Translate this page into:
How do repeat suicide attempters differ from first timers? An exploratory record based analysis
Address for correspondence: Dr. Vikas Menon, Department of Psychiatry, Jawaharlal Institute of Post Graduate Medical Education and Research, Puducherry - 605 006, India. E-mail: drvmenon@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Evidence indicates that repeat suicide attempters, as a group, may differ from 1st time attempters. The identification of repeat attempters is a powerful but underutilized clinical variable.
Aims:
In this research, we aimed to compare individuals with lifetime histories of multiple attempts with 1st time attempters to identify factors predictive of repeat attempts.
Setting and Design:
This was a retrospective record based study carried out at a teaching cum Tertiary Care Hospital in South India.
Methods:
Relevant data was extracted from the clinical records of 1st time attempters (n = 362) and repeat attempters (n = 61) presenting to a single Tertiary Care Center over a 4½ year period. They were compared on various sociodemographic and clinical parameters. The clinical measures included Presumptive Stressful Life Events Scale, Beck Hopelessness Scale, Coping Strategies Inventory – Short Form, and the Global Assessment of Functioning Scale.
Statistical Analysis Used:
First time attempters and repeaters were compared using appropriate inferential statistics. Logistic regression was used to identify independent predictors of repeat attempts.
Results:
The two groups did not significantly differ on sociodemographic characteristics. Repeat attempters were more likely to have given prior hints about their act (χ2 = 4.500, P = 0.034). In the final regression model, beck hopelessness score emerged as a significant predictor of repeat suicide attempts (odds ratio = 1.064, P = 0.020).
Conclusion:
Among suicide attempters presenting to the hospital, the presence of hopelessness is a predictor of repeat suicide attempts, independent of clinical depression. This highlights the importance of considering hopelessness in the assessment of suicidality with a view to minimize the risk of future attempts.
Keywords
Attempted suicide
cognition
depression
hopelessness
suicide
Introduction
Suicide is a major social and public health issue worldwide.[12] A prior suicide attempt is one of the strongest predictors of eventual suicide.[34] However, there are difficulties in accurately identifying individuals who are likely to repeat from a sample of 1st time suicide attempters. Traditionally, clinicians and researchers viewed all suicide attempters together regardless of their number of attempts. However, emerging evidence suggests that there are robust differences between 1st time and multiple suicide attempters.[5] Multiple attempters tend to be single young subjects,[6] with a positive family history of suicide,[78] having poor adaptive functioning,[9] poor coping resources,[6] and various psychiatric co-morbidities including schizophrenia, depression, substance use, and personality disorders.[67910] Rudd et al. compared three groups: A group of young adult suicide ideators, 1st time suicide attempters, and multiple suicide attempters and they showed that last group had elevated levels of depression, hopelessness, perceived stress, and poor coping.[11] Similar findings were also reported by investigators who studied people with more number of lifetime attempts[12] and adolescents.[13] From a clinical standpoint, characterization of repeat attempters is important as they are at a greater risk of eventually killing themselves.[14] From a suicide prevention perspective, this group merits closer attention as identifying repeat suicide attempters is a simple, convenient way of risk stratification for management.[9] Notwithstanding these obvious gains, studies trying to delineate repeat attempters are rare from Asian countries. This is important to know as the characteristics of repeat attempters may differ as a function of culture and ethnicity. The present study aims to support the existing literature by trying to identify the clinical and demographic variables that differentiate repeat suicide attempters from 1st time attempters in South India. To remove the possible interaction of risk factors, we also aimed to identify independent predictors of repeat attempts using a regression model.
Methods
Context of the study
The study setting was the outpatient Department of Psychiatry at a teaching cum Tertiary Care Hospital in South India. Baseline evaluation of subjects was done in the crisis intervention clinic (CIC), a specialty clinic run by the Department of Psychiatry since January 2010, offering multimodal care for clients with attempted suicide. The case assessment and management protocol followed in the clinic has been described in detail elsewhere.[15] Patients are referred to CIC from various departments of the hospital after medical stabilization. The duration between the first contact to hospital and interview in CIC ranged between 2 and 7 days. Questionnaire and instruments used in the clinic were based on the literature review and opined to be relevant for the clinic for risk stratification of the suicide attempters and their management. For the purposes of the study, suicide attempt was defined as a self-inflicted, potentially injurious behavior with a nonfatal outcome for which there is evidence (either explicit or implicit) of intent to die.[16]
Data collection
The following instruments are used to collect relevant sociodemographic and clinical data as part of evaluation at the CIC:
-
Semi-structured proforma designed to tap the relevant psychosocial and demographic details
-
Presumptive Stressful Life Events Scale, a 51-item scale constructed and standardized specifically for the Indian population.[17] The items, which include both desirable and undesirable stressful events, are quantified with weighted scores. We used the scale primarily as a checklist to elicit the number of stressful life events that occurred in last 1-year preceding the suicide attempt
-
Beck Hopelessness Scale (BHS) - This is a 20-item validated true-false scale used to measure the negative attitudes and expectancies of the patients which reflect hopelessness. It has 9-item keyed false and 11-item keyed true. Each item is scored 0 or 1, and hence, total scores summing all the items can range from 0 to 20.[18] The total score on the scale were used for analysis. The scale has been previously used by Indian suicide researchers[19]
-
Coping Strategies Inventory (CSI) – Short Form. The CSI was originally developed as a 78-item instrument to elicit and categorize coping responses to day to day situations. A shortened 16-item version has been developed to reflect the original scale without loss of psychometric properties and yields 4-item sub-scale scores: (a) Problem -focused engagement, (b) problem-focused disengagement, (c) emotion-focused engagement, and (d) emotion-focused disengagement[20]
-
Global Assessment of Functioning Scale – This is axis-V of Diagnostic and Statistical Manual of Mental Disorders-4th Edition, which records the clinicians judgment regarding the highest level of adaptive functioning, in the areas of social relations, occupational functioning, and use of leisure time, demonstrated by the individual during the past 1-year.[21] The scale has a score range of 1–100. Higher the score, better the adaptive functioning.
All questionnaires were administered by postgraduate residents in the Department of Psychiatry, who were given training on the use of these instruments. Psychiatric diagnoses were made through clinical interviewing and finalized after discussion with the consultant-in-charge of the clinic (SK). International Classification of Diseases-10, classification of mental, and behavioral disorders: Clinical descriptions and diagnostic guidelines were followed in making diagnoses.[22]
The department maintains a comprehensive database of all patients who have availed of services in the CIC since its inception. For this research, we scrutinized the clinical charts of 439 patients who had registered themselves from the inception of the clinic till July 2014. They were categorized into two groups – 1st time and multiple attempters and were compared on various sociodemographic and clinical parameters.
Data analysis
Data were analyzed using SPSS version 20 (IBM Corp, TX, USA). An initial univariate analysis comparing the 1st time and multiple suicide attempters was done using Mann–Whitney U-test for continuous data or Chi-square test for discrete variables. The strength of these comparisons was measured with nonparametric pˆ for skewed distribution continuous data and Cramer's V for discrete data, the higher value of which suggests a better effect size of the association. The pˆ was computed as Mann–Whitney U/(nAnB), where nA and nB were the sample sizes of the two groups. The variables which showed at least a trend level significance in this univariate analysis (P < 0.10) were entered into the backward logistic regression model to identify predictors of multiple attempters. Backward logistic model was used as it minimizes the number of variables by using a limited number of co-variates. All statistical analysis was done for two-tailed significance and the statistical level of significance (P value) was set at 0.05 for univariate and final multivariate model.
Results
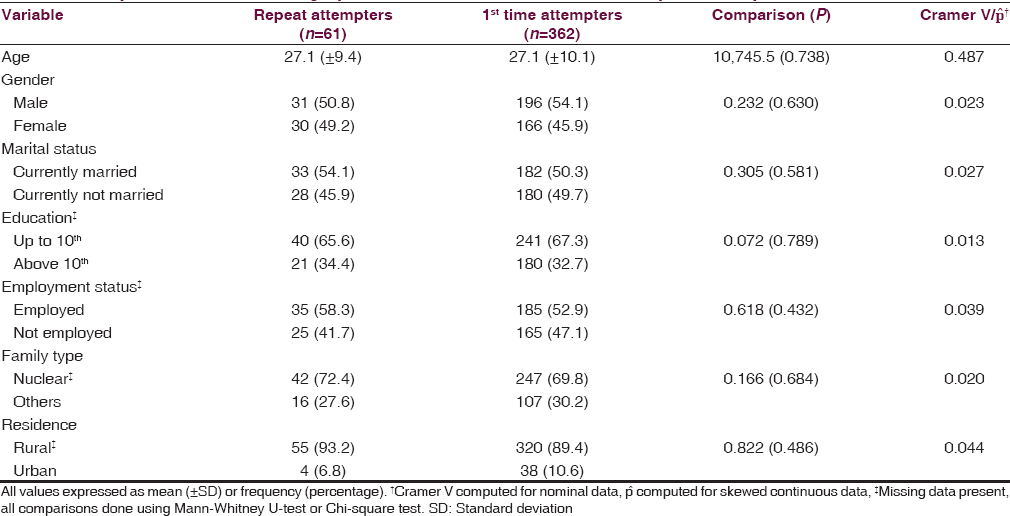
A total of 439 patients were registered in the CIC during the study period. Of them, a suicidal attempt could be established in 423 patients (96.4 of the sample). Sixty-one (14.4%) were repeat attempters while remaining 362 (85.6%) were first ever attempters. The differences in demographic characteristics of 1st time attempters and repeat suicide attempters are shown in Table 1. The two groups did not differ significantly across any of the demographic variables.
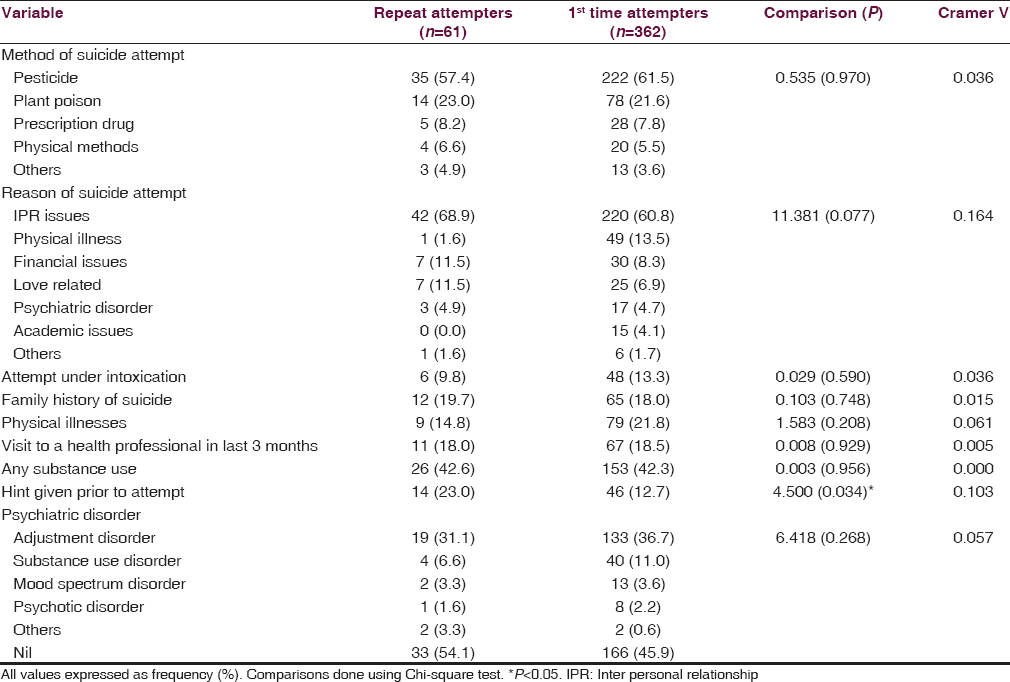
The methods and the reasons of suicidal attempt are depicted in Table 2. Overall, use of pesticide was the most common method for a suicide attempt. Interpersonal relationship issues were the most common reason of suicide attempt. A larger proportion of repeat suicide attempters had given hint prior to a suicide attempt. Otherwise, the two groups did not significantly differ between each other on the attempt being made under intoxication, having a family history of suicide, having a physical illness, visit to a health professional in past 3 months, or substance use. Adjustment disorder was the most common clinical diagnosis in both the groups.
The number of stressors [Table 3] reported by the two groups did not significantly differ. Furthermore, the coping sub-scale scores, inpatient stay durations and functioning in the past 1-year scores did not significantly differ between the groups. Significant differences were noted in the BHS scores, with repeat attempters having greater levels of hopelessness.
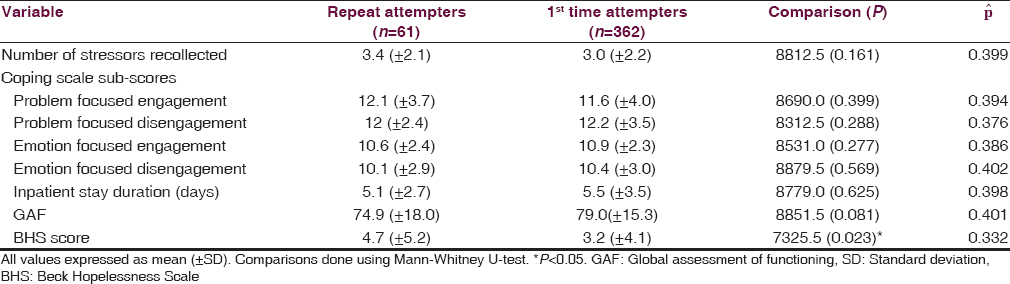
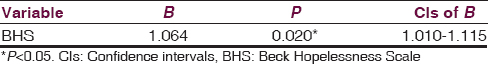
Logistic regression analysis was conducted to find the independent predictors of repeat attempts. Those variables which showed at least a trend level significance on univariate analysis (P < 0.10) were entered into backward Wald regression. It was seen that higher BHS score was the only variable that independently predicted repeat suicide attempts (P = 0.020) [Table 4]. Each point increase in BHS scores was associated with increase in the chance of making a repeat suicide attempt by 6.4% (95% confidence intervals [CIs] of 1.0% to 11.5%) (odds ratio - 1.064, 95% CIs of 1.010–1.115). The Nagelkerke R2 of the model was 0.23 and the correct classification rate was 85.9%.
Discussion
The present hospital record based study tried to compare the sociodemographic and clinical characteristics between 1st time (n = 362) and repeat (n = 61) suicide attempters. We found that the two groups did not differ on any of the demographic characteristics. This is broadly similar to previous reports from India[10] and the West[923] and suggests that the demographics of repeat attempters tend to remain uniform across various ethno-cultural settings. Only a few studies have reported a female preponderance among multiple attempters.[24]
Repeat attempters did not differ from single attempters when compared on the preferred mode and reasons for the current attempt. This is consistent with prior reports that failed to show any incremental lethality with subsequent attempts among multiple lifetime attempters.[25] Further, no differences were found on their health care seeking patterns as both the groups had sought the help of a health-care professional in the preceding 3 months. However, we noted that repeat attempters were more likely to have dropped verbal or other hints prior to their attempts. This raises important questions about the availability of a window period for intervention in this group that may reduce the possibility of suicidal acts and is worth exploring further.
No significant differences emerged between 1st time and repeat suicide attempters in terms of psychiatric morbidity, coping styles, levels of stress, and overall functioning. Our findings differ with the conclusions drawn by Forman et al. who showed that multiple suicide attempters displayed poorer problem solving skills and experienced greater relationship difficulties.[9] A 2 years follow-up study showed higher rates of major depression among repeat attempters.[10] However, a recent report extending the follow-up to 10 years did not suggest any differences in rates of axis-I co-morbidity between 1st time and multiple attempters similar to our findings.[26]
The major finding of the present study was that levels of hopelessness distinguished 1st time attempters from repeat attempters. Similar findings have been noted earlier by Rudd et al. though their sample composed of only young adults enlisted for military duty.[11] Increased concurrent expression of depression and hopelessness has been consistently reported among multiple attempters by previous investigators who compared this group with first ever attempters.[6910] According to many classic, as well as recent papers, depression, and hopelessness are closely linked and hopelessness mediates the relationship between depression and intent in attempted suicide.[27282930] However, few studies have shown an association of hopelessness with repeat attempts, independent of depression as we have done. Our findings are probably of clinical and theoretical relevance because it tells us that hopelessness could be an independent predictor of multiple suicide attempts even in the absence of clinical depression. We propose an amalgamation of the strain theory of suicide[31] with Beck's theory of modes[32] which may provide a generic cognitive model for multiple suicidal behaviors. The strain theory postulates that psychological strain, brought on by contradictory and competing pressures in an individual's life, precedes suicidal behavior.[33] As this strain gets too overwhelming, his or her coping repertoire may get exhausted, and hopelessness may occur prior to the contemplation of suicide. Over a period of time, this organization of schemas relevant to negative expectancies, memories, and self-evaluations, referred to as modes by Beck,[34] may get established and prone to activation by minimal triggers.[3235] To sum up, the suicidal mode preceded by cognitive hopelessness becomes easily accessible to the individual when it is repeatedly engaged in and requires minimal triggering stimuli for its subsequent activation as it is fresh in memory. A closer evaluation of the relationship between hopelessness and multiple suicide attempts through prospectively designed studies may help to further our theoretical understanding of how hopelessness may be causally related to attempt status or vice versa.
Our findings need to be interpreted in the context of certain limitations. This was a record based study, and hence, carries some design limitations including recall bias. The findings are drawn from a single Tertiary Care Center, and hence, needs wider replication for generalizability. No structured instrument was used to assess psychiatric co-morbidity. Furthermore, the two groups (repeat suicide attempters and first timers) were unbalanced in terms of the distribution of the number of cases, necessitating use of nonparametric tests. The strengths of this study include studying a well-defined sample of suicide attempters using internationally accepted nomenclature and comparison of 1st time and repeat attempters on a broad set of variables to generate information. For the same reason, there was no admixture of parasuicides in our sample, otherwise a limitation in many studies on suicide. We also included certain novel variables such as health care seeking patterns not often seen in the literature. The measures used in this study are popular and validated across cultural settings, and hence, our results can be meaningfully when compared with global findings.
To conclude, the presence of hopelessness, irrespective of depression, may be a clinically useful marker to identify individuals at risk for making repeat suicidal attempts. This finding may have special significance for low and middle income countries where, consistently, lower rates of axis-I co-morbidity have been documented among suicide attempters[3637] as opposed to data from developed nations.[38] Other factors such as age, gender, stress, coping, and functioning did not distinguish these groups. Based on this, we propose that repeat suicide attempters as a group are different, at least in terms of cognitive schemas and may need different management approaches including case conceptualizations and treatment interventions. Hence, clinicians need to pay enhanced attention to the evaluation of hopelessness during a routine evaluation of attempted suicide. Further research questions that may be best addressed through longitudinal data in this group include whether and how hopelessness is causally related to the attempt status. The relationship of hopelessness with other factors that may predict multiple attempts also needs to be explored in order to come up with a coherent theoretical model for multiple suicidal attempts.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The epidemiology of suicide and parasuicide. Acta Psychiatr Scand Suppl. 1993;371:9-20.
- [Google Scholar]
- Suicide risk assessment and formulation: An update. Asian J Psychiatr. 2013;6:430-5.
- [Google Scholar]
- Factors associated with multiple versus single episode suicide attempts in the 1990-1992 and 2001-2003 United States national comorbidity surveys. J Nerv Ment Dis. 2008;196:806-13.
- [Google Scholar]
- Risk and protective factors predicting multiple suicide attempts. Psychiatry Res. 2013;210:957-61.
- [Google Scholar]
- Long-term follow-up of unsuccessful violent suicide attempts: Risk factors for subsequent attempts. J Trauma. 1992;33:457-64.
- [Google Scholar]
- Association between familial suicidal behavior and frequency of attempts among depressed suicide attempters. Acta Psychiatr Scand. 2009;119:406-10.
- [Google Scholar]
- History of multiple suicide attempts as a behavioral marker of severe psychopathology. Am J Psychiatry. 2004;161:437-43.
- [Google Scholar]
- Predictors of repeat suicidal attempts aftern first-ever attempt: A two-year follow-up study. Hong Kong J Psychiatry. 2008;18:131-5.
- [Google Scholar]
- Relationships among suicide ideators, attempters, and multiple attempters in a young-adult sample. J Abnorm Psychol. 1996;105:541-50.
- [Google Scholar]
- Multiple attempters of suicide presenting at an emergency department. Can J Psychiatry. 1986;31:328-30.
- [Google Scholar]
- Association between multiple suicide attempts and negative affects in adolescents. J Am Acad Child Adolesc Psychiatry. 1998;37:488-94.
- [Google Scholar]
- Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205-28.
- [Google Scholar]
- Stressful life events, hopelessness, and coping strategies among impulsive suicide attempters. J Neurosci Rural Pract. 2015;6:171-6.
- [Google Scholar]
- Rebuilding the tower of Babel: A revised nomenclature for the study of suicide and suicidal behaviors. Part 2: Suicide-related ideations, communications, and behaviors. Suicide Life Threat Behav. 2007;37:264-77.
- [Google Scholar]
- Presumptive stressful life events scale (PSLES) – A new stressful life events scale for use in India. Indian J Psychiatry. 1984;26:107-14.
- [Google Scholar]
- The measurement of pessimism: The hopelessness scale. J Consult Clin Psychol. 1974;42:861-5.
- [Google Scholar]
- Clinical and socio-demographic correlates of suicidal intent among young adults: A study from South India. Crisis. 2013;34:282-8.
- [Google Scholar]
- Psychometric evaluation of a Coping Strategies Inventory Short-Form (CSI-SF) in the Jackson Heart Study cohort. Int J Environ Res Public Health. 2007;4:289-95.
- [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. (5th ed). Arlington, VA: American Psychiatric Association; 2013.
- [Google Scholar]
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization; 1992.
- [Google Scholar]
- Diagnostic and psychosocial differences in psychiatrically hospitalized military service members with single versus multiple suicide attempts. Compr Psychiatry. 2014;55:450-6.
- [Google Scholar]
- Follow-up study of patients with attempted suicide. Int J Soc Psychiatry. 1988;34:285-91.
- [Google Scholar]
- Are high-lethality suicide attempters with bipolar disorder a distinct phenotype? Arch Suicide Res. 2009;13:247-56.
- [Google Scholar]
- Individuals with single versus multiple suicide attempts over 10 years of prospective follow-up. Compr Psychiatry. 2013;54:238-42.
- [Google Scholar]
- Hopelessness, depression and suicidal intent in parasuicide. Br J Psychiatry. 1984;144:127-33.
- [Google Scholar]
- Suicidal intent, hopelessness and depression in a parasuicide population: The influence of social desirability and elapsed time. Br J Clin Psychol. 1990;29(Pt 4):361-71.
- [Google Scholar]
- The association between depression and suicide when hopelessness is controlled for. Compr Psychiatry. 2013;54:790-6.
- [Google Scholar]
- Psychological strains and youth suicide in rural China. Soc Sci Med. 2011;72:2003-10.
- [Google Scholar]
- Advances in cognitive theory and therapy: The generic cognitive model. Annu Rev Clin Psychol. 2014;10:1-24.
- [Google Scholar]
- Psychological tensions found in suicide notes: A test for the strain theory of suicide. Arch Suicide Res. 2008;12:67-73.
- [Google Scholar]
- Beyond belief: A theory of modes, personality, and psychopathology. In: Salkovskis PM, ed. Frontiers of Cognitive Therapy. New York, US: Guilford Press; 1996. p. :1-25.
- [Google Scholar]
- Intensity and duration of suicidal crises vary as a function of previous suicide attempts and negative life events. J Consult Clin Psychol. 2000;68:909-16.
- [Google Scholar]
- Comparison of patients with and without mental disorders treated for suicide attempts in the emergency departments of four general hospitals in Shenyang, China. Gen Hosp Psychiatry. 2010;32:549-55.
- [Google Scholar]
- Psychiatric comorbidity and gender differences among suicide attempters in Bangalore, India. Gen Hosp Psychiatry. 2012;34:410-4.
- [Google Scholar]
- Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: A case-control study. Am J Psychiatry. 1996;153:1009-14.
- [Google Scholar]






