] they found future uncertainty and financial problems significantly affecting the QOL in long-term GBM survivors. In Austria, despite having one of the best healthcare and social security systems in the world, their long-term GBM survivors are suffering from significant financial burden. In a developing country like India where most of the people meet the medical expenses through personal savings, the need for a prolonged and costly treatment can become a significant financial burden on the patient and family. The effects of RT can be progressive and may appear many months to years after the treatment.[21]
The present study documented impairment of specific cognitive functions in these long-term survivors of GBM. The effects on cognitive functions are probably multifactorial, namely, the tumor itself, surgery, RT, and chemotherapy effects. We found that the motor speed on the right side, which was the dominant side for all patients, was significantly affected as compared to healthy controls on test of finger tapping. There was no significant association between location of tumor and motor speed.
The subjects in our study had impaired visuomotor coordination, motor persistence, and sustained attention. The response speed was also affected. These patients also had impaired mental flexibility and long-term memory. Steinbach et al. also found that attention was significantly affected in patients with GBM who had survived for >5 years.[15] We also found impairments in ability to plan and remember information for a longer period, thereby affecting independence in day-to-day functioning. Similar results were reported in another study on recurrent glioma patients.[22] Hottinger et al. noted that the long-term GBM survivors had significant impairment of cognitive functions with affected attention and memory.[23]
We did not find association of cognitive deficits and location of tumor, though the sample is very small to make any definite inferences. Flechl et al. also did not find such association in long-term GBM survivors.[20] Some studies performed in patients with low-grade glioma found that cognitive deficits are common when the tumor is located in the left frontal lobe.[2425] However, no studies have found similar association for high-grade gliomas. It can be considered that high-grade primary brain tumors may have changes in higher mental functions irrespective of their location in either eloquent or noneloquent areas of brain, which can possibly be due to the systemic chemotherapy and RT, resulting in global cognitive dysfunction, irrespective of the location.
In children, the long-term survivors of GBM did not have a significant effect on cognitive functions. However, these results should be interpreted with caution due to very small sample size. Another concern in pediatric age group is that the GBM in children is a different entity with relatively better prognosis as compared to adults. The median overall survival is reported as 43 months with the median progression-free survival of 12 months. The overall survival rate was 67% at 1 year, 52% at 2 years, and 40% at 5 years.[26] There is a potential to study these children separately for the impairment in QOL and cognitive functions in a multicenter study to obtain sufficient number of long-term survivors and to derive strong conclusions.
To summarize, the patients with GBM, despite having improved survival, are left with significantly impaired overall health-related QOL as well as impairments in various domains of cognition affecting functional status. Consequentially, there is an explicit necessity to address these issues of QOL and cognitive status in addition to improving the treatment strategies for prolonging survival. There should be a lot of emphasis and need for integrated rehabilitative and support programs as well as financial safeguard and social integration of these patients and caregivers to improve the QOL of these patients. A more inclusive multidisciplinary approach with stress on post-treatment care, psychological support, awareness of the disease, improvement in social support, disease-specific patient group interactions with active inputs from medical personnel can enhance the QOL of these patients in the long term.
CONCLUSION
The QOL of long-term GBM survivors is affected considerably due to fatigue, poor quality of sleep, inability to concentrate, presence of depression, financial burden, and impaired personal and social relationships. Different domains of cognition like motor speed, sustained attention, long-term memory, mental flexibility and executive functions are significantly impaired affecting personal, social, and professional lives. The limitation of this study is that the sample size is small. Notwithstanding the limitations, the present study clearly portrays the significant impairment of QOL in long-term survivors of GBM and identifies need to simultaneously address these issues in management of these patients and to ensure a wholesome approach in the management of GBM.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- RESPONSE: Re: Brain and other central nervous system cancers: Recent trends in incidence and mortality. J Natl Cancer Inst. 2000;92:77A-8.
- [Google Scholar]
- Distress persists in long-term brain tumor survivors with glioblastoma multiforme. J Cancer Surviv. 2008;2:269-74.
- [Google Scholar]
- Long-term glioblastoma multiforme survivors: A population-based study. Can J Neurol Sci. 1998;25:197-201.
- [Google Scholar]
- Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009;10:459-66.
- [Google Scholar]
- Quality of life: What is it? How should it be measured? Oncology (Williston Park). 1988;2:69-76, 64.
- [Google Scholar]
- Cognitive impairment and quality of life in long-term survivors of malignant brain tumors. Ital J Neurol Sci. 1994;15:481-8.
- [Google Scholar]
- Cognitive functioning and quality of life in malignant glioma patients: A review of the literature. Psychooncology. 1997;6:169-77.
- [Google Scholar]
- Quality of life in patients with stable disease after surgery, radiotherapy, and chemotherapy for malignant brain tumour. J Neurol Neurosurg Psychiatry. 1999;67:358-63.
- [Google Scholar]
- WHOQOL Group. The World Health Organization's WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res. 2004;13:299-310.
- [Google Scholar]
- NIMHANS Neuropsychology Battery Manual. Bangalore, India: NIMHANS Publication; 2004.
- Quality of life in brain tumor patients: The relative contributions of depression, fatigue, emotional distress, and existential issues. J Neurooncol. 2002;57:41-9.
- [Google Scholar]
- Surviving glioblastoma for more than 5 years: The patient's perspective. Neurology. 2006;66:239-42.
- [Google Scholar]
- Impact of therapy on quality of life, neurocognitive function and their correlates in glioblastoma multiforme: A review. J Neurooncol. 2011;104:639-46.
- [Google Scholar]
- Prospective study of neuropsychologic testing and quality-of-life assessment of adults with primary malignant brain tumors. Int J Radiat Oncol Biol Phys. 2003;55:992-9.
- [Google Scholar]
- Quality of life among patients with a brain tumor and their carers. J Psychosom Res. 2007;63:617-23.
- [Google Scholar]
- Health-related quality of life in patients with glioblastoma: A randomised controlled trial. Lancet Oncol. 2005;6:937-44.
- [Google Scholar]
- Neurocognitive and sociodemographic functioning of glioblastoma long-term survivors. J Neurooncol. 2012;109:331-9.
- [Google Scholar]
- Neurocognitive deficits after radiation therapy for brain malignancies. Am J Clin Oncol. 2015;38:634-40.
- [Google Scholar]
- Cognitive function as a predictor of survival in patients with recurrent malignant glioma. J Clin Oncol. 2000;18:646-50.
- [Google Scholar]
- Neurological outcome of long-term glioblastoma survivors. J Neurooncol. 2009;95:301-5.
- [Google Scholar]
- Early cognitive impairment in a subset of patients with presumed low-grade glioma. Neurocase. 2010;16:503-11.
- [Google Scholar]
- Factors influencing neurocognitive outcomes in young patients with benign and low-grade brain tumors treated with stereotactic conformal radiotherapy. Int J Radiat Oncol Biol Phys. 2010;77:974-9.
- [Google Scholar]
- Long-term outcomes in children with glioblastoma. J Neurosurg Pediatr. 2010;6:145-9.
- [Google Scholar]






