Translate this page into:
Endovascular trends in the treatment of intracranial aneurysms in a Peruvian reference center
*Corresponding author: Giancarlo Saal-Zapata, Department of Neurosurgery, Hospital Nacional Guillermo Almenara Irigoyen, La Victoria, Lima, Peru. gsaal1987@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Saal-Zapata G, Durand-Castro W, Valer-Gonzales D, Flores-Quijaite JE, Rodriguez-Varela R. Endovascular trends in the treatment of intracranial aneurysms in a Peruvian reference center. J Neurosci Rural Pract 2023;14:655-9.
Abstract
Objectives:
Endovascular treatment of intracranial aneurysms (IAs) has evolved in recent years and is currently the preferred treatment worldwide. We analyzed the trends in the number of patients, number of aneurysms, aneurysm characteristics, and techniques used in a pure endovascular cohort of patients treated in a reference center.
Materials and Methods:
Between 2010 and 2020, a retrospective data collection of patients who underwent endovascular intervention of IAs was performed. We used the Mann-Kendal test to evaluate the trends. In addition, the moving-average technique was used to assess smoother curves.
Results:
Eight hundred and forty-five aneurysms were treated in 765 patients, the mean age was 53.9 ± 14.6 years and 81% were women. The number of patients (P = 0.016) and aneurysms (P = 0.003) increased significantly. Unruptured (P = 0.029) and posterior communicating artery aneurysms increased their frequency of treatment (P = 0.042). Balloon remodeling (P = 0.01) and the use of flow diverters showed a positive trend (P = 0.016).
Conclusion:
There have been an increased number of patients and aneurysms treated endovascularly at our institution, including unruptured and posterior communicating aneurysms. Advanced endovascular techniques also increased. Comparative studies including surgical cases must be done in our region to determine the best approach.
Keywords
Intracranial aneurysm
Subarachnoid hemorrhage
Endovascular treatment
Coiling
Balloon-assisted coiling
INTRODUCTION
Endovascular treatment (EVT) of intracranial aneurysms (IAs) marked a major change in the neurosurgical practice. Since the introduction of Guglielmi Detachable Coils (GDC), this technique has experienced an increase in several centers worldwide.[1] Primary coiling, advanced assisted-coiling techniques with balloons and stents, flow diverters, and intrasaccular devices have emerged as new alternatives in the treatment of this pathology.[2,3] In addition, new devices, approaches and techniques have improved over time, and nowadays, EVT is performed worldwide.[4,5]
Few centers have reported their trends over time regarding the EVT of IAs. As mentioned in the previous studies, clipping is nowadays less common and EVT is increasing.[2-7] According to a recent publication, IA treatment will continue to shift toward EVT with the development of new materials, including intrasaccular devices and new flow diverters.[3]
Hence, the objective of our study was to assess the trends in the number of aneurysms, angiographic characteristics and endovascular techniques employed during a decade in a reference endovascular institution.
MATERIALS AND METHODS
Patient selection and variables
Between January 2010 and December 2020, data collection from medical charts, angiographic studies, and brain tomographic scans of 765 patients who were candidates for EVT was performed at our institution. Age, sex, number of patients, and number of aneurysms were collected. Aneurysms’ characteristics included rupture status, location, size (large and width) and neck diameter. Endovascular techniques employed included primary coiling, balloon-assisted coiling (BAC), stent-assisted coiling (SAC), primary stenting, the combination of coiling + balloon + stenting, and flow diversion. An additional analysis including complications (intraoperative rupture), occlusion rates determined by the Raymond-Roy (RR) classification, and clinical outcomes determined by the modified Rankin Scale (mRS) was also performed.
Procedure details
All the patients were treated under general anesthesia. From January 2010 to December 2016, the procedures were performed in a C-arm Philips BV Pulsera (Philips, Philips Medical Systems, The Netherlands). From January 2017 and beyond, all the procedures were performed in the biplane angiography Philips Allura Xper FD20/10 (Philips). Continuous irrigation through saline solutions with 1500 UI of heparin was maintained during the entire procedure. The femoral or radial artery was approached according to the surgeon’s preference. A 6F guide catheter mas commonly used. For Penumbra coils 400 (PC400), an 8F guide catheter was used. For primary coiling, a 0.017-inch (Headway 17, Microvention ; VASCO+10, Balt) or 0.025-inch microcatheter (PX Slim; Penumbra) were navigated over a 0.014 microguidewire (Traxcess 14; Microvention) under road mapping into the aneurysm sac. Depending on the aneurysm shape, location and status of rupture, primary coiling, BAC, SAC, or flow diverter placement were chosen as the main techniques. For BAC, the Scepter (Microvention), Eclipse (Balt) or Hyperform (Microvention) balloons were used. The balloons were navigated over a 0.014-inch microguidewire in all cases. For SAC, LVIS/LVIS Jr (Microvention), LEO/LEO baby (Balt), and Neuroform (Stryker) stents were employed. Depending on the type of stent, a 0.017-inch, 0.021-inch, or 0.027-inch microcatheters were used. For flow diverters, a 0.027-inch microcatheter was used to deliver the device in the parent artery. Manual compression of the femoral or radial artery was performed at the end of the procedure.
Statistical analysis
Categorical variables were shown as percentages and numerical variables as means and standard deviation. The Mann-Kendal test was used to assess time trends in the number of patients, number of aneurysms treated per year, mean age, rupture status, aneurysm characteristics, location, and the endovascular technique employed. We used the moving average (MA) technique, using the current observation, one lagged observation, and one forward observation with the aim of creating smoother curves. Stata v14.0 (StataCorp, College Station, TX, USA) was used for the statistical analysis.
RESULTS
Trends according to number of patients, number of aneurysms, and age
Seven hundred and sixty-five patients underwent 845 endovascular embolizations of IAs. The overall mean age was 53.9 ± 14.6 years and 81% were women. The mean age of men and women was 52.2 and 54.3 years, respectively. A significant growing trend in the number of patients during time was evidenced (P = 0.016; p for MA [pMA] = 0.005), especially in 2019 in which more aneurysms were treated. When the number of aneurysms was analyzed, a significant growing trend during time was seen (P = 0.003; pMA = 0.003). When the mean age of the patients was evaluated, we did not identify significant variations (P = 0.39; pMA = 0.138) [Figure 1].
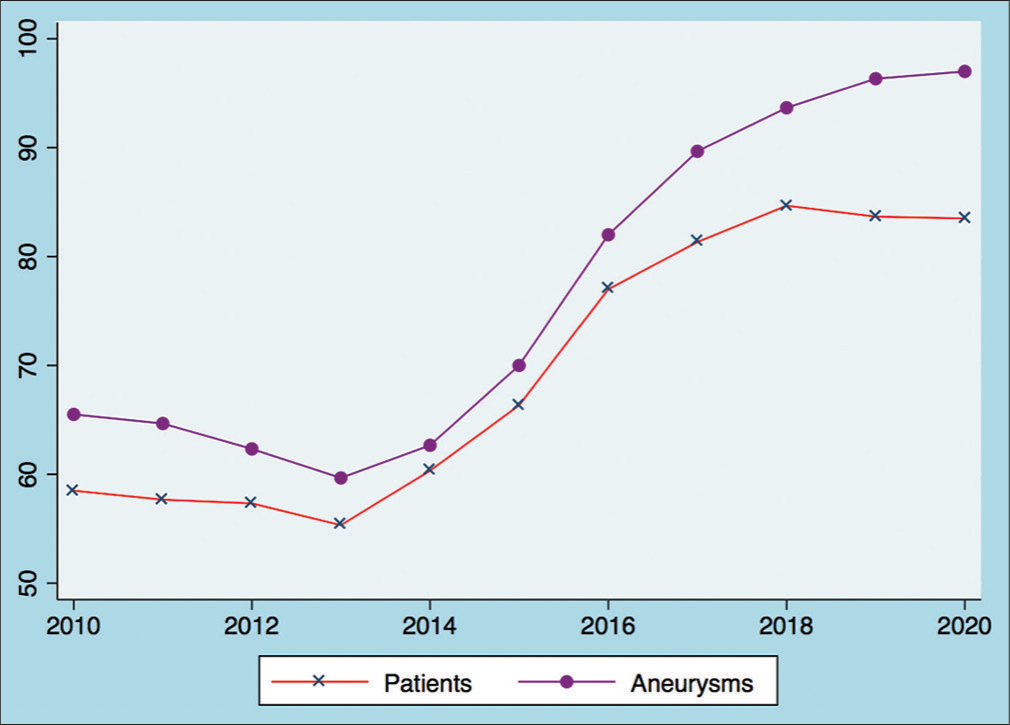
- Trends of the number of patients and aneurysms treated, which shows an increased number of cases.
Trends according to aneurysm characteristics: Rupture status, location, and dimensions
We analyzed trends according to the aneurysm status (rupture vs. unruptured) during time. No variations were seen in the case of ruptured aneurysms (P = 0.117; pMA = 0.1), whereas we found a significant growing trend in the treatment of unruptured cases (P = 0.029; pMA = 0.001), especially since the year 2015 to the present [Figure 2]. We grouped the aneurysm location in seven groups. Posterior communicating artery aneurysms increased their treatment (P = 0.042: pMA = 0.002), paraclinoid aneurysms did not show variations (P = 0.06; pMA = 0.019), as well as anterior communicating aneurysms (P = 0.235; pMA = 0.21). For middle cerebral artery (P = 0.431; pMA = 0.347), internal carotid artery (ICA) (P = 1; pMA = 0.754), and posterior fossa aneurysms (P = 0.813; pMA = 0.028), there were no differences [Figure 3]. We evaluated the dimension of aneurysms: We did not find variations in large (P = 0.31; pMA = 0.213), width (P = 0.35; pMA = 0.876) or neck diameter (P = 1; pMA = 0.815) during time [Figure 4].
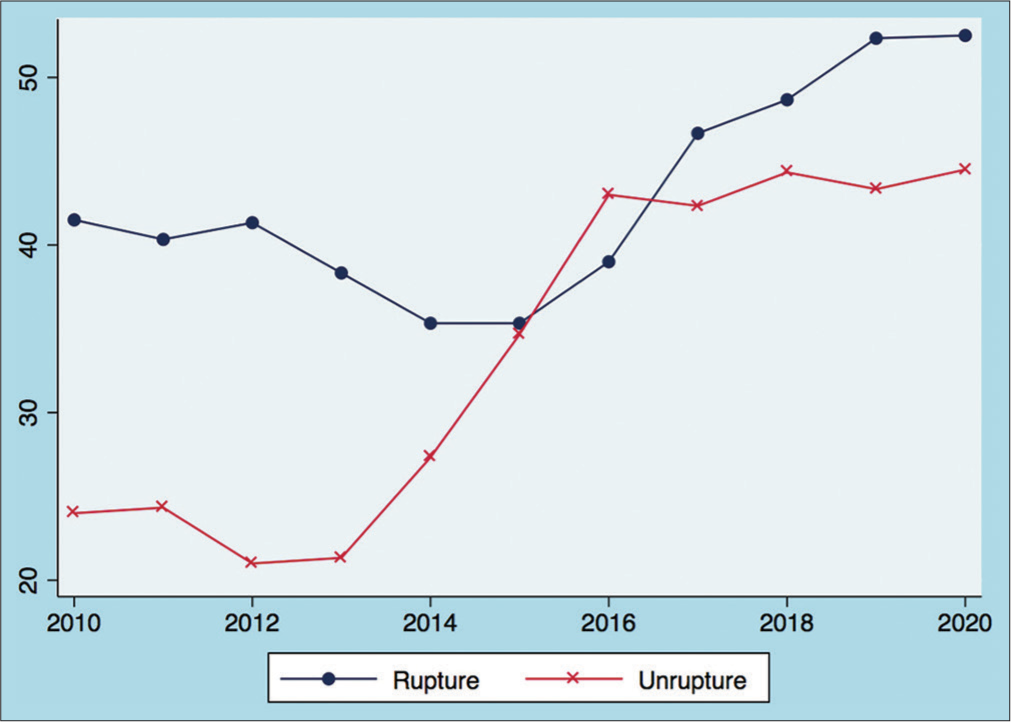
- Trends in cases of ruptured and unruptured aneurysms, with a positive trend in the number of unruptured cases treated endovascularly.

- Location of the aneurysms treated, with a positive trend in the number of posterior communicating cases.
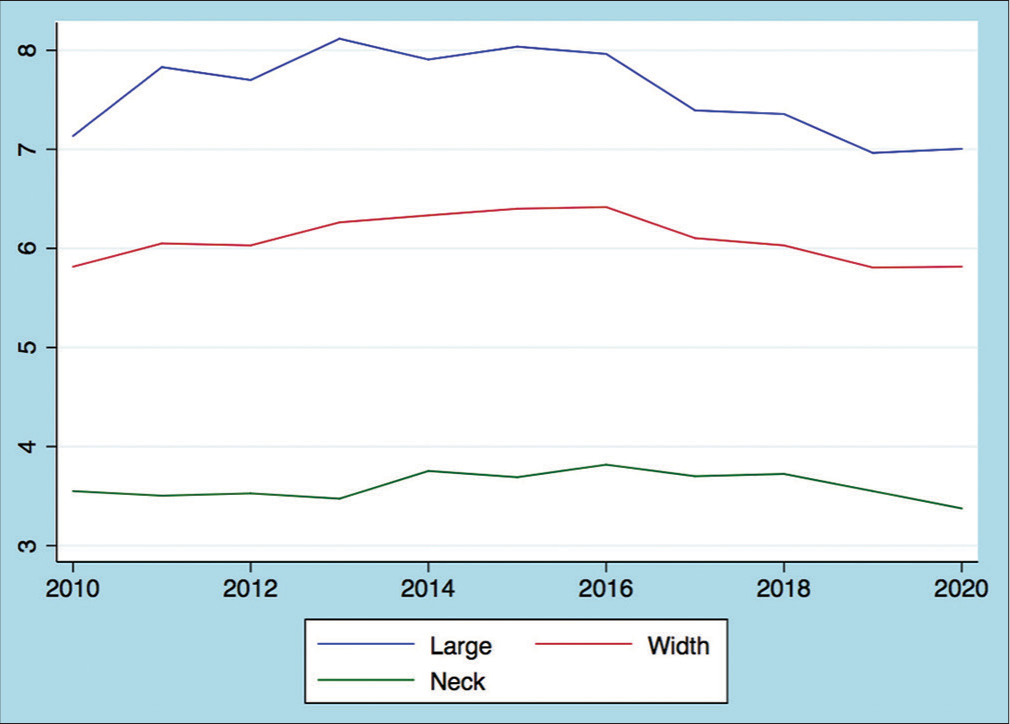
- Dimensions of the aneurysms treated.
Trends according to the endovascular technique employed
Primary coiling did not show variations in time (P = 0.75; pMA = 0.184). A significant growing trend was seen for BAC (P = 0.01; pMA = 0.003), but not for SAC (P = 0.531; pMA= 0.014). Flow diverters showed a positive trend (P = 0.016; pMA <0.001). The trend became negative when only stents were used (P = 0.021; pMA = 0.003). Finally, coiling + balloon + stent, which were more frequently used in the last 3 years, showed a growing tendency (P = 0.016; pMA = 0.003) [Figure 5].

- Endovascular techniques employed.
Complications, occlusion rates, and follow-up
During the study period, 44 patients (5.65%) developed intraoperative rupture during the embolization, with the highest rate in the year 2020 with 10 cases (11.1%). According to the RR classification, immediate complete occlusion was 47.5%, neck remnant 17.1%, RR3A in 32.8%, and RR3B in 0.8% of the patients. The mean angiographic follow-up was performed in 49.6% of the patients during the study period. A good clinical outcome determined by a mRS <3 was achieved in 90.5% of patients during the study period.
DISCUSSION
Our study aimed to determine the trends in the EVT of IAs in a Peruvian tertiary endovascular institution. We identified an increasing trend in the treatment of patients and aneurysms during the last decade when EVT was employed, with a significant positive trend in the treatment of unruptured and posterior communicating artery aneurysms. Similar results were published recently.[8] We also found that the treatment with BAC, flow diverters, and coiling + balloons + stents have maintained a significant growing trend during the last decade as well. Finally, a negative trend was identified with the use of primary stenting. Overall, the use of advanced techniques for embolization of unruptured aneurysms has increased over the period analyzed, which explains the development of new endovascular devices and their availability in our endovascular center.
Surgical treatment of IAs has been the gold standard treatment before the development of endovascular therapy.[6] Since the introduction of GDC in the early 90s, a decrease in clipping was evidenced in several centers worldwide,[9] specially when two landmark studies demonstrated better clinical outcomes and good occlusion rates when EVT was used.[10-12] Indeed, our center shifted to EVT considering the results of the previously mentioned trials. Nevertheless, clipping remains as the main treatment modality according to its long-term occlusion rates and lower associated costs.[13] The emergence of coils, balloons, and stents favored EVT to include a wide range of aneurysms’ sizes and morphologies, and not only selected cases of small or medium sized, or short-neck aneurysms.[2] In our institution, EVT has become the first-line treatment for IAs regardless of the location, status of rupture, or morphology.
We found that EVT of unruptured IAs increased, which is the trend found in previous publications.[4,7,8,14] In this scenario, better clinical outcomes and a shorter length of in-hospital stay are the main advantages of this treatment modality.[7,15,16] However, long-term durability of the embolization remains unclear,[14] specially when only primary coiling is employed as the main technique.[17] An increased use of diagnostic imaging revealing unruptured aneurysms as incidental findings may explain our results. We did not find an increase in the EVT of ruptured aneurysms, similar to the findings of previous publications.[4,6,14,18,19] This determined that our institution receives a constant number of ruptured cases during this period, and this finding may be used as a public health indicator for possible screening and post-operative rehabilitation. According to the location, we determined that the most frequent aneurysm was found in the posterior communicating artery segment of the ICA, which in turn is the most frequent aneurysm in our population. On the other hand, paraclinoid aneurysms showed a positive trend since 2014; however, this was not statistically significant. Other locations and aneurysm dimensions did not show any variability during the study period.
Primary coiling was the main treatment modality in the early development of EVT with precise indications.[1,20] Wide-neck and dysplastic aneurysms were not the main indications for treatment initially, but with an increased experience in the technique, a wider spectrum of cases could be treated.[21] We observed that primary coiling tend to decrease specially since 2018, but this was not statistically significant. However, this determined the shift in the use of adjunctive techniques to improve aneurysm obliteration and reduce recurrence rates. Nevertheless, we observed that the use of BAC and flow diverters increased, due to the growing tendency to treat wide-neck, dysplastic, and complex aneurysms to produce a complete sac occlusion.[3] A negative trend to use primary stenting explains the increasing use of flow diverters which have higher occlusion rates at follow-up.[22]
Given the complexity of endovascular procedures, continuous training is mandatory in order to update knowledge in the field. With this purpose, health-care professional meet several courses and conferences worldwide either online or in-person. On the other hand, the institution has the Training Program that allows health-care professionals to train in their respective specialties. However, many times self-funded training is required to attend meetings. Indeed, the hospital is a Social Security institution supported by a monthly stipend from formal employees around the country. Therefore, there is a large economic funding supporting high-cost endovascular procedure.
The study has several limitations: due to the retrospective design, there is an inherent limitation. The lack of a comparison group, specifically clipping cases, is maybe the most important limitation in order to compare the trends of these techniques in a single-center scenario. Nevertheless, the aim of the study focusses specifically in the EVT of IAs. Other important variables such as complication rates, length of stay, clinical, and angiographic follow-up are lacking because of the incomplete data in the 1 years of the decade. Our database was obtained mostly from clinical records and angiographic reports, so accuracy of the data should be taken with caution. Finally, our institution is a reference endovascular center which receives complex cases from all over the country, so the population shown here is unique, and a selection bias must be considered.
CONCLUSION
EVT of IAs is the first-line treatment in our institution. As evidenced in our study, there is an increase in the number of unruptured aneurysms, located in the posterior communicating segment and treated with balloon-assisted techniques. These trends are in accordance with current data, where EVT is increasing in several centers worldwide. Further studies with long-term clinical and radiological follow-up are required to determine the benefits of this minimally invasive technique and compare these results with open surgery cases.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Surgical versus endovascular management of ruptured and unruptured intracranial aneurysms: Emergent issues and future directions. World Neurosurg. 2020;136:17-27.
- [CrossRef] [PubMed] [Google Scholar]
- Recent trends in the treatment of cerebral aneurysms: Analysis of a nationwide inpatient database. J Neurosurg. 2008;108:1163-9.
- [CrossRef] [PubMed] [Google Scholar]
- Flow-diverter devices for intracranial aneurysms: Systematic review and meta-analysis. Neurosurgery. 2013;73:193-200.
- [CrossRef] [PubMed] [Google Scholar]
- Shifting treatment paradigms for ruptured aneurysms from open surgery to endovascular therapy over 25 years. World Neurosurg. 2017;106:919-24.
- [CrossRef] [PubMed] [Google Scholar]
- Coiling vs. clipping: Hospital stay and procedure time in intracranial aneurysm treatment. Rofo. 2009;181:989-95.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of large and giant fusiform intracranial aneurysms with Guglielmi detachable coils. J Neurosurg. 1996;84:55-62.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular versus surgical treatment in subarachnoid haemorrhage: Cost analysis. Neurocirugia (Astur). 2015;26:13-22.
- [CrossRef] [PubMed] [Google Scholar]
- Natural course of unoperated intracranial arteriovenous malformations: Study of 50 cases. J Neurosurg. 1989;71:805-9.
- [CrossRef] [PubMed] [Google Scholar]
- The future of open vascular neurosurgery: Perspectives on cavernous malformations, AVMs, and bypasses for complex aneurysms. J Neurosurg. 2019;130:1409-25.
- [CrossRef] [PubMed] [Google Scholar]
- Intraoperative digital subtraction angiography and the surgical treatment of intracranial aneurysms and vascular malformations. J Neurosurg. 1990;73:526-33.
- [CrossRef] [PubMed] [Google Scholar]
- Angiographic outcome of intracranial aneurysms with neck remnant following coil embolization. J Neurointerv Surg. 2015;7:484-9.
- [CrossRef] [PubMed] [Google Scholar]
- Recent trends in neuro-endovascular treatment for acute ischemic stroke, cerebral aneurysms, carotid stenosis, and brain arteriovenous malformations. Neurol Med Chir (Tokyo). 2017;57:253-60.
- [CrossRef] [PubMed] [Google Scholar]
- International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005;366:809-17.
- [CrossRef] [PubMed] [Google Scholar]
- National trends in the treatment of ruptured cerebral aneurysms in Korea using an age-adjusted method. J Korean Med Sci. 2020;35:e323.
- [CrossRef] [PubMed] [Google Scholar]
- Recent trends in electively treated unruptured intracranial aneurysms. J Stroke Cerebrovasc Dis. 2019;28:2011-7.
- [CrossRef] [PubMed] [Google Scholar]
- Geographic variation and regional trends in adoption of endovascular techniques for cerebral aneurysms. J Neurosurg. 2011;114:1768-77.
- [CrossRef] [PubMed] [Google Scholar]
- The barrow ruptured aneurysm trial: 6-year results. J Neurosurg. 2015;123:609-17.
- [CrossRef] [PubMed] [Google Scholar]
- Four-year trends in the treatment of cerebral aneurysms in Poland in 2009-2012. Acta Neurochir (Wien). 2014;156:861-8.
- [CrossRef] [PubMed] [Google Scholar]
- Unruptured intracranial aneurysms--risk of rupture and risks of surgical intervention. N Engl J Med. 1998;339:1725-33.
- [CrossRef] [PubMed] [Google Scholar]
- Guglielmi detachable coil embolization of intracranial aneurysms. J Stroke Cerebrovasc Dis. 1997;6:249-52.
- [CrossRef] [PubMed] [Google Scholar]
- Cerebral aneurysm treatment trends in National Inpatient Sample 2007-2016: Endovascular therapies favored over surgery. J Neurointerv Surg. 2020;12:957-63.
- [CrossRef] [PubMed] [Google Scholar]
- Unruptured intracranial aneurysms: Natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003;362:103-10.
- [CrossRef] [PubMed] [Google Scholar]






