Translate this page into:
Expanding access to microneurosurgery in low-resource settings: Feasibility of a low-cost exoscope in transforaminal lumbar interbody fusion
*Corresponding author: Ibrahim E. Efe, Department of Neurosurgery, Charité-Universitätsmedizin Berlin, Charitéplatz, Berlin, Germany. ibrahim.efe@charite.de
-
Received: ,
Accepted: ,
How to cite this article: Ramirez ME, Peralta I, Nurmukhametov R, Castillo RE, Castro JS, Volovich A, et al. Expanding access to microneurosurgery in low-resource settings: Feasibility of a low-cost exoscope in transforaminal lumbar interbody fusion. J Neurosci Rural Pract 2023;14:156-60.
Abstract
Objectives:
Less than a quarter of the world population has access to microneurosurgical care within a range of 2 h. We introduce a simplified exoscopic visualization system for low-resource settings.
Materials and Methods:
We purchased a 48 megapixels microscope camera with a c-mount lens and a ring light at a total cost of US$ 125. Sixteen patients with lumbar degenerative disk disease were divided into an exoscope group and a microscope group. In each group, we performed four open and four minimally invasive transforaminal lumbar interbody fusions (TLIF). We conducted a questionnaire-based assessment of the user experience.
Results:
The exoscope achieved similar outcomes with comparable blood loss and operating time as the microscope. It provided similar image quality and magnification. Yet, it lacked stereoscopic perception and the adjustability of the camera position was cumbersome. Most users strongly agreed the exoscope would significantly improve surgical teaching. Over 75% reported that they would recommend the exoscope to colleagues and all users saw its great potential for low-resource environments.
Conclusion:
Our low-budget exoscope is safe and feasible for TLIF and purchasable at a fraction of the cost of conventional microscopes. It may thus help expand access to neurosurgical care and training worldwide.
Keywords
Global neurosurgery
Spine surgery
Low cost
Surgical ergonomics
Exoscope
INTRODUCTION
Yasargil and Caspar were the first to perform microscope-assisted surgeries on the lumbar spine to reduce tissue damage.[1,2] The exoscope was later introduced as a hybrid visualization system capable of projecting the surgical field to a high-definition screen through a digital microscope camera. It is considered superior to the conventional binocular operating microscope with regard to enhanced surgeon’s comfort, greater magnification, and wider focal distance.[3,4] Yet, both microscopes and exoscopes are too high priced to cover the need for microneurosurgical care in low- and middle-income countries (LMICs). Less than 25% of the world population has access to a microneurosurgical facility within a range of 2 h. A main limitation is the lack of proper equipment due to high acquisition and maintenance costs.[5] We introduce a simplified low-cost exoscopic visualization system to achieve optical magnification, illumination, and video recording in low-resource settings.
Transforaminal lumbar interbody fusion (TLIF) is widely used in the treatment of lumbar herniated discs. TLIF allows access to the disk space through a laminectomy and unilateral facetectomy with minimal dural tension and better foraminal decompression.[6] Minimally invasive TLIF was later described to minimize soft-tissue trauma.[7] We, here, evaluate the low-budget exoscope’s user experience in terms of image quality, handling, and comfort compared to the conventional microscope in TLIF surgery.
MATERIALS AND METHODS
We tested the feasibility of a low-cost exoscope compared to a conventional surgical binocular microscope. The study was performed in the Department of Spine Surgery at the Hospital of the Russian Academy of Sciences. We conducted this study in compliance with the principles of the Declaration of Helsinki. To become fully acquainted with the functions and to determine the ideal settings of our exoscope, we tested its feasibility using artificial models and cadaveric specimens before our study. A total of 16 patients with single-level lumbar degenerative disease were enrolled and underwent minimally invasive or open TLIF between November and December 2021. Patients were randomly allocated to the (1) microscope-assisted minimally invasive, (2) microscope-assisted open, to the (3) exoscope-assisted minimally invasive, and (4) exoscope-assisted open groups randomly, resulting in four patients per subgroup. The surgical staff participated in a digital 15-item survey based on Likert five-point scales assessing the usability of the low-budget exoscope compared to the conventional microscope [Table 1].
| What is your role in your department? |
| Was the image quality of the low-budget exoscope superior to that of the conventional binocular microscope? |
| Was the brightness of the operative field superior when using the low-budget exoscope compared to the conventional binocular microscope? |
| Was it more convenient to perform the surgery as first operator with the low-budget exoscope compared to the conventional binocular microscope? |
| Was it more convenient to perform the surgery as assistant or scrub nurse with the low-budget exoscope compared to the conventional binocular microscope? |
| Is it easier to teach a surgery using the low-budget exoscope compared to the conventional binocular microscope? |
| Was it easier to zoom with the low-budget exoscope compared to the conventional binocular microscope? |
| Was it easier to focus with the low-budget exoscope compared to the conventional binocular microscope? |
| Was it easier to adjust the position and angle of the low-budget exoscope compared to the conventional binocular microscope? |
| Was it easier to preoperatively set up the low-budget exoscope compared to the conventional binocular microscope? |
| Did you have to ever convert from the low-budget exoscope to the conventional binocular microscope during a surgery? If yes, please explain the situation that made it necessary to switch to the conventional binocular microscope. |
| Would you recommend the low-budget exoscope to your colleagues? |
| Will you continue using the low-budget exoscope in the future? |
| Do you think the low-budget exoscope has the potential to improve neurosurgical care in low-and middle-income countries? |
| Which neurosurgical subspecialties will benefit most from the use of the low-budget exoscope? |
Patient characteristics
All patients suffered from back pain. Reduced motor strength in the lower extremities was reported by six patients in the microscope and five patients in the exoscope group. In both groups, six patients had sensory disturbances. Median time from symptom onset to surgery was 7 months in the microscope and 6 months in the exoscope group. Cardiovascular and metabolic comorbidities were present in both study arms [Table 2].
| Characteristics | Operating microscope (n=8) | Low-budget exoscope (n=8) |
|---|---|---|
| Lower back pain | 8 | 8 |
| Motor strength scale<5/5 | 6 | 5 |
| Sensory disturbances | 6 | 6 |
| Cardiovascular comorbidities | 5 | 2 |
| Diabetes mellitus | 1 | 4 |
| Smoking | 6 | 4 |
Device properties
We attached a 48 megapixels 4K 1080p industrial video microscope camera with a 1X-130X C-mount lens to a cantilever. The portable stand allowed manual positioning of the camera. A ring light composed of 56 LED bulbs provided focused shadow-free illumination with adjustable brightness. All parts were sterilized with ethylene oxide. The surgical field was projected to a 55” 2K television screen. We purchased the exoscope at a price of approximately US$ 150 [Figure 1]. Neither the microscope camera nor the television screen allowed for three-dimensional visualization. The OPMI VARIO 700 (Carl Zeiss Meditec AG) was used for the conventional microscope-assisted groups.
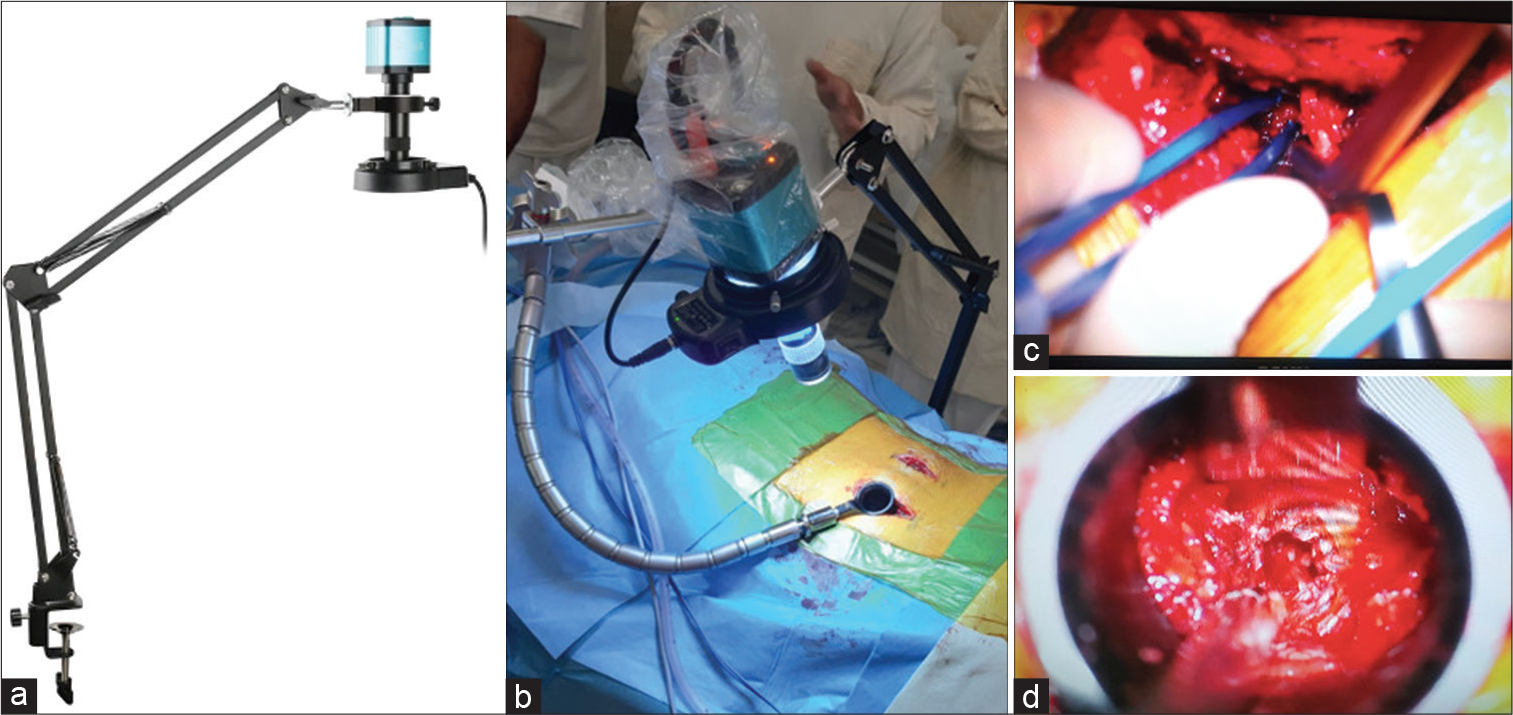
- The fully assembled low-budget exoscope (a) composed of video microscope camera, C-mount lens, LED ring light, and cantilever. Intraoperative setup (b) with camera pointing at tubular retractor in a minimally invasive transforaminal lumbar interbody fusion (TLIF) procedure. The surgical field of an open TLIF (c) and a minimally invasive TLIF (d) as projected on the television screen.
RESULTS
Surgical outcome
There were no significant differences in mean operating duration and blood loss between the low-budget exoscope and the microscope groups [Table 3]. All patients reported satisfactory lumbar and radicular pain relief. No complications were encountered. In both groups, the postoperative course was uneventful, allowing early mobilization and discharge within 3 days after surgery.
| Minimally invasive TLIF | Operating microscope | Low-budget exoscope |
|---|---|---|
| Mean patient age | 53.75±9.91 | 51±7.48 |
| Mean blood loss in ml | 225±30 | 209.5±22.23 |
| Mean operation duration in minutes | 116.5±6.61 | 128.25±6.34 |
| Open TLIF | Operating microscope | Low-budget exoscope |
| Mean patient age | 54.25±10.99 | 51.75±8.35 |
| Mean blood loss in ml | 545±157.59 | 514±97.42 |
| Mean operation duration in minutes | 97±9.02 | 101.5±7.72 |
User experience
The questionnaire was anonymously filled by five neurosurgery residents, three senior neurosurgeons, and the chief of the department. Three users reported on their experience as first operators, whereas the remaining six reported on their experience as assistant operators. The overall user experience was positive [Figure 2]. Image quality, brightness, zoom, and focus functions were non-inferior to those of the operating microscope according to most users. Surgeon’s convenience and pre-operative set-up were rated largely similar. A striking advantage of the low-budget exoscope was reported to be its use in training. More than 60% of users absolutely agreed that it was superior to the microscope in teaching surgery. Further, anecdotal reports by the senior staff included that the lack of stereoscopic perception and the cumbersome adjustability of the camera may result in a shallow learning curve. Yet, close to 80% agreed that they would recommend the device to their colleagues and 70% wanted to continue using it in the future. The users unanimously agreed that the low-cost exoscope holds great potential for LMICs.
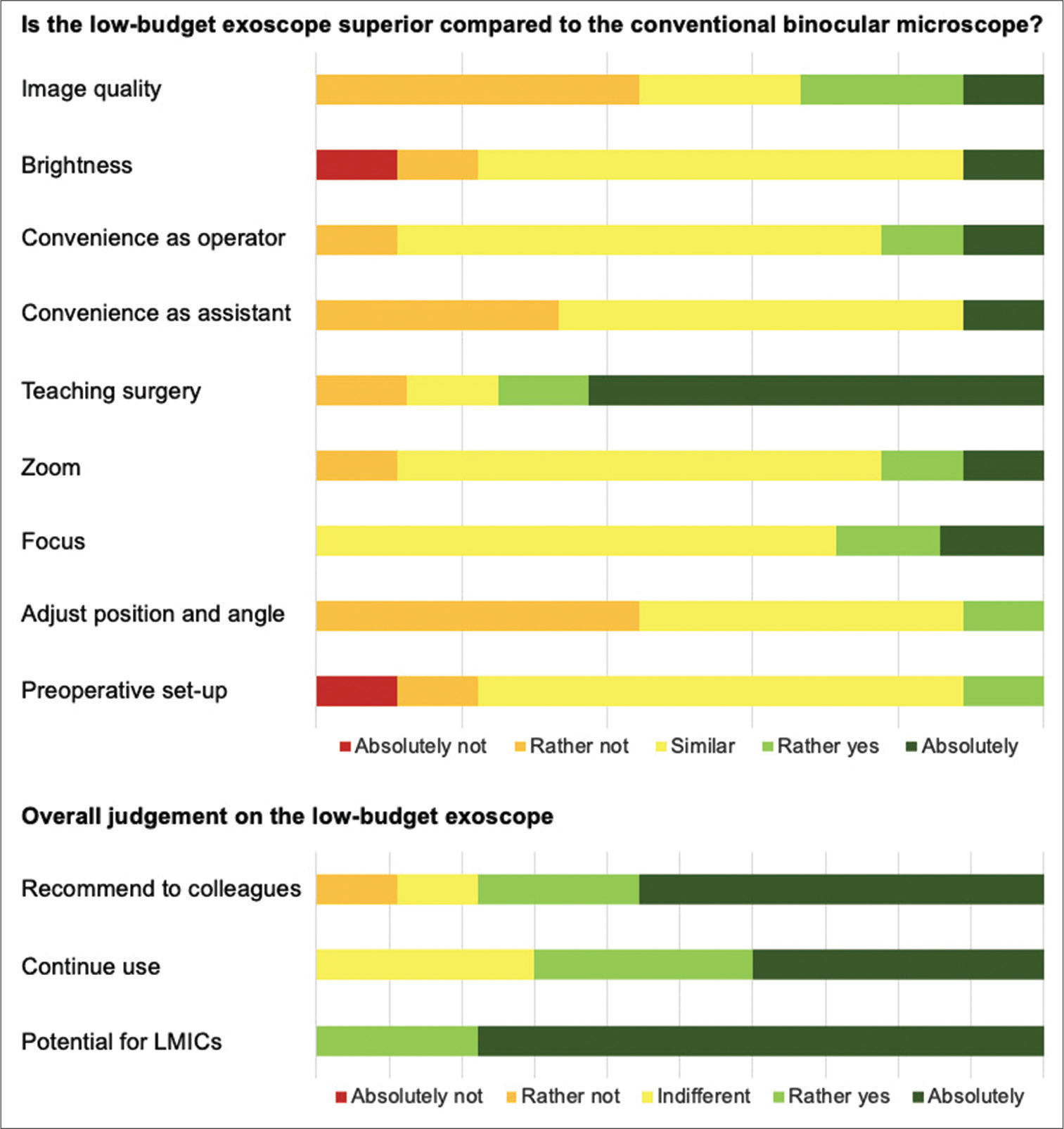
- Results of the digital questionnaire-based usability assessment.
DISCUSSION
We achieved similar outcomes with our low-cost exoscope as with the conventional operating microscope. These results were in line with the previous reports on exoscopes in neurosurgery.[8,9] The technology has gained popularity mainly due to enhanced surgeon’s comfort. The surgical field is projected to a screen allowing the surgeon to operate in a comfortable posture. The larger working distance results in more convenient instrument maneuverability and less obstruction when passing instruments in and out of the surgical field. The monitor allows the entire staff to follow the surgery from the first operator’s perspective instead of separate binocular objectives. The operator may become more aware of the rest of the operating room personnel, facilitating communication between all team members.[10,11] A recent survey showed that operating room staff felt more involved and could be of more help in exoscope-assisted surgeries than in those performed with a binocular microscope.[12] The small size of our device allowed full sterilization and easy transportation. Yet, our exoscope did not perform better than the microscope in terms of convenience. Adjusting the camera position was perceived to be cumbersome. Robotic exoscopes currently attempt to overcome this difficulty.[13] A support arm with greater freedom of motion might be a low-cost solution to achieve a more seamless workflow. According to our senior users, the lack of 3D vision was another major drawback. Our exoscope may not be suitable for deep and narrow surgical corridors, potentially limiting its use in cranial surgery. Existing exoscope systems already rely on 3D cameras to preserve image quality and depth perception while being ergonomically superior than the microscope. Novel technologies contain 4K-3D displays and fluorescent filters. The main limiting factor remains the high cost of such systems. The prices of currently available exoscopes range from $250.000 to $1.500.000.[13] While fluorescent filters help in complex microvascular and tumor surgeries, many neurosurgical operations in LMICs are still performed with no magnification due to the lack of equipment. We hope that our experiences with our $150 low-cost exoscope may encourage neurosurgeons in LMICs to seek similar solutions to provide safe microneurosurgery.
Limitations of the study
Our aim was to share our first experiences with the low-budget exoscope and to report operative data of our initial patient cohort. Hence, our sample size is small rendering statistical statements impossible. Further, we chose the TLIF procedure as it is a common spinal approach that many of our colleagues worldwide are familiar with. We cannot safely assume, however, that the low-budget exoscope would comply with the high standards of neuro-oncological or cerebrovascular operations. Thus, our results cannot be generalized to other surgical indications and careful consideration is mandatory when testing the device for other procedures or patient groups. Further, the questionnaire was filled by nine staff members of the Department of Spine Surgery at the Central Clinical Hospital of the Russian Academy of Sciences. Five were residents with limited microsurgical experience and four were senior specialists. Some could judge the feasibility from the main surgeon’s perspective, others only from that of the first assistant. Yet, all responses were pooled and quantified equally. Three of the nine survey respondents have co-authored this manuscript, rendering our survey prone to response bias. However, these three respondents joined the authors list only at the final stage of this study and were unaware that they would become coauthors at the time of exoscope use and survey participation.
CONCLUSION
Our low-budget exoscope is safe and feasible for the use in TLIF. It is of significant benefit in surgical teaching. Yet, it is purchasable at a significantly lower price than conventional microscopes. We hope that this low-cost technology can help expand access to microneurosurgical care and training worldwide.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- A new surgical procedure for lumbar disc herniation causing less tissue damage through a microsurgical approach In: Wüllenweber R, Brock M, Hamer J, Klinger M, Spoerri O, eds. Lumbar Disc Adult Hydrocephalus. Advances in Neurosurgery. Vol 4. Berlin, Heidelberg: Springer; 1977. p. :74-80.
- [CrossRef] [Google Scholar]
- Microsurgical operation of herniated lumbar disc In: Wüllenweber R, Brock M, Hamer J, Klinger M, Spoerri O, eds. Lumbar Disc Adult Hydrocephalus: Advances in Neurosurgery. Vol 4. Berlin, Heidelberg: Springer; 1977. p. :81.
- [CrossRef] [Google Scholar]
- The use of the exoscope in lateral skull base surgery: Advantages and limitations. Otol Neurotol. 2019;40:236-40.
- [CrossRef] [PubMed] [Google Scholar]
- From Exoscope into the next generation. J Korean Neurosurg Soc. 2017;60:289-93.
- [CrossRef] [PubMed] [Google Scholar]
- Neurosurgical care: Availability and access in low-income and middle-income countries. World Neurosurg. 2018;112:e240-54.
- [CrossRef] [PubMed] [Google Scholar]
- Transforaminal lumbar interbody fusion (TLIF) JBJS Essent Surg Tech. 2016;6:e22.
- [CrossRef] [PubMed] [Google Scholar]
- Minimally invasive lumbar fusion. Spine (Phila Pa 1976) 2003(28 Suppl):S26-35.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional, high-definition exoscopic anterior cervical discectomy and fusion: A valid alternative to microscope-assisted surgery. World Neurosurg. 2019;130:e244-50.
- [CrossRef] [PubMed] [Google Scholar]
- A high-definition 3D exoscope as an alternative to the operating microscope in spinal microsurgery. J Neurosurg Spine. 2020;33:705-14.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical experience with a high definition exoscope system for surgery of pineal region lesions. J Clin Neurosci. 2014;21:1245-9.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of operating microscope and exoscope in a highly challenging experimental setting. World Neurosurg. 2021;147:e468-75.
- [CrossRef] [PubMed] [Google Scholar]
- A practice survey to compare and identify the usefulness of neuroendoscope and exoscope in the current neurosurgery practice. Asian J Neurosurg. 2020;15:601.
- [CrossRef] [PubMed] [Google Scholar]
- The role of 3D exoscope systems in neurosurgery: An optical innovation. Cureus. 2021;13:e15878.
- [CrossRef] [Google Scholar]






