Translate this page into:
Head banging persisting during adolescence: A case with polysomnographic findings
Address for correspondence: Dr. Ravi Gupta, Department of Psychiatry and Sleep Clinic, Himalayan Institute of Medical Sciences, Swami Ram Nagar, Doiwala, Dehradun - 248 140, Uttarakhand, India. E-mail: sleepdoc.ravi@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Head banging is a sleep-related rhythmic movement disorder of unknown etiology. It is common during infancy; however, available literature suggests that prevalence decreases dramatically after childhood. We report the case of a 16-year-old male who presented with head banging. The symptoms were interfering with his functioning and he had been injured because of the same in the past. We are presenting the video-polysomnographic data of the case. Possible differential diagnoses, etiology, and treatment modalities are discussed. The boy was prescribed clonazepam and followed up for 3 months. Parents did not report any episode afterward.
Keywords
Head banging
parasomnia
sleep-related rhythmic movement disorder
Introduction
Sleep-related rhythmic movement disorders (RMDs) usually manifests as body rocking, head banging, rolling of head, body, or leg, and lastly, banging of leg.[1] These movements involve large muscle groups and are often seen during drowsiness or sleep.[1] These movements are common in infants (prevalence nearly 60%), but their prevalence decreases to 5% by the age of 5 years.[1] Body rocking is most common, while head banging is least common presentation of RMD.[12] Head banging may cause injury to the child or sounds of banging may disturb the sleep of bed partner. These movements are considered a disorder when they interfere with sleep, induce significant functional impairment on the subsequent day, or result in bodily injury. In addition, these movements need to be differentiated from a number of conditions, most importantly, from nocturnal epilepsy.[13]
We are presenting a case of an adolescent who presented with head banging since childhood. The overnight recording by video-polysomnography confirmed the diagnosis.
Case Report
A 16-year-old boy presented with the complaints of hitting the bed or wall with his head during sleep, with a frequency of one or two nights per week. He was oblivious of what was happening in the night, but was informed by his parents regarding his abnormal activity during sleep. Because of the same reason, his parents did not allow him to spend night away from his home. Thus, it was interfering with his social life and he wanted medical help. On the other hand, parents sought consultation because they were worried about not only the abnormal activity during sleep but also the possibility of a head injury during these episodes.
The parents reported that this problem started at the age of 1 year where he would usually bang his head on the bed or pillow during sleep. Each episode would last about 2-5 min and was self-limiting. During these episodes, the child would assume prone position with knees close to his chest and then he would hit the bed or pillow or wall with his forehead. The movements were rhythmic and stereotyped. The episodes used to recur at varying intervals each night during which it was difficult to wake up the child. Often, the banging used to be so strong that the child had injured himself. A decrease in the frequency of the episodes was noticed after the age of 10 years. During childhood, the episodes were recurring at a frequency of three to five nights per week; but after the age of 10 years, they had reduced to one or two nights per week. Moreover, these episodes became limited to the second half of the night. Whenever he was woken up from these episodes, he reported amnesia regarding the movement.
The child was following a regular sleep schedule with bed time at around 11 p.m. He used to fall asleep easily and wake up by himself at around 6 a.m., feeling fresh. He regularly took 1-h nap during the day.
The child was born full term through normal delivery and achieved developmental milestones on time. He was attending 10th grade and was performing well in all academic activities at the time of presenting to us. He was well adjusted at school and enjoyed a good social circle. Medical and developmental histories were unremarkable. There was no history to suggest epilepsy, developmental delay, pervasive developmental disorder, substance abuse, or any other psychiatric illness. There was no history of any other type of stereotyped movement disorder during wakefulness or sleep. Chronic sleep deprivation, restless legs syndrome, sleep-talking, sleep-walking, sleep-related breathing disorder, narcolepsy, were also ruled out. The family history was negative for sleep disorder, epilepsy, neurological disorder, or psychiatric illness.
His neurological examination and mental status examination did not reveal any abnormality. Medical and Ear Nose and Throat (ENT) examinations were normal. His neck circumference at the level of cricothyroid was 32 cm, and his body mass index (BMI) was 20.08 kg/m2 , (height 158 cm, weight 50 kg). Awake electroencephalography (EEG) and computed tomography (CT) scan of Brain were normal.
A diagnosis of sleep-related RMD, head banging, was made and a video-synchronized full night polysomnography was ordered. The polysomnography was repeated on a second night since the child did not present any of the symptoms on the first trial. After the diagnosis was made, he was prescribed clonazepam 0.25 mg at bedtime and followed up for 3 months. Parents did not report any episode during this period.
Polysomnography
Polysomnography was performed with Easy III data acquisition system (Cadwell, Kennewick, WA, USA) using a standard montage.[4] Data were analyzed according to the American Academy of Sleep Medicine AASM guidelines.[4]
Analysis of polysomnographic data
Total sleep time was 416 min. Sleep-onset latency was 1 min. Wake time after sleep onset was 3 min. Morning report suggested usual quality sleep with sleep efficiency of 99%. Rapid eye movement sleep (REM) latency was reduced (47 min). Hypnogram suggested usual stage shifting during the night. Length and amount of different sleep stages were adequate. Arousal Index during the test night was 0. The patient rested in supine position without frequent changes. The study ruled out sleep-related breathing disorder, with a respiratory disturbance index (RDI) of 2 (all were post-arousal central sleep apneas). Occasional limb movements were observed during sleep, with the periodic limb movements during sleep (PLMS) index of 7. Electrocardiogram did not show any abnormality. Rhythmic movements of 1 Hz were seen during stage 2 sleep [Figure 1]. The child scratched his cheek and assumed the frog-like posture with knees below abdomen and arms folded. He then started banging his head on the pillow for nearly 2 min. Then he woke up and laid down on the bed again. The movements were rhythmic [Video]. Alpha activity in posterior leads and predominantly theta activity with movement artifacts (1 Hz) was seen in frontal leads [Figure 1]. No epileptiform activity was observed [Figure 1].
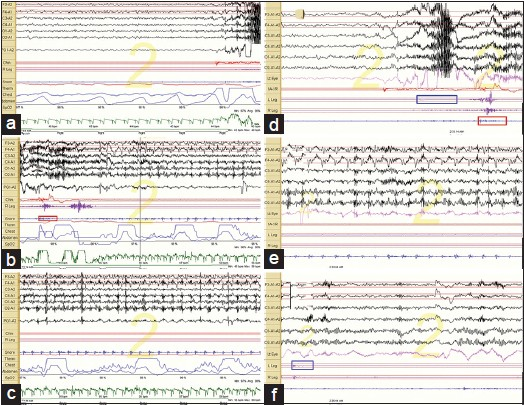
- (a) 30-s epoch shows movement originating from N2 sleep; (b) 30-s epoch shows change of body position; (c) 30-s epoch shows alpha in posterior leads and persistent slowing in central and frontal leads, with movement artifacts; (d) 20-s epoch shows normal EEG before the onset of movements; (e) 20-s epoch shows persistent slow waves in central and frontal leads with absent epileptiform activity; (f) 20-s epoch shows normal EEG after the episode
Discussion
This case presented with frequent abnormal head movements during sleep since childhood, with a significant decrease over time. The movements were stereotyped, rhythmic, and involved large muscle groups. These movements had resulted once in an injury and were disrupting his social functioning, e.g., he was not able to attend family functions or school camps. Thus, all the criteria for RMDs were met.[1]
A number of other sleep disorders may mimic RMD and it can also be seen along with a number of psychiatric conditions. Though the movements in some sleep disorders, viz., bruxism, sucking of thumb or lips during sleep, and hypnagogic foot tremor, are rhythmic and stereotyped, yet these movements should not be confused with RMD.[1] Unlike these disorders, movements in RMD are usually complex and involve large muscle groups.[1] RMD has been reported in association with a range of psychiatric conditions, e.g., intellectual disability (ID), pervasive developmental disorder (PDD), and attention deficit hyperactivity disorder (ADHD).[15] In these patients, rhythmic movements are predominantly seen during wakefulness, which was not reported by the informants in the present case.[1] In addition, in subjects with ID and PDD, RMD may persist even during adulthood.[1] Contrarily, in subjects with normal intelligence, RMD usually improve by childhood.[1] Though rare, similar to the present case, adult cases of sleep-related RMD with normal intelligence have also been reported.[2] Still, we suggest that ID, PDD, and other psychiatric disorders must be ruled out in adult patients with sleep-related RMD.
Another important differential diagnosis for sleep-related RMD is nocturnal epilepsy, particularly, nocturnal frontal lobe epilepsy (NFLE).[36] A number of clinical and electrophysiological characteristics can be used to differentiate NFLE from parasomnia or RMD, e.g., clustering, semiology, timing, duration, stereotypy, and age of onset.[78] NFLE may start in childhood or adulthood, and manifests as short-spanned stereotyped movements occurring multiple times in a night or during wakefulness.[36] Contrarily, sleep-related RMDs are of relatively longer duration and appear only during sleep, particularly, stage 2 sleep.[3] However, sometimes RMD may develop during the transition stage of sleep and wakefulness or during REM sleep also.[9] In the present case, rhythmic movements occurred only during sleep (stage 2 sleep); these movements had a span of approximately 2 min and were present since infancy, thus favoring the diagnosis of RMD. In addition, NFLE patients may show abnormal EEG activity during the episode.[6] However, if few leads are used or the locus of epileptiform activity is deep, then epileptiform activity may not be identified with surface EEG even with international 10-20 system.[78] In such cases, brain functional neuroimaging during ictus may help clarifying the diagnosis.[78] Although the routine polysomnographic EEG electrode placement might miss the epileptiform activity in this patient, a diagnosis of NFLE is highly improbable based on the presence of the complex repetitive behavior, which so far has never been described in this condition (see video).[8]
RMD may also be considered as one type of parasomnia. Parasomnias are complex behaviors that occur during sleep.[1] Parasomnias may occur during slow-wave sleep, e.g., sleep-walking, sleep-talking, or during REM sleep, viz., REM sleep behavior disorder.[13] They are usually preceded by a brief arousal phenomenon, are of longer duration than epilepsy, and often terminate with arousal or light sleep.[78] As often seen during slow-wave-sleep parasomnias, electroencephalographic dissociation was seen in the present case (vide infra). Absence of any motor activity during stage 3 sleep and presence of muscle atonia during REM ruled out the disorders of arousal and REM sleep behavior disorder, respectively, in this case.[13] Since slow-wave sleep parasomnias occur during brief arousals from sleep, any sleep disorder that interferes with the maintenance of sleep can give rise to parasomnia. This is why some patients with sleep apnea develop RMD at the termination of apnea when the apneic events are associated with an arousal. It also explains why therapy of the underlying disorder, e.g., continuous positive airway pressure (CPAP), in cases of sleep apnea improve RMD.[2] However, RMD in the present case was not related to any other sleep disorder.
The etiology of RMD is still unknown and a number of hypotheses have been proposed to describe its etiopathogenesis.[291011] While some consider it as a learned behavior to sooth oneself during sleep, other hypothesis advocates the role of genetic factors, as in some cases, RMD can be familial.[91011] Meyer et al.[2] proposed that RMD could be related to male hormones as they found a male predominance in adult population with RMD. It could be related to the arousals from sleep, but is usually not considered a disorder of arousal.[2] In short, still more research is required to find out the etiopathogenesis of RMD. Diagnosis of RMD requires video-synchronized whole night attended polysomnography, similar to what was done in the present case. As discussed above, these complex movements may be a manifestation of REM sleep behavior disorder rather than RMDs which are seen during non-rapid-eye-movement NREM sleep.[11] The examination of the polysomnography recording of RMD usually reveals the presence of muscle artifacts along with movement artifacts, without arousal.[2] The examination of sleep record in the present case shows that the occipital rhythm was alpha, suggesting arousal, while slowing was seen in the frontal leads, suggesting persistent sleep during the episode [Figure 1]. Thus, similar to NREM parasomnias, dissociation between the occipital and frontal electrical activity during the episode was seen.[12] Thus, we propose that RMD could be a type of NREM sleep parasomnia.
A number of therapeutic modalities have been found effective in the treatment of RMD, but it largely depends upon co-morbid sleep disorder. In subjects without co-morbid sleep apnea, clonazepam at bed time has been found effective in RMD.[131415] On the other hand, as already discussed, CPAP therapy has also been found to reduce the frequency of RMD in cases with co-morbid sleep apnea.[216] In the present case, co-morbid sleep disorders were ruled out; hence, clonazepam was chosen. Clonazepam 0.25 mg at bed time resulted in amelioration of symptoms in the present case. We assume that by reducing the arousals, clonazepam improved the maintenance of sleep in the present case and thus was effective in the management of RMD.[213141516] Thus, this case favors the arousal hypothesis of RMD. Arousal hypothesis is further supported by Attarian et al.'s report that described RMD in three successive generations and argued that inability to maintain continuous sleep could be an underlying pathology.[17] However, since the cases were seen in a family, this report does not exclude the hypothesis of learned behavior or genetic etiology.[17] Due to the lack of understanding of the pathophysiology of RMD, guidelines for the management of RMD are not available.
To conclude, the available literature suggests that RMD should be diagnosed with the help of attended video-polysomnography after ruling out co-morbid psychiatric and sleep disorders. Adequate management of underlying co-morbid sleep disorder or drugs that improve the maintenance of sleep may help in the management of RMD.
Video on available at: www.ruralneuropractice.com
Source of Support: Nil.
Conflict of Interest: None declared.
References
- American Academy of Sleep Medicine. International Classification of Sleep Disorders. In: Diagnostic and Coding Manual (2nd ed). Westchester, IL: American Academy of Sleep Medicine; 2005.
- [Google Scholar]
- Iber C, Ancoli-Israel S, Chesson A, Quan SF, eds. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, terminology, and technical specification (1st ed). Westchester, IL: American Academy of Sleep Medicine; 2007.
- Review of the possible relationship and hypothetical links between attention deficit hyperactivity disorder (ADHD) and the simple sleep related movement disorders, parasomnias, hypersomnias, and circadian rhythm disorders. J Clin Sleep Med. 2008;4:591-600.
- [Google Scholar]
- Differentiating parasomnias from nocturnal seizures. J Clin Sleep Med. 2012;8:108-12.
- [Google Scholar]
- NREM arousal parasomnias and their distinction from nocturnal frontal lobe epilepsy: A video EEG analysis. Sleep. 2009;32:1637-44.
- [Google Scholar]
- Other parasomnias. In: Kryger MH, Dement W, Roth T, eds. Principles and practice of sleep medicine. St Louis, Missouri: Elsevier Saunders; 2011. p. :1098-105.
- [Google Scholar]
- A multigenerational family with persistent sleep related rhythmic movement disorder (RMD) and insomnia. J Clin Sleep Med. 2009;5:571-2.
- [Google Scholar]
- Association of idiopathic rapid eye movement sleep behavior disorder in an adult with persistent, childhood onset rhythmic movement disorder. J Clin Sleep Med. 2009;5:374-5.
- [Google Scholar]
- Physiopathogenetic interrelationship between nocturnal frontal lobe epilepsy and NREM arousal parasomnias. Epilepsy Res Treat. 2012;2012:312693.
- [Google Scholar]
- Atypical headbanging presentation of idiopathic sleep related rhythmic movement disorder: Three cases with video-polysomnographic documentation. J Clin Sleep Med. 2012;8:403-11.
- [Google Scholar]
- Association of body rolling, leg rolling, and rhythmic feet movements in a young adult: A video-polysomnographic study performed before and after one night of clonazepam. Mov Disord. 2008;23:602-7.
- [Google Scholar]
- Rhythmic movement disorder associated with respiratory arousals and improved by CPAP titration in a patient with restless legs syndrome and sleep apnea. Sleep Med. 2009;10:501-3.
- [Google Scholar]
- A multigenerational family with persistent sleep related rhythmic movement disorder (RMD) and insomnia. J Clin Sleep Med. 2009;5:571-2.
- [Google Scholar]






