Translate this page into:
Frontal Bone Hemangioma in an 8-year-old Female: A Common Tumor in a Rare Location
Address for correspondence: Dr. Abhimanyu Sharma, Department of Pathology, University College of Medical Sciences and Guru Tegh Bahadur Hospital, Dilshad Garden, New Delhi - 110 095, India. E-mail: abhimanyu20s@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Intraosseous hemangioma is a rare bone tumor accounting for 0.7%–1.0% of all bone tumors. In the skull, frontal bone is the commonly involved bone. An 8-year-old female presented to our outpatient department with complaints of pain and swelling over forehead for 4 months. X-ray revealed a lytic expansile lesion involving frontal bone with sunburst pattern of bony spicules radiating to periphery of the lesion. Magnetic resonance imaging revealed the presence of a well-circumscribed lesion with both intra as well as extracranial components. Histopathology revealed a vascular tumor consisting of both small (capillary) and large (cavernous) sized vessels. A diagnosis of mixed type of hemangioma of the frontal bone was given. Recognition of hemangioma on radiology and confirmation by histopathology is essential for proper management as it might be confused clinically with other locally aggressive/malignant lesions.
Keywords
Bone neoplasms
frontal bone
hemangioma
INTRODUCTION
Intraosseous hemangioma is a rare bone tumor accounting for 0.7%–1.0% of all bone tumors.[1] These tumors are mostly found in vertebral bodies and are rarely seen in the calvarium, where they represent 0.2% of bony neoplasms.[2]
According to Heckl et al., among the calvarial bones, the frontal bone is the most commonly involved.[3] The peak age incidence is in the fourth decade although pediatric case has been described.[4]
CASE REPORT
An 8-year-old female presented to our outpatient department with complaints of pain and swelling over forehead for 4 months. The swelling gradually progressed in size, had a bony consistency, and was nontender. There was no history of trauma. X-ray revealed a lytic expansile lesion involving frontal bone with sunburst pattern of bony spicules radiating to periphery of the lesion [Figure 1]. Magnetic resonance (MR) imaging revealed the presence of a well-circumscribed lesion with both intra as well as extracranial components, involving frontal bone in the midline. The lesion showed heterogeneous signal intensity on T2-weighted images and showed vivid, heterogeneous contrast enhancement. The lesion caused mass effect and edema in the right frontal lobe. However, there was no evidence of intraparenchymal infiltration with clear demarcation from galea and dura mater (linear hypointensity on outer and inner aspect, respectively) [Figure 2]. An en bloc resection was performed for the patient with adequate margins. Surgery was done in view of mass effect, increase in size of the lesion, and perilesional edema.

- X-ray shows a lytic lesion involving frontal bone with sunburst pattern of bony spicules radiating to periphery of lesion
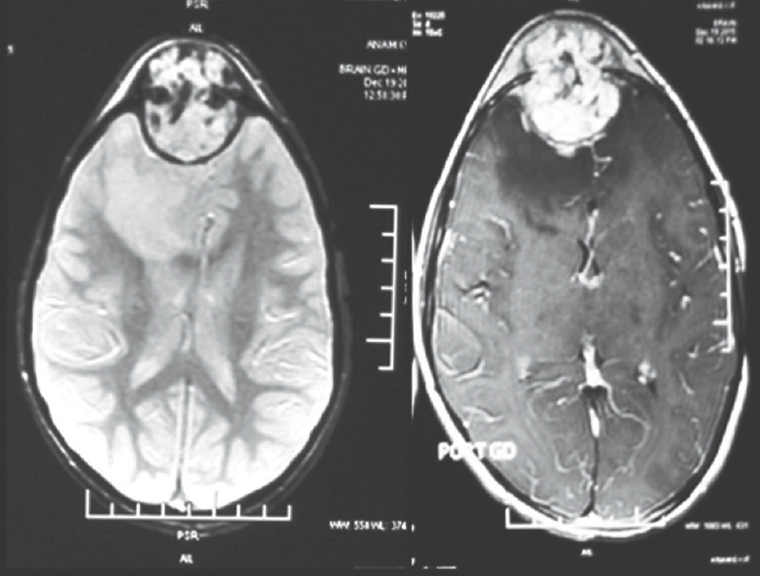
- Magnetic resonance imaging showing a well-circumscribed lesion involving frontal bone in the midline showing heterogeneous signal intensity on T2-weighted images. The lesion is causing mass effect and edema in the right frontal lobe. However, there is no evidence of intraparenchymal infiltration with clear demarcation from galea and dura mater
Histopathology
We received a focally expanded bony piece measuring 9 cm × 5 cm × 4.5 cm. Cut surface revealed a well-circumscribed variegated lesion measuring 7 cm × 5 cm × 4.5 cm with cystic areas filled with blood. Hematoxylin and eosin sections after decalcification revealed a vascular tumor consisting of both small (capillary) and large (cavernous) sized vessels [Figure 3]. The vessels were arranged predominantly in the form of lobules, but at places, they were present in a loose edematous stroma [Figure 3]. The vessels were variably shaped with a single layer of endothelial cells without any shedding. The lumen consisted predominantly of red blood corpuscles. The endothelial cells were oval to comma shaped with round to oval nucleus with condensed chromatin and inconspicuous nucleoli. Anaplasia and mitoses were not seen. Based on the above findings, a diagnosis of mixed type of hemangioma of the frontal bone was given.
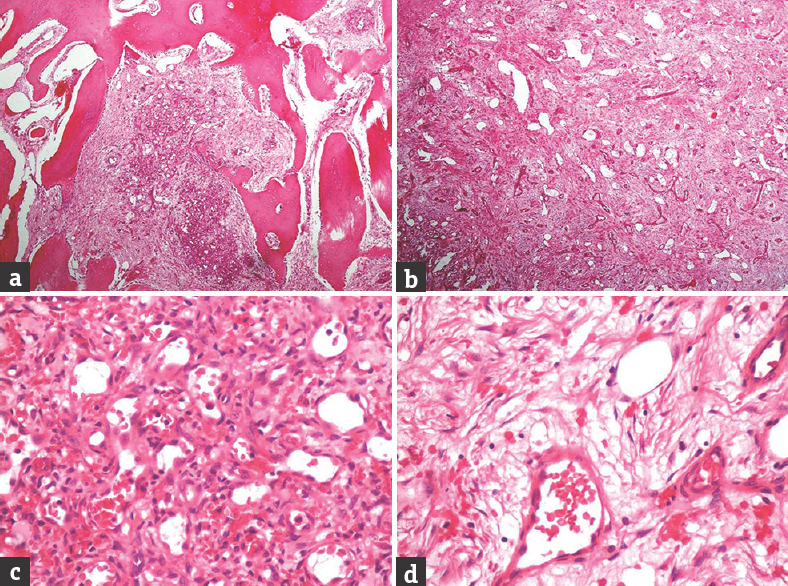
- Microscopy of frontal bone hemangioma. (a) Microscopy showing both small- and large-sized vessels along with bony trabeculae (H and E, ×40). (b) Microscopy showing both small- and large-sized vessels in loose edematous stroma (H and E, ×40). (c) Microscopy showing small-sized vessels with single layer of endothelial cells and red blood cells within the lumen (H and E, ×400). (d) Microscopy showing vessels in edematous stroma with red blood cells within the lumen (H and E, ×400)
DISCUSSION
Intraosseous hemangioma usually presents as a bony swelling. The pathogenesis of primary intraosseous hemangioma remains unknown. Trauma is considered to be the most important etiology of this tumor.[1] Our case had a bony swelling such as other reviewed cases[12] but did not have any history of trauma. Clinicoradiologically, the differential diagnosis included hemangioma, eosinophilic granuloma, and osteosarcoma. On computed tomography (CT), eosinophilic granuloma appears as a punched-out osteolytic lesion without sclerotic rim or periosteal reaction. Its edges may be beveled, due to usually asymmetric involvement of the outer and inner tables.[5] These features were not seen in our case. However, histology is essential to rule out the possibility of eosinophilic granuloma. Osteosarcoma shows prominent periosteal reaction and a wide zone of transition which were not seen in our case.
On radiology, most cases of calvarial hemangioma usually erode only the outer table,[6] but in our case, both the inner and outer tables of calvarium were eroded. Calvarial hemangiomas are usually seen as a lytic lesion with a sclerotic rim in a honeycomb or sunburst-like appearance on skull radiographs.[12] Further evaluations with CT confirm and substantiate the findings of plain film because of its ability to delineate cortical and trabecular details. On T1-weighted MR images, a heterogeneously hypo- to iso-intense mass is seen, and on T2-weighted MR images, a heterogeneously hyperintense mass is seen. The lesion enhances diffusely and heterogeneously after contrast medium administration.[126] The above findings are similar to what we found in our patient.
Histologically, Mirra divided hemangiomas of bone and soft tissues into five variants:[7]
-
Capillary
-
Cavernous
-
Mixed
-
Cellular
-
Histiocytoid.
In the reviewed cases of intraosseous hemangioma of the skull bones, the histological pattern was either capillary or cavernous.[1267] Our case had morphology of mixed type of hemangioma with both capillary and cavernous vessels. The treatment of choice for intraosseous hemangioma is en bloc resection with an adequate normal bone margin which was done in our case.[1]
Our case was an 8-year-old female which is an uncommon age for presentation of such a tumor. Moreover, we had a mixed type of morphology on histopathology, with both capillary and cavernous vessels, which is an uncommon feature. Pathological differential diagnosis includes intermediate grade and malignant vascular tumors of bone such as hemangioendothelioma and angiosarcoma. In our case, the vascular spaces were lined by a single layer of endothelial cells favoring the possibility of hemangioma. There was absence of high cellularity, solid areas, hobnail cells, syncytial or papillary clusters, and shedding of individual and clusters of cells into the lumen which is seen in angiosarcoma/hemangioendothelioma.[8] Anaplasia and mitosis which are usually seen in angiosarcoma were not seen in our case leading to the final diagnosis of hemangioma of the frontal bone.
To conclude, recognition of hemangioma on radiology and confirmation by histopathology is essential for proper management as it might be confused clinically with other locally aggressive/malignant lesions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Primary intraosseous hemangioma in the frontal bone. Arch Plast Surg. 2013;40:283-5.
- [Google Scholar]
- Primary intraosseous cavernous hemangioma of the clivus: Case report and review of the literature. J Neurol Surg Rep. 2013;74:17-22.
- [Google Scholar]
- Cavernomas of the skull: Review of the literature 1975-2000. Neurosurg Rev. 2002;25:56-62.
- [Google Scholar]
- Congenital cavernous hemangioma of the calvaria. Case report. J Neurosurg Pediatr. 2009;3:41-5.
- [Google Scholar]
- Calvarial lesions: A radiological approach to diagnosis. Acta Radiol. 2009;50:531-42.
- [Google Scholar]
- Cavernous hemangioma of the frontal bone: A case report. J Med Case Rep. 2014;8:121.
- [Google Scholar]
- Primary cavernous haemangioma of the frontal bone: Computed tomography features. J Clin Diagn Res. 2015;9:MJ01-2.
- [Google Scholar]
- Vascular tumors. In: Mirra JM, ed. Bone Tumors; Clinical, Radiologic and Pathologic Correlations. Philadelphia: Lea – Febiger; 1989. p. :1335-478.
- [Google Scholar]






