Translate this page into:
Glioblastoma Masquerading as a Parafalcine Meningioma: A Pathological Surprise!
Chittur Viswanathan Gopalakrishnan, MS, MCh Department of Neurosurgery, Aster Medcity Kuttisahib Road, Cheranalloor, Kochi India drgopal1976@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
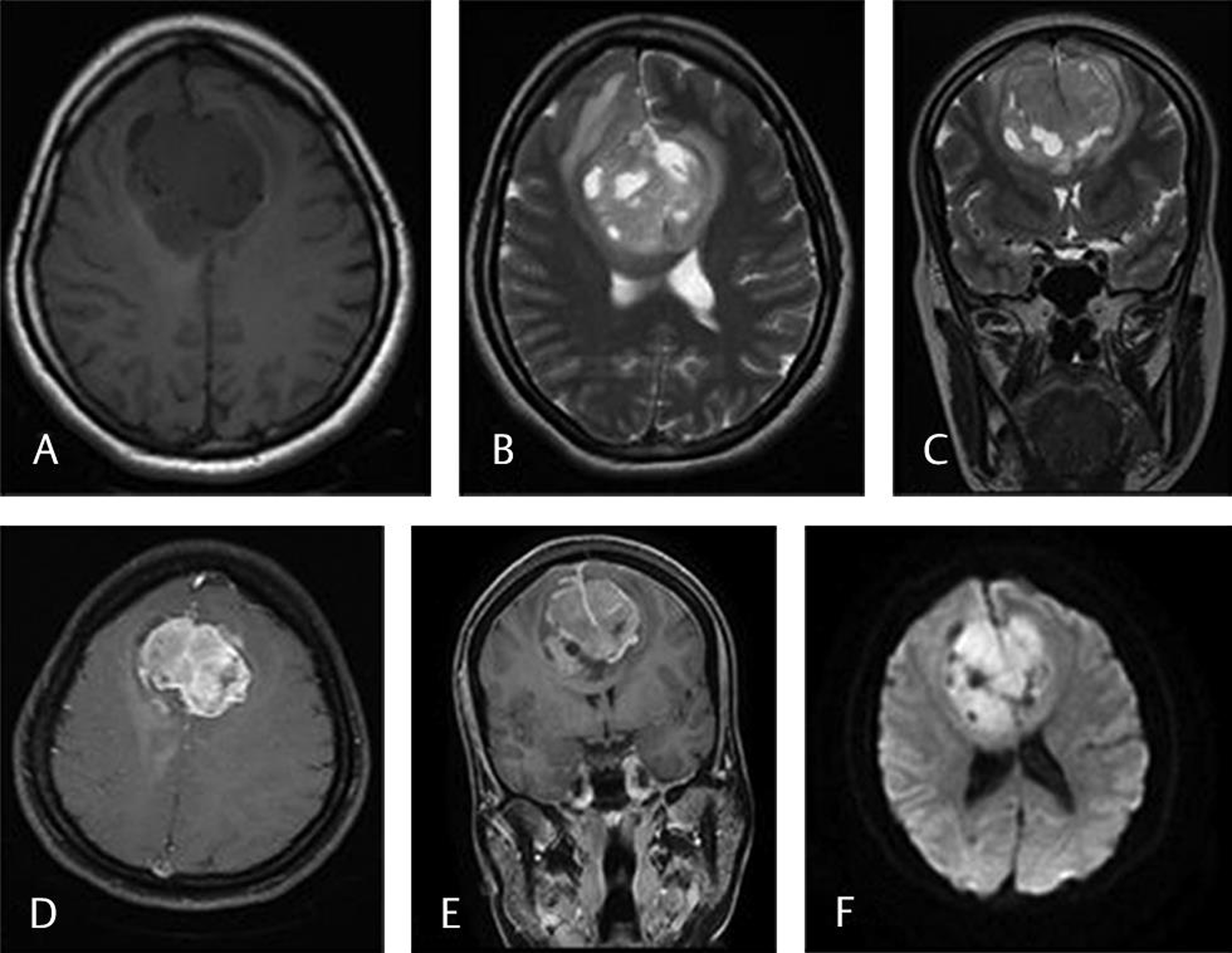
A 30-year-old female presented with an acute history of left-sided focal seizures with secondary generalization. Magnetic resonance imaging (MRI) of the brain (Fig. 1) revealed a large tumor attached to mid one-third of the falx cerebri with extension to either sides, a heterogeneous contrast enhancement (Fig. 1D E) and presence of extensive peritumoral edema. A provisional diagnosis of mid one-third falx meningioma was made, and the patient underwent bifrontal craniotomy and excision of the lesion.
-
Fig. 1 T1 (A) and T2 (B) weighted axial MRI show a large heterogeneous tumor encasing the falx and extending into both the cerebral hemispheres. There is perilesional edema with buckling of the cortex on coronal T2W (C) image. The attachment to the falx with its enhancement is seen in postcontrast T1W axial (D) and coronal (E) MRI. Diffusion weighted imaging (F) shows areas of restricted diffusion within the tumor. MRI, magnetic resonance imaging.
Fig. 1 T1 (A) and T2 (B) weighted axial MRI show a large heterogeneous tumor encasing the falx and extending into both the cerebral hemispheres. There is perilesional edema with buckling of the cortex on coronal T2W (C) image. The attachment to the falx with its enhancement is seen in postcontrast T1W axial (D) and coronal (E) MRI. Diffusion weighted imaging (F) shows areas of restricted diffusion within the tumor. MRI, magnetic resonance imaging.
Intraoperatively, the tumor was greyish, soft to firm, vascular, and adherent to the falx. The pial plane between the tumor and the parenchyma was breached along with multiple pial feeders. The falx was excised along with the tumor.
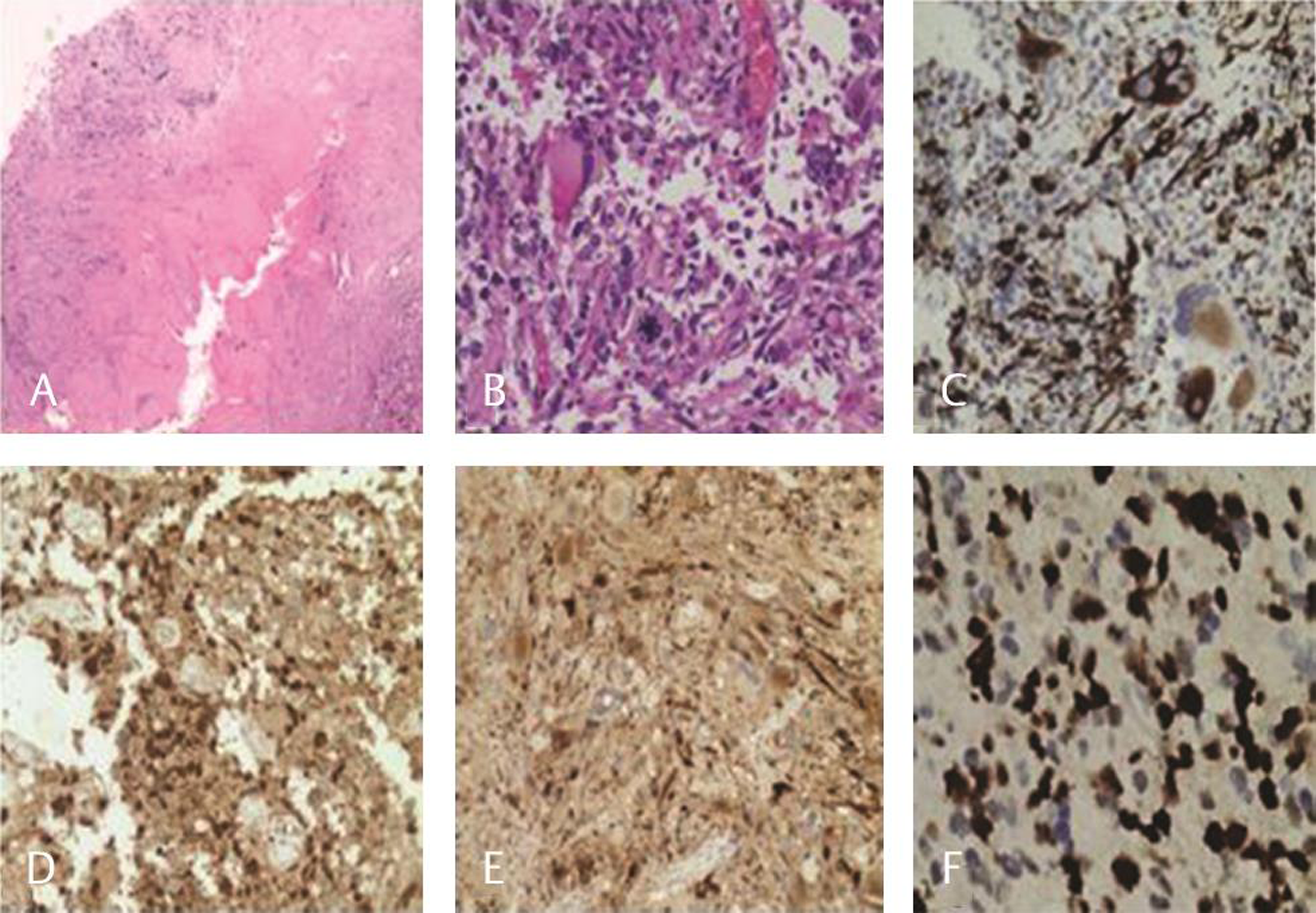
The histopathology showed a cellular neoplasm attached to the dural collagen (Fig. 2A) with highly pleomorphic cells, hyperchromatic nuclei, intranuclear pseudoinclusions, and fibrillary cytoplasm with atypical mitosis (Fig. 2b) and necrosis. The immunohistochemistry showed strong glial fibrillary acidic protein and S-100 in tumor cells with coexpression of epithelial membrane antigen and retained nuclear ATRX (alpha thalassemia/mental retardation syndrome X linked gene mutation) gene mutation. In immunohistochemistry, IDH1 (R132H) was negative and p53 was not expressed. The Ki-67 proliferation index was 30%. The diagnosis of glioblastoma multiforme, isocitrate dehydrogenase-wild type, World Health Organization grade IV was confirmed.
-
Fig. 2 Cellular neoplasm attached to dural collagen (A, H&E, ×20); markedly pleomorphic cells with atypical mitosis (B, H&E ×400); immunohistochemical expression of glial fibrillary acidic protein in tumor cells (C); S-100, (D) epithelial membrane antigen (E) and high MIB-1 proliferation index (F). H&E, hematoxylin and eosin.
Fig. 2 Cellular neoplasm attached to dural collagen (A, H&E, ×20); markedly pleomorphic cells with atypical mitosis (B, H&E ×400); immunohistochemical expression of glial fibrillary acidic protein in tumor cells (C); S-100, (D) epithelial membrane antigen (E) and high MIB-1 proliferation index (F). H&E, hematoxylin and eosin.
As originally proposed by Cushing, falx meningiomas are tumors arising from the falx cerebri covered by the overlying cortex.1 Falx meningiomas predominately have a propensity for unilateral extension but can often be bilateral and dumb-bell shaped.2 Falx meningiomas are divided into two types: internal and external. The former originates from the inferior sagittal sinus and the later from the body of the falx.3
There have been case reports in literature where glioblastoma multiforme (GBMs) at different locations have mimicked a meningioma on imaging.4 Many of the times, it is often an intraoperative and pathological surprise. In MRI, meningiomas and GBMs can often be differentiated due to their characteristic appearances (Table 1). But rarely one may mimic the other causing a pathological surprise.
|
Radiologic features on MRI |
Meningioma |
Glioblastoma |
|---|---|---|
|
Abbreviations: CSF, cerebrospinal fluid; MRI, magnetic resonance imaging. |
||
|
General |
Well-defined extra-axial tumor |
Intra-axial irregular mass |
|
Extra-axial mass vs. intra-axial mass |
CSF cleft sign Broad dural base Displaced subarachnoid vessels Bony hyperostosis Expand subarachnoid space White matter buckling sign |
Thickened nonenhancing cortex with increased T2 signal Expansion of nearby gyri (this is the opposite of the white matter buckling sign) Thickening of the corpus callosum |
|
On contrast administration |
Uniform contrast enhancement |
Ring enhancing contrast enhancement with central necrosis |
|
Vasogenic edema |
Can be present |
Profound vasogenic edema |
|
Bony changes |
Bone hyperostosis and meninges show dural tail sign |
No obvious bony changes |
|
Midline crossing |
Can involve the meninges causing contralateral extension |
Can involve the corpus callosum and spread to the opposite side |
|
Local tumor spread |
Pressure effect on the surrounding brain is more |
Less pressure effect in comparison to their size |
In our case, on retrospective review of the images, there were some points against a diagnosis of an extra-axial lesion. The symmetrical extent of the tumor on either side of the falx, the extensive pial breach especially in the anterior cingulate, the heterogeneity on contrast possibly suggesting areas of necrosis, and nonvisualization of a definite cerebrospinal fluid cleft surrounding the tumor should have raised the suspicion of a high grade intrinsic tumor preoperatively. The prognosis of these two totally diverse pathological entities is different, and therefore, the recognition is of utmost importance. It helps in surgical planning and patient counseling prior to surgery.
This report highlights the importance of keeping in mind a differential diagnosis of an alternate pathology when the MRI features are ambiguous. Additional MRI sequences like magnetic resonance spectroscopy and MR perfusion can often help in clinching the diagnosis preoperatively rather than a histological surprise later on.
Note
The work was primarily performed at Aster Medcity, Kochi, Kerala.
Conflict of Interest
None declared.
References
- . 1938;27(2):185. Their classification, regional behavior, life history, and surgical end results. Bull Med Libr Assoc
- Falx meningiomas: surgical results and lessons learned from 68 cases. J Korean Neurosurg Soc. 2007;42(4):276-280.
- [Google Scholar]
- Microneurosurgery of CNS Tumors, IV-B. Stuttgart: Georg Thiem Verlag; 1996. p. :134-165.
- [Google Scholar]
- Glioblastoma mimicking meningioma: report of 2 cases. World Neurosurg. 2016;95:624.e9-624.e13.
- [Google Scholar]
- Smithuis R, Montanera W. The radiology assistant: systematic approach. radiologyassistant. Available at: https://radiologyassistant.nl/neuroradiology/brain-tumor/systematic-approach. Published 2008





