Translate this page into:
High intradural lumbar disk herniation: Known result of an unknown cause
Address for correspondence: Dr. Alugolu Rajesh, Department of Neurosurgery, Nizam's Institute of Medical Sciences,Punjagutta, Hyderabad - 500 082, Andhra Pradesh, India. E-mail: drarajesh1306@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Herniated disks, making their way into and through the dura are an uncommon feature of a fairly common problem of intervertebral disks. The diagnosis is usually made intraoperatively, for it is a very uncommon imaging differential.
A 65-year-old male presented with radiating pain along the right lower limb of two-weeks duration, associated with paraesthesias. There was neither a history of weakness of the limbs nor any bowel/bladder disturbances. The Lasegue's sign was negative. There were no other motor or sensory deficits. Magnetic resonance imaging (MRI) of the lumbosacral spine [Figure 1] showed the presence of an intradural lesion, which was isointense on a T1-weighted image (T1WI,) mildly hyperintense on a T2WI [Figure 2] weighted image, and enhancing on contrast, opposite to the D12-L1 disk space. The lesion was displacing the conus posteriorly. The disk, at this level, was dehydrated, but no obvious protrusion was seen on the sagittal images. The axial cuts at the same level showed an extradural component, which was hypointense as compared to the intrathecal hyperintense component. The working diagnosis was a schwannoma and the patient was taken up for surgery. D12 and L1 laminectomy was performed. Following durotomy a disk fragment was seen compressing the right L1 nerve root, surprisingly sparing the conus and cauda. The offending disk fragment was removed and decompression achieved. The dural rent was well-delineated and there were no adhesions between the dura and the posterior longitudinal ligament (PLL). The defect was closed by placement of sliver clips. In the postoperative period, the patient was relieved of his radicular pain and was doing well in the follow up, after 18 months.
Intradural disk herniations are not uncommon and account for up to 1.5% of all disk herniations,[1] and to date at least a hundred cases or above have been reported. Mutt et al. have classified these herniations into type A and type B depending on whether the disk herniates into the dura of the thecal sac or the nerve root sleeve.[2]

- Magnetic resonance imaging sagittal T2W imaging of the dorsolumbar spine showing an extra-axial lesion anterior to the neural elements, with widened CSF spaces both cranially and caudally
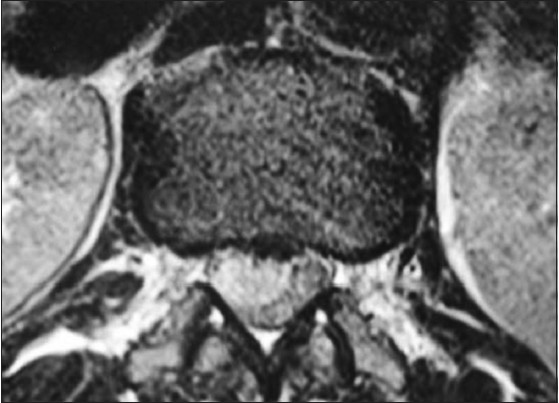
- Magnetic resonance imaging axial sections showing compression of the neural elements on the right side anteriorly
Various theories have been put forth concerning their etiopathogenesis and their occurrence is common at specific locations.
-
Altered annulus-PLL-dural interface, acting as a single membrane, which if associated with a narrowed spinal canal, is a situation good enough for the nucleus pulposus to egress and breach the dura. Perforation of the PLL and duramater is required for this herniation to occur. In the lumbar spine, the L4-L5 and L3-L4 levels are sites of predilection, and although rare, instances of cervical intradural disk herniations have also been published[3]
-
Fixation of the dural roots by the dural ligaments to the periosteum and disk results in fixation and limited mobility, and thus, predisposes for possible intradural extension. These adhesions can be congenital or acquired (following previous surgery).[4]
Many of the authors have tried to ascertain the importance of identifying this condition preoperatively with imaging studies, but were unsuccessful, and almost all of them were confirmed retrospectively. Such intradural disk herniations have been commonly described to occur in the lumbar region (92%), followed by the thoracic (5%) and cervical (3%) region.[5] Pertinent to this case, points of significance include the following: First, an extremely rare location of the transgressed fragment, that is, at the dorsolumbar junction. Second, a surprisingly short history of radiculopathy of just two weeks, which gives one the idea of the rapidity with which the disk has transgressed the dura, against the literature evidence where the symptoms are present for few months to year before presentation. Finally, there were neither identifiable adhesions at the dura-posterior longitudinal ligament interface nor any predisposing factors like a confined epidural space or previous surgeries at or adjacent to the level in context.
This case, apart from reiterating the importance of a transgressed disk as a possibility in the list of differentials for an intradural extramedullary lesion at the dorso-lumbar junction, compels one to think in terms of an altogether different possible mechanism, which could be unique to this region. Future biomechanical and pathogenetic studies particularly aimed at this level in a predisposed population could guide us to the cause.
References
- Intraradicular and intradural lumbar disc herniation: Experiences with nine cases. Surg Neurol. 1995;44:536-43.
- [Google Scholar]
- Intraradicular disc herniations in the lumbar spine and a new classification of intradural disc herniations. Spinal Cord. 2001;39:545-8.
- [Google Scholar]
- Anatomy and significance of fixation of the lumbosacral nerve roots in sciatica. Spine (Phila Pa 1976). 1983;8:672-9.
- [Google Scholar]
- Intradural disc herniations in the cervical, thoracic, and lumbar spine: Report of three cases and review of the literature. J Spinal Disord. 1990;3:396-403.
- [Google Scholar]





