Translate this page into:
Dolichoectasia of vertebrobasilar arteries as a cause of hydrocephalus
Address for correspondence: Dr. Ritesh Kansal, Department of Neurosurgery, King Edward Memorial Hospital, Seth GS Medical College, Parel, Mumbai - 400 012, India. E-mail: drkansal@yahoo.co.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Dolichoectasia of vertebrobasilar artery is a condition in which the vertebral/basilar artery is elongated, distended and tortuous. It is usually asymptomatic. It may present with compressive or ischemic symptoms. Hydrocephalus as a complication of vertebrobasilar dolichoectasia is rare. We present a case of a 60-year-old male with dolichoectasia of the basilar artery causing compression of the third ventricular outflow and, thus, presenting with noncommunicating hydrocephalus.
Keywords
Dolicoectasia
hydrocephalus
vertebrobasilar artery
Introduction
Vertebrobasilar dolichoectasia (VBD) is a condition characterized by ectasia, elongation and tortuosity of the basilar artery. It may manifest clinically by compression of the cranial nerves, ischemic symptoms or intracranial bleeding. Rarely, the dilated and ecstatic basilar trunk may manifest as obstructive hydrocephalus. We present a 60-year-old male with markedly dilated and elongated basilar trunk compressing the third ventricular outflow and, thus, presenting with hydrocephalus.
Case Report
A 60-year-old male presented to our outpatient department with complaints of headache since 2 years. He also complained of imbalance while walking and episodes of urinary incontinence since the past 5 months. On examination, he had bilateral papilloedema. He underwent further evaluation with magnetic resonance imaging (MRI) of the brain, computerized tomography (CT) of the brain and CT angiography. MRI brain revealed dilated supratentorial ventricles with periventricular ooze. Dilated and tortuous basilar artery was noted extending into the suprasellar space compressing the third ventricular outflow. CT angiography of the brain showed dilated and tortuous left vertebral artery curving in the premesencephalic cistern from left to right and again from right to left. The basilar artery was also tortuous, with a diameter of 7.0 mm and extending into the suprasellar cistern [Figure 1]. The patient underwent right-sided ventriculoperitoneal shunt and the headache improved postoperatively.
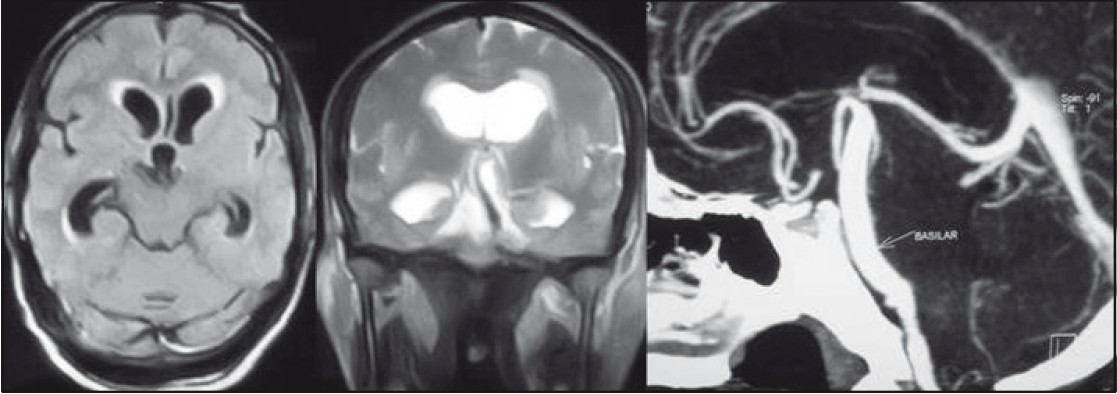
- Left and middle pictures show dilated ventricles with dolichoectatic basilar artery compressing the midbrain and outflow of the third ventricle. The right picture shows the computerized tomography angiogram with the dilated and elongated basilar trunk extending into the suprasellar space
Discussion
VBD is an anatomic variant that consists of enlargement and dilatation, often associated with a tortuous and elongated vessel.[1] It is known by various names like dolichoectasia, megadolichoectasia fusiform aneurysm of the vertebral and basilar arteries and tortuous vertebrobasilar system.[2] The prevalence of VBD is 4.4%, and it is more commonly observed in women. The major location for VBD is the basilar artery alone (40%), followed by bilateral vertebral arteries, basilar artery (22%) and both vertebral arteries (16%).[1]
The diagnostic criteria for VBD is a basilar artery or vertebral artery diameter >4.5 mm or deviation of any portion of them higher than 10 mm from the shortest expected course, or basilar length >29.5 mm or intracranial vertebral artery length >23.5 mm.[1]
The vertebrobasilar system may be considered elongated if the basilar artery lies lateral to the margin of the clivus or dorsum sellae, or if it bifurcates above the plane of the suprasellar cistern.[2]
The etiology of VBD is not clear. Hypertension, commonly associated with VBD, may cause continued stress on the walls of the artery and degrade the vessel wall by damaging and loosening the collagen and elastin meshwork that comprises the intima.[3]
Traditionally, VBD has been regarded as atherosclerotic in nature, much like aneurysms of the peripheral vascular system. However, recently, Mizutani and Aruga[4] suggested that some cases represent a dissecting process. It may also be a congenital vasculopathy of the elastic layer of the arterial wall.[156]
VBD is characterized by a high degree of variability in clinical outcome. It is usually asymptomatic and less than 10% of the patients have neurologic symptoms.[7]
It may present with varied clinical syndromes like cerebellar dysfunction, ischemic stroke, transient or permanent motor deficits, central sleep apnea, trigeminal neuralgia, hydrocephalus as well as brain stem compression syndrome.[158] Symptoms may range from mild to severe. Clinical expression of this condition may be due to compression of the cranial nerves or brainstem, ischemia in the vertebrobasilar arterial territory and intracranial bleeding.
The hydrocephalus is an uncommon complication of VBD. Ikeda et al. studied 7345 adult subjects, and found that 96 of them had asymptomatic VBD. Among these 96 subjects, only four subjects had hydrocephalus as the neuroradiological finding.[9] Hydrocephalus in VBD can be due to compression of the third ventricle by the ectatic, elongated and tortuous basilar artery. Only few cases of hydrocephalus due to direct compression of the aqueduct, foramen of Monro or third ventricle have been reported in the literature.[10–14] Most of these cases have been reported in elderly patients. A peculiar mechanism of hydrocephalus by “water-hammering” effect due to the pulsating blood in the ectatic vessel, which creates cerebrospinal fluid outflow impairment through the third ventricle, has also been described.[15]
Management of VBD depends on symptomatic manifestations. For asymptomatic patients with VBD, functional testing such as brainstem auditory-evoked potentials (BAEPs), blink reflex (BR) and motor-evoked potentials may be useful for long-term monitoring and may help in the decision-making process prior to the surgical approach for relief of subjective symptoms.[6] Our patient presented with typical features of obstructive hydrocephalus. Ventriculoperitoneal shunt provided prompt relief in symptoms of the patient. These cases are most commonly managed with ventriculoperitoneal shunt. Cases having obstruction of foramen of Monro may benefit with biventricular shunt.[46] Endoscopic third ventriculostomy may be technically difficult in these cases due to the odd anatomy of the basilar trunk.
Conclusion
VBD as a rare cause of obstructive hydrocephalus needs to be kept in mind by neurosurgeons.
The authors acknowledge with gratitude the encouragement and support of Dr. Atul Goel.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Vertebrobasilar dolichoectasia diagnosed by magnetic resonance angiography and risk of stroke and death: A cohort study. J Neurol Neurosurg Psychiatry. 2004;75:22-6.
- [Google Scholar]
- High-resolution computed tomography of the basilarartery, 2: Vertebrobasilar dolichoectasia: Clinical-pathological correlation and review. AJNR Am J Neuroradiol. 1986;7:61-72.
- [Google Scholar]
- Central sleep apnoea diaphragmatic paralysis associated with vertebral artery compression of the medulla oblongata. J Neurol. 2003;250:503-5.
- [Google Scholar]
- Recurrent subarachnoid hemorrhage from untreated ruptured vertebrobasilar dissecting aneurysms. Neurosurgery. 1995;36:905-11.
- [Google Scholar]
- Bulbar compression by an ectatic vertebral artery: A novel neurovascular construct relieved by microsurgical decompression. Neurosurgery. 2005;56:117-24.
- [Google Scholar]
- Posterior circulation infarcts in patients with vertebrobasilar dolichoectasia. Stroke. 1998;29:653-9.
- [Google Scholar]
- Clinical-angiographic correlation in 132 patients with megadolichovertebrobasilar anomaly. Neuroradiology. 1984;26:213-6.
- [Google Scholar]
- Vertebrobasilar arterial dolichoectasia: Complications and prognosis. Rev Neurol (Paris). 1991;147:714-22.
- [Google Scholar]
- Cardiovascular risk and neuroradiological profiles in asymptomatic vertebrobasilar dolichoectasia. Cerebrovasc Dis. 2010;30:23-8.
- [Google Scholar]
- Non-communicating hydrocephalus due to megadolichobasilar artery - case report. Neurol Med Chir (Tokyo). 1995;35:104-6.
- [Google Scholar]
- MRI in aqueduct compression and obstructive hydrocephalus due to an ecstatic basilar artery. Neuroradiology. 1993;35:447-8.
- [Google Scholar]
- Hydrocephalus caused by dolichoectatic basilar artery.Case report. J Neurosurg Sci. 2000;44:155-8.
- [Google Scholar]
- Vertebrobasilar dolichoectasia: A rare cause of obstructive hydrocephalus. B J Radiol. 2008;81:e123-6.
- [Google Scholar]
- Basilar megadolicho trunk causing obstructive hydrocephalus at the foramina of Monro. Surg Neurol. 2006;65:199-201.
- [Google Scholar]
- A peculiar mechanism of hydrocephalus: The “water-hammering” effect. Neurochirurgie. 1998;44:117-20.
- [Google Scholar]






