Translate this page into:
Dural Ectasia of the Optic Nerve: A Rare Presentation in Neurofibromatosis Type I
Address for correspondence: Dr. Minhaj Shaikh, Department of Radiology, AIIMS, Jodhpur, Rajasthan, India. E-mail: minhaj0443@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Neurofibromatosis Type 1 (NF-1) is a common neurocutaneous syndrome with a characteristic spectrum of pathologies affecting the optic pathway. Optic pathway glioma and optic nerve meningioma are two such common afflictions of the optic nerve in NF-1. Dural ectasia of the optic nerve also known as optic nerve meningocele is a rare manifestation of optic nerve involvement in NF-1. Magnetic resonance imaging (MRI) is an excellent modality to accurately identify, characterize, delineate, and differentiate dural ectasia of the optic nerve from the commoner lesions such as optic glioma and meningioma in NF-1. We describe a case of a young woman with NF and a large recurrent palpebral neurofibroma. MRI evaluation of the orbits revealed extensive ectasia of the dura lining the cerebrospinal fluid sheath around all the segments of the optic nerve and around the optic chiasm.
Keywords
Dural ectasia
glioma
meningioma
neurofibromatosis
optic nerve
INTRODUCTION
Neurofibromatosis type I (NF-1) is a complex multisystem genetic disorder with a wide spectrum of cutaneous and neurologic manifestations. Optic nerve involvement in NF-1 is characterized by benign lesions such as optic nerve glioma and meningioma. However, a rare presentation of optic nerve involvement in NF-1 is ectasia of the dura lining the cerebrospinal fluid (CSF) sheath around the optic nerve. Clinicians and radiologists are familiar with the spinal dural ectasias and meningoceles in NF; however, dural ectasia of the optic nerve is not often mentioned in literature owing to its rarity. Also known as optic nerve sheath meningocele, this lesion merits differentiation from the common optic nerve pathologies in NF-1 such as glioma and meningioma. Magnetic resonance imaging (MRI) is an excellent tool to accurately detect, delineate, and differentiate dural ectasia of the optic nerve from other common optic nerve pathologies in NF-1. This case report familiarizes the clinicians and radiologist with this rare affliction of the optic pathway in NF and emphasizes the role of MRI in accurate diagnosis and differentiation from the commoner pathologies of optic nerve glioma and meningioma.
CASE REPORT
A 20-year-old female presented with a recurrent large sagging soft-tissue swelling arising from the right upper eyelid and draping over the right side of her face. She was operated 7 years back for the same soft-tissue mass which was histopathologically diagnosed as neurofibroma. The recurrent neurofibroma was covering her right eye completely, and the palpebral aperture was seen only when the mass was manually lifted up. Contrast-enhanced multiplanar and multisequence MRI of the brain and the orbits was done on a GE Discovery MR750w 3.0T scanner for further evaluation. MRI revealed a large neurofibroma arising from the right upper eyelid with infiltration into intraorbital fat. The globe was dysmorphic and proptosed with T2-hypointense hemorrhagic contents. There was tubulocystic dilation of the CSF sheath along the intraconal, intracanalicular, and intracranial segments of the right optic nerve as well as along the optic chiasm [Figures 1 and 2]. Thin hypointense optic nerve was seen coursing through it. On contrast-enhanced images, smooth enhancement of the dura lining the CSF sheath was seen; however, no internal nodular or solid areas of enhancement were noted [Figure 3].
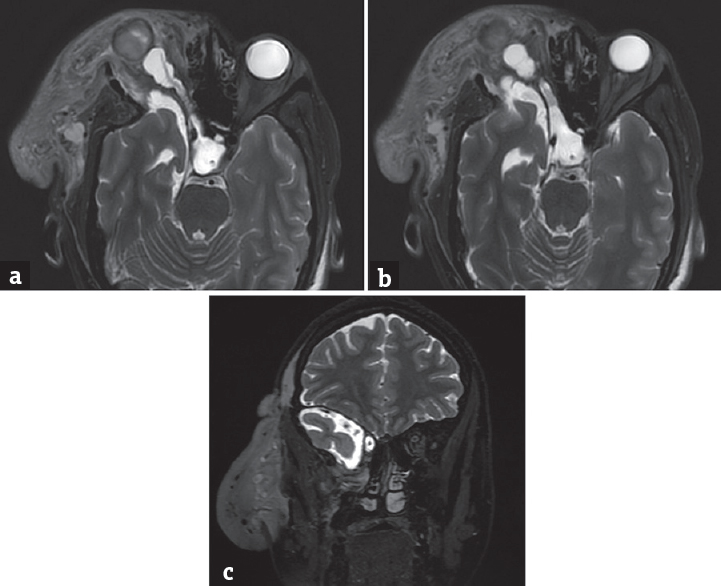
- Dural ectasia of optic nerve. (a) Axial T2WI shows a large sagging mass (neurofibroma) arising from the right palpebral soft tissues and infiltrating into the orbit (block white arrow). The tubulocystic dilation of the CSF sheath around a thin right optic nerve can be seen extending all the way upto the optic chiasm (thin white arrow). The deformed, proptosed right globe with hemorrhagic contents can also be seen (block black arrow). (b) Axial T2WI at a slightly caudal level shows tubular dilation of the CSF sheath around the intracranial portion of the right optic nerve and the optic chiasm. The enlarged right middle cranial fossa (due to dysplastic sphenoid bone) with herniating anterior temporal pole and widened CSF spaces can be seen (black arrow). (c) Coronal T2WI shows the dilated CSF sheath around the intracranial segment of right optic nerve (thin white arrow), widened CSF spaces of the dysplastic and enlarged right middle cranial fossa (black arrow), and sagging right palpebral neurofibroma (block white arrow)
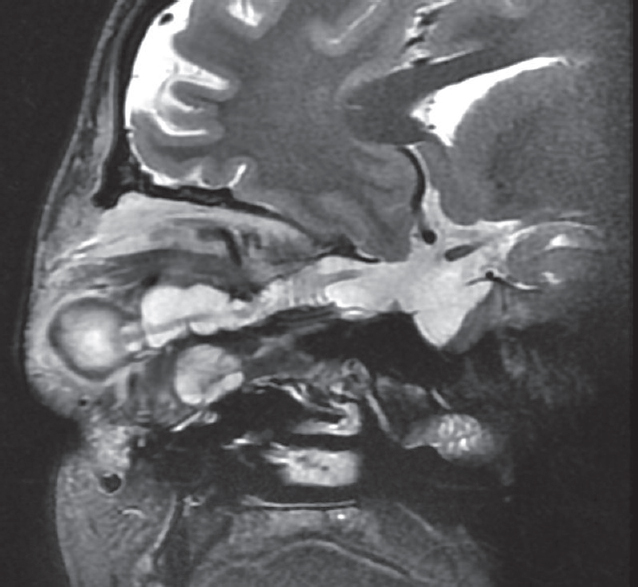
- Complete extent of dural ectasia. Sagittal T2WI shows the entire extent of dural ectasia from the optic nerve head to optic chiasm. Note the thin T2 hypointense optic nerve coursing through it
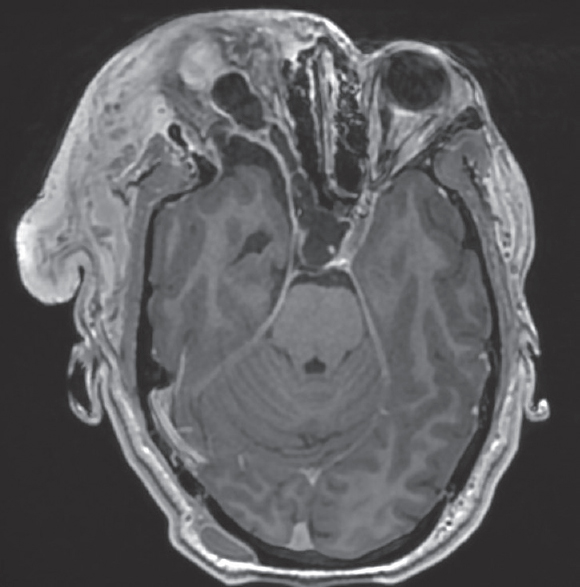
- Contrastenhanced MRI. Contrast enhanced axial T1WI show the dilated perioptic CSF sheath with smooth and sharp enhancement of the dura outlining it. No internal areas of enhancement are seen within it. Note the heterogeneous enhancement of the palpebral neurofibroma
DISCUSSION
The earliest description of dural ectasia of the optic nerve sheath was by Bane in 1918 who described it as a cyst of dural sheath of the optic nerve.[1] The most extensive series of patients with dilated optic nerve sheaths and enlarged CSF spaces was studied by Garrity et al. who described their clinical and radiological (computed tomography [CT] and MRI) features and were the first to use the term “optic nerve sheath meningoceles.”[2] They defined it as dilation of optic nerve sheath and expansion of CSF around the optic nerve and recommended MRI as the imaging modality of choice. Of the 13 patients with optic nerve sheath meningoceles, three had NF-1. Addressing this particular association, Lovblad et al. in 1994 studied the CT and MRI characteristics of three patients with NF-1 and dural ectasia of the optic nerve sheath.[3] They found the dural ectasias of the optic nerve as nonprogressive, nonenhancing, CSF density enlargements of the optic nerve which cannot be reliably distinguished from the more common optic pathway lesion in NF1, the optic glioma. MRI showed dural ectasias as dilated perioptic dural sheaths; however, the authors cautiously advised to include optic gliomas in the differential diagnoses as they encountered reports of similar appearing lesions on MRI turning out to be perioptic gliosis/gliomatosis due to optic gliomas on pathologic examination.[3] This was further illustrated in recent literature when the peripheral T2 hyperintensity (mimicking dilated CSF/subarachnoid space) in optic nerve gliomas was found to be leptomeningeal infiltration of the tumor on pathologic examination.[45]
The most common brain tumor in NF-1 is optic pathway gliomas.[6] Optic pathway gliomas affect about 20% of children with NF-1 and are isointense to hyperintense on T2-weighted images show variable enhancement and no separate visualization of the optic nerve from the tumor.[46] Other case reports of optic nerve meningoceles (associated with or without NF-1) describe it as tubular or saccular enlargement of optic nerve sheath filled with CSF and harboring a separately visualized normal or thickened optic nerve (imparting a characteristic bull's-eye appearance on coronal T2-weighted images) similar to our case.[78] Thus, a nonenhancing and separately visualized optic nerve of uniform thickness surrounded by an enlarged CSF filled optic nerve sheath should serve to confidently diagnose optic nerve meningocele. Surgical decompression of the optic nerve has been successfully reported to prevent progression of vision loss in patients with acute presentation.[910]
CONCLUSION
NF-1 is associated with a myriad of orbital pathologies, one of which is dural ectasia of the optic nerve or optic nerve meningoceles. Familiarity with its classic imaging and clinical features described in this case report can help its early detection and differentiation from a more sinister manifestation of NF-1, the optic glioma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initial will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Optic nerve sheath meningoceles. Clinical and radiographic features in 13 cases with a review of the literature. Ophthalmology. 1990;97:1519-31.
- [Google Scholar]
- Dural ectasia of the optic nerve sheath in neurofibromatosis type 1: CT and MR features. J Comput Assist Tomogr. 1994;18:728-30.
- [Google Scholar]
- Orbital neoplasms in adults: Clinical, radiologic, and pathologic review. Radiographics. 2013;33:1739-58.
- [Google Scholar]
- MR imaging of neoplastic and non-neoplastic lesions of the brain and spine in neurofibromatosis type I. Neurol Sci. 2018;39:821-7.
- [Google Scholar]
- Dural ectasia of the optic nerve sheath: Is it always benign? Eye Brain. 2009;1:5-7.
- [Google Scholar]
- Bilateral idopathic optic nerve sheath meningocele associated with unilateral transient cystoid macular oedema. Eye (Lond). 2002;16:800-2.
- [Google Scholar]
- Surgically verified case of optic sheath nerve meningocele: Case report with review of the literature. Neurosurg Rev. 1997;20:201-5.
- [Google Scholar]






