Translate this page into:
Giant Bilateral Calvarial Hyperostosis Secondary to Small Unilateral Frontal Meningioma
Address for correspondence: Dr. Satyashiva Munjal, Department of Neurosurgery, Paras Hospitals, Sector 43, Sushant Lok, Gurugram - 122 002, Haryana, India. E-mail: satyashivamunjal@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A 28-year-old male patient presented to us with bilateral frontal hyperostosis associated with a small unilateral frontal intracranial meningioma. He underwent successful excision of the involved bone and repair of the large cranial defect using a titanium mesh. Histological examination revealed tumor infiltration of the overlying bone. Surgical challenges in the management of such a case are also discussed.
Keywords
Bilateral
calvarial hyperostosis
unilateral meningioma
INTRODUCTION
Meningiomas account for 20%–25% of all tumors of the central nervous system.[12] Hyperostosis is seen in 4.5% of all cases of meningiomas.[23] Bone invasion by tumor cells is a commonly accepted mechanism. We present a rare case of a 28-year-old male who presented to us with bilateral frontal extensive calvarial hyperostosis associated with a unilateral frontal meningioma.
CASE REPORT
A 28-year-old male presented to us with progressively increasing frontal bossing since childhood. It was insidious in onset, initially on the left side but progressively increased to involve the other sides. He also complained of headache for past 6 months which was insidious in onset, frontal in location, mild-to-moderate intensity to begin with, increased in intensity, and frequency over the past 2 months. It used to usually occur in early morning and get relieved by vomiting. There was no history of loss of consciousness, seizure, or any other neurological deficits. On examination, the patient had a large frontal protuberance extending from the middle of the forehead up to the vertex. It was asymmetrically more on the left side. Rest of the examination was unremarkable. Computed tomography head [Figure 1] done showed contrast-enhancing dural-based lesion in left frontal lobe with perilesional edema suggestive of a meningioma. Overlying frontal bone [Figure 2] showed marked hyperostosis with “sunburst appearance.” The hyperostosis is seen to cross the midline and extend to the opposite side. He underwent a bifrontal craniotomy (using a bi-coronal scalp flap) and Simpson Grade 1 excision of the meningioma. The pericranium appeared to be infiltrated by the tumor. Craniotomy was made using multiple burr holes. Frontal bone was thick, highly vascular, and was densely adherent to the underlying dura on the left side. Tumor was soft to firm, extra-axial, highly vascular, and suckable suggestive of a meningioma. Simpson Grade 1 excision was done. Duraplasty was done with tensor fascia lata graft. Bifrontal cranial defect was repaired with titanium mesh [Figure 3]. The patient had an uneventful postoperative stay and was discharged on postoperative day 10. Histopathologic examination [Figure 4] of the tumor revealed sheets and whorls of spindle to meningothelial cells with mild nuclear atypia. Occasional psammoma bodies were observed. The findings were suggestive of Grade 1 meningioma. Both the pericranium and bone were infiltrated by the tumor cells.
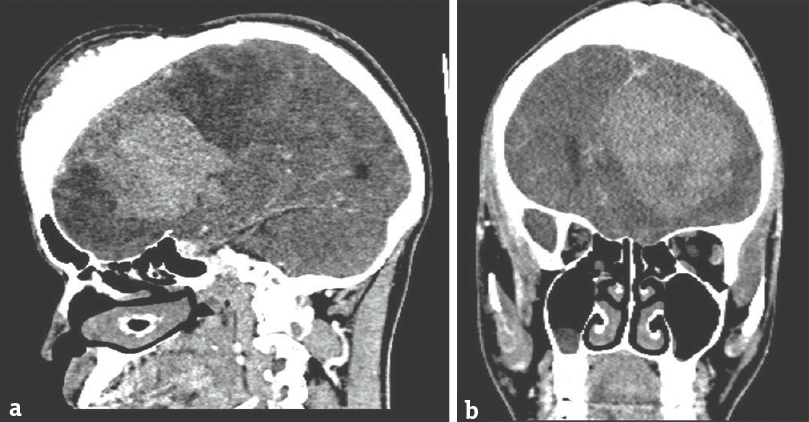
- (a and b) Contrast-enhanced computed tomography head showing contrast-enhancing unilateral dural-based extra-axial frontal space-occupying lesion suggestive of meningioma
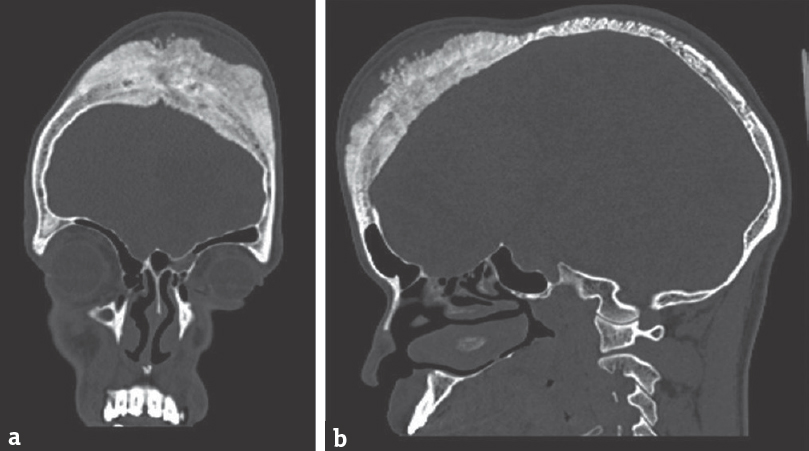
- (a and b) Computed tomography bone cuts showing extensive bilateral calvarial hyperostosis
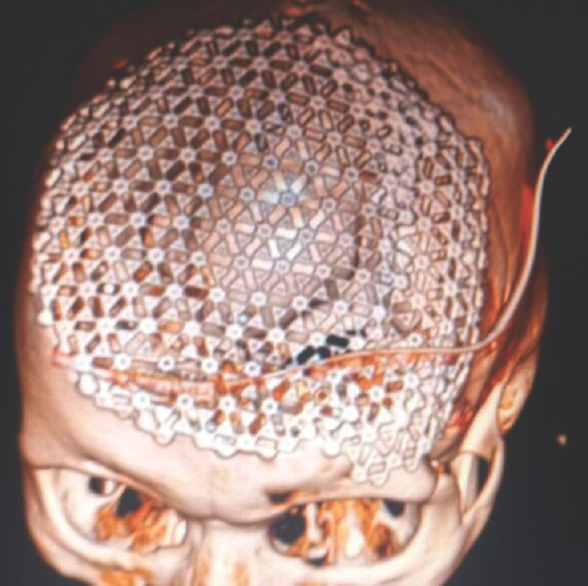
- Postoperative computed tomography (three-dimensional reconstruction) showing repair of cranial defect using titanium mesh
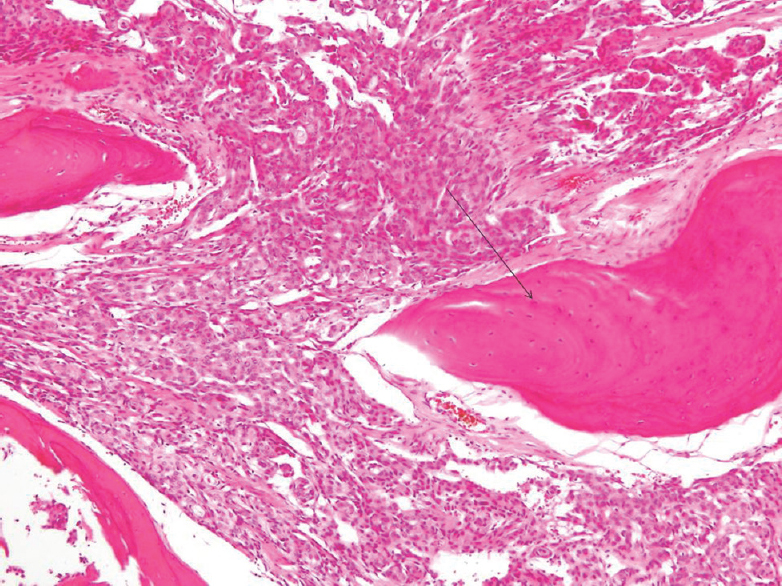
- Histopathology examination showing sheets and whorls of tumor cells (meningioma) infiltrating bone (arrow)
DISCUSSION
Meningiomas account for about 20%–25% of all central nervous system tumors.[12] They are usually slow growing and can insidiously attain a large size before producing clinical symptoms. Associated calvarial hyperostosis is seen in 4.5% of cases of meningiomas.[23] En plaque meningiomas are associated with a higher incidence of hyperostosis, reported between 13% and 49%.[4] Primary intraosseous meningioma is associated with hyperostosis in 60% of cases.[34] The histological type of meningioma does not seem to relate to extent or incidence of hyperostosis.[2]
Etiology of associated hyperostosis in meningioma is controversial. Whether it is due to direct infiltration of bone by the tumor cells or due to secondary changes in the bone induced by the tumor is a point of debate.[235] Histological demonstration of infiltration of bone by tumor cells has been demonstrated by various authors and is the commonly accepted mechanism.[24] In our case too, tumor cells were found to infiltrate the bone as well as overlying pericranium.
Usually, calvarial hyperostosis is smaller than the associated meningioma, but in our case, large bifrontal calvarial hyperostosis was associated with a relatively small left frontal convexity meningioma which raises doubts over the “infiltration theory.” Other proposed alternative mechanisms which may play a role are preceding trauma, irritation of the bone by the tumor without actual invasion, stimulation of osteoblasts by factors secreted by tumor cells, production of bone by tumor itself, and vascular changes caused by the tumor.[5]
In 1934, Echlin proposed an association between hyperostosis and direct infiltration of the bone by tumor cells which has been seconded by various authors since then.[6] Pieper et al. demonstrated on histology that hyperostosis in tumors of cranial base is a result of direct tumor invasion.[1] However, it must be borne in mind; hyperostosis is not always associated with tumor invasion. According to Pei et al., increased expression of matrix metalloproteinases (MMP)-13 and membrane Type 1 MMP may contribute to hyperostosis.[5]
Bilateral extensive frontal bone hyperostosis in such case is a surgical challenge. Wide excision of the involved bone must be done to reduce the incidence of recurrence. In our case, extensive removal of involved bone was done. Preoperative embolization may be done to reduce the vascularity of the bone and the tumor. The cranial defect may be repaired by artificial bone cement or a titanium mesh.
CONCLUSION
Hyperostosis is commonly associated with meningiomas. Exact mechanism is not known, but invasion of bone by the tumor cells is the most likely cause. In some cases, extensive hyperostosis may be associated with a small intracranial tumor. Wide resection of the bone must be done in such cases to reduce recurrence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Hyperostosis associated with meningioma of the cranial base: Secondary changes or tumor invasion. Neurosurgery. 1999;44:742-6.
- [Google Scholar]
- Does bony hyperostosis in intracranial meningioma signify tumor invasion? A radio-pathologic study. Neurol India. 2012;60:50-4.
- [Google Scholar]
- Hyperostotic meningioma with minimal tumor invasion into the skull. Neurol Med Chir (Tokyo). 2005;45:480-3.
- [Google Scholar]
- Giant calvarial hyperostosis with biparasagittal en plaque meningioma. Neurol India. 2006;54:210-2.
- [Google Scholar]
- Possible role of matrix metalloproteinases (MMPs) in hyperostosis of intracranial meningiomas. Acta Neurochir (Wien). 2012;154:611-20.
- [Google Scholar]
- Cranial osteomas and hyperostoses produced by meningeal fibroblastomas. Arch Surg. 1934;28:357-405.
- [Google Scholar]






