Translate this page into:
Does Gender Influence Electroconvulsive Therapy Sessions Required across Psychiatric Diagnoses? A 5-Year Experience from a Single Center
Address for correspondence: Dr. Vikas Menon, Department of Psychiatry, Jawaharlal Institute of Postgraduate Medical Education and Research, Dhanvantri Nagar, Puducherry - 605 006, India. E-mail: drvmenon@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Context:
There is a paucity of systematic data reflecting the practice of electroconvulsive therapy (ECT) from developing countries.
Aim:
We aimed to identify the number of ECT sessions required to yield response and gender diffeferences in the number of sessions across various diagnostic categories.
Setting and Design:
A record-based study from a teaching cum tertiary care hospital in South India.
Subjects and Methods:
Case records of patients who received modified ECT from January 2011 to January 2016 were reviewed. The sociodemographic details and ECT-related data were collected. Psychiatric diagnoses were ascertained as per the International Classification of Diseases, 10th Revision criteria.
Statistical Analysis Used:
Kruskal–Wallis test and Mann–Whitney U-test.
Results:
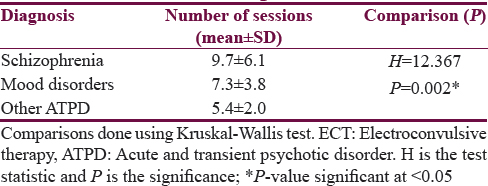
Among 148 patients, 82 (55.4%) had mood disorder (bipolar disorder and recurrent depressive disorder), 43 (29.1%) had schizophrenia, and 22 (14.9%) had other acute and transient psychotic disorders (ATPDs). Patients with mood disorders, schizophrenia, and other ATPD received 7.3 (± 3.8), 9.7 (± 6.1), and 5.4 (± 2.0) ECT sessions, respectively, to achieve response. There was no gender difference in the number of sessions received.
Conclusion:
Our findings show that number of ECT sessions required to yield response may be disorder-specific. Gender does not influence the ECT dose requirement. Variations in ECT parameters across settings may limit the generalizability of results.
Keywords
Acute psychosis
bipolar disorder
electroconvulsive therapy
psychiatry
schizophrenia
treatment response
INTRODUCTION
Electroconvulsive therapy (ECT) is a well-established and commonly utilized somatic treatment when psychiatrists encounter severe or refractory mental disorders such as major depression with prominent suicide risk, recalcitrant psychosis, and acute catatonic states with inadequate response to pharmacotherapy.[12] Despite concerns about its side effects, most patients and caregivers approach the procedure as a life-saving treatment.[3] Although many clinical guidelines are available on practice and indications of ECT,[45] literature has less to divulge on number of sessions required for clinical response across the spectrum of common indications and whether gender may be a determinant of the same.
Knowledge on the required number of sessions will inform us about patient education, plan hospital stay, implement treatment strategies, and importantly prevent various side effects. In India, common diagnoses for which ECT has been prescribed are schizophrenia and mood disorders and lastly catatonia as an independent indication.[6] Indications, legal requirements, and practice of ECT have been shown to vary considerably across settings. More pertinently perhaps, this is one area where fidelity to clinical guidelines has been found insufficient.[7] In such a scenario, it is important for countries to have a valid and representative database about use and practice of ECT. With this background, we aimed at ascertaining the number of ECT sessions required to yield response and the gender influence on number of sessions required in patients with diagnoses of schizophrenia, mood disorders, and other acute and transient psychiatric disorders (other ATPD). The last category was chosen because, in our center, patients presenting with acute onset catatonic signs with no preceding mood or psychotic features are commonly assigned this diagnosis. As there is no national ECT registry in India, the present study will provide real world data on use and practice of ECT.
SUBJECTS AND METHODS
Study design and setting
The current retrospective record-based study was conducted in a public sector, tertiary care general hospital psychiatric unit in Southern India. The unit offers both inpatient and outpatient services in its premises. All patients attending the outpatient department are initially screened by a qualified psychiatrist for psychiatric and physical morbidity. Those deemed to have underlying psychiatric morbidity are allotted a date for detailed evaluation. On this day, they are asked to come with a reliable informant and evaluated by a junior resident trainee psychiatrist. All psychiatric diagnoses are made as per the International Classification of Diseases, 10th Revision.[8] Subsequently, a detailed management plan is formulated after discussion with consultant psychiatrist and comprises pharmacotherapy, psychosocial strategies, and ECT as indicated. ECT is initiated on an inpatient basis and common indications are prominent suicidal behavior, catatonia, depressive stupor, acute excitement, or disruptive behavior not responding adequately to pharmacotherapy or where a rapid response is desirable. Patients with acute onset catatonia without any discernible mood or psychotic symptoms are assigned a diagnosis of other acute and transient psychotic disorders (ATPDs). Other less common indications include treatment-resistant delusions or hallucinations, especially in schizophrenia. The psychiatry unit of the institute maintains a comprehensive ECT register that stores information including diagnosis, severity of psychopathology, and treatment received, both with ECT and concurrent pharmacotherapy. The data are identified by unique patient hospital number. For the present study, data were collected from this register about all patients with diagnosis of schizophrenia, mood disorders (including depressive disorders and bipolar mood disorders), and other ATPD who underwent modified ECT during the 5-year period from January 2011 to January 2016. Data extracted from the register included relevant clinical profile, psychopathology ratings, ECT-related information such as indications, number of ECT sessions required for response, adverse outcomes, and reasons for termination of the procedure.
Electroconvulsive therapy procedure
Following is a brief description of the ECT procedure that is practiced in our psychiatry unit. Modified ECT using a brief-pulse ECT apparatus - NIVIQURE ICE60601/1TYPECE is being practiced in our center. After obtaining a high-risk written informed consent from the patients or their primary caregivers, ECT is administered at a frequency of two sessions per week. Anesthetic drugs used are atropine, thiopentone, and succinylcholine. Unless specifically indicated, all patients receive bitemporal threshold ECT. This refers to the practice of placing the center of the electrodes 2–3 cm above the midpoint of the line connecting the outer canthus of the eye and the external auditory meatus of each side.[9] In threshold ECT, seizure threshold is estimated in the first sitting, and subsequently, the same electrical dosage is continued in further sittings which has been shown to be comparable in efficacy but with fewer side effects for a range of psychiatric disorders and hence is practiced routinely in our center.[1] Treatments are continued till patient achieves clinical remission or until a plateau in benefits is observed or upon the emergence of adverse effects that preclude continuation of ECT or if patients withdraw their consent as per standard guidelines.[4]
Statistical analysis
Frequencies and percentages were used to represent categorical variables. Means and standard deviations were used to represent continuous variables. Diffeferences in number of ECT sessions required and gender influences across diagnoses were compared using Kruskal–Wallis test and Mann–Whitney U-test, respectively.
RESULTS
Over a 5-year period, 148 patients were administered ECT either as inpatients or outpatients. The sample comprised 60 males and 88 females. The mean age of the sample was 29.5 (± 11.3) years. The age range of the sample was between 18 and 61 years.
The distribution of diagnosis showed that mood disorders (bipolar affective disorder and recurrent depressive disorder) were the baseline diagnosis in more than half (55.4%, n = 82) of the individuals who underwent ECT. Schizophrenia was the diagnosis in 43 patients (29.1%) and other ATPDs in 22 patients (14.9%). The baseline diagnosis was not available in 1 patient. Subsequently, the total number of ECT sessions administered for each diagnostic category was analyzed [Table 1]. In the schizophrenia group (n = 43), patients received a mean of 9.7 (± 6.1) sessions of ECT while patients in the mood disorders (n = 82) category received a mean of 7.3 (± 3.8) sessions. Patients who had a diagnosis of other ATPDs (n = 22) received a mean of 5.4 (± 2.0) sessions. These diffeferences were statistically significant as per the Kruskal–Wallis test. We did not have data on the number of ECT sessions needed for two patients.
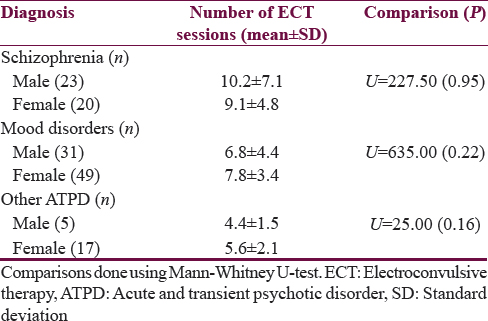
Although females with mood disorders and acute transient psychotic disorders required more number of ECT sessions than their male counterparts, the reverse was true for schizophrenia [Table 2]. However, none of these diffeferences were statistically significant.
DISCUSSION
Among the 148 patients who were administered ECT, mood disorder was the most frequent diagnosis followed by schizophrenia and other ATPD. This finding is in variance with earlier reports of ECT practice in Asia, where schizophrenia was observed to be the most common diagnosis.[6] Our findings may be artefactual as our sample had more females and affective diagnoses are more commonly encountered in females.[10] Hence, more studies from other centers in the country are required to validate these results.
The average number of ECT sessions required to yield therapeutic response in patients with schizophrenia, mood disorders, and other ATPD approximately coincide with that reported in cross-cultural literature.[11112] Similar to our results, catatonia as the sole indication for ECT has been shown to respond earlier compared to mood disorders and schizophrenia.[13] Our findings are also in line with systematic reviews on ECT practice, which have concluded that the minimum number required can range from 12 to 20 in schizophrenia,[3] 5–6 in catatonia,[13] 6–12 in mood disorders.[114]
The statistically significant difference in the number required across the three diagnoses indicates that the dose requirement to achieve response might be disorder-specific. However, one should exert caution in interpreting these findings as there are considerable variations in ECT parameters such as mode of delivery and electrode placement – unilateral or bifrontal or bitemporal,[15] intensities – threshold and suprathreshold,[1617] and frequency of sessions and variations in pulse–width – brief and ultrabrief,[12] all of which may conceivably influence stimulus dosing and response to ECT. Here, we have employed bitemporal threshold ECT for cases which, according to our knowledge, is most commonly practiced across India.
Previous studies have looked into the gender influence on the electrical charge delivered during ECT.[18] The present study is one of the few attempts to check the gender influence on number of ECT sessions. We could not find any significant effect of gender on ECT sessions required to induce a response across diagnostic categories. These findings are consistent with those from other cultures[19] and in resonance with the hypothesis that response to ECT is gender-neutral.[20] However, the skewed nature of our sample and inadequate numbers in subcategories such as other ATPD may indicate that these findings are not conclusive. Limitations of the study include its retrospective design, possible selection bias by virtue of being a single-center study, and nonmatching of sample across the studied groups. Further, we did not analyze gender diffeferences in electrical charge delivered during sessions or diffeferences in reasons for termination of ECT as we did not have access to this data. Given the naturalistic study design, the results are not affected by constraints of patient selection and ensuring strict protocols as in clinical trials. For this reason, they are also more reflective of real-world practice of ECT in Indian settings.
CONCLUSION
Mean number of ECT sessions are least for catatonia followed by mood disorders and schizophrenia. Number of sessions and dose required to achieve response may be disorder-specific. ECT-induced clinical response in major psychiatric disorders is independent of gender.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank the faculty and residents of the Department of Psychiatry, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India, for their timely help at various stages of this research. We also thank Dr. Siddharth Sarkar, Assistant Professor, National Drug Dependence and Treatment Center, All India Institute of Medical Sciences, New Delhi, for his contribution toward data collection.
REFERENCES
- Speed of response to threshold and suprathreshold bilateral ECT in depression, mania and schizophrenia. J Affect Disord. 2009;117:104-7.
- [Google Scholar]
- Electroconvulsive therapy and its different indications. Dialogues Clin Neurosci. 2008;10:105-17.
- [Google Scholar]
- Perceptions and awareness of electroconvulsive therapy among patients and their families: A review of the research from developing countries. J ECT. 2010;26:317-22.
- [Google Scholar]
- 2003. National Institute for Clinical Excellence. Guidance in the Use of Electroconvulsive Therapy (Technology Appraisal Guidance 59). London: NICE; Available from: https://www.nice.org.uk/guidance/ta59
- College guidelines on electroconvulsive therapy: An update for prescribers. Adv Psychiatr Treat. 2005;11:150-6.
- [Google Scholar]
- A survey of the practice of electroconvulsive therapy in Asia. J ECT. 2010;26:5-10.
- [Google Scholar]
- Contemporary use and practice of electroconvulsive therapy worldwide. Brain Behav. 2012;2:283-344.
- [Google Scholar]
- WHO. The ICD-10 Classification of Mental and Behavioural Disorders. Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization; 1992.
- Bifrontal, bitemporal and right unilateral electrode placement in ECT: Randomised trial. Br J Psychiatry. 2010;196:226-34.
- [Google Scholar]
- Electroconvulsive therapy in catatonic patients: Efficacy and predictors of response. World J Psychiatry. 2015;5:182-92.
- [Google Scholar]
- Ultra-brief pulse ECT in bipolar and unipolar depressive disorder: Diffeferences in speed of response. Bipolar Disord. 2009;11:418-24.
- [Google Scholar]
- Does catatonic schizophrenia improve faster with electroconvulsive therapy than other subtypes of schizophrenia? World J Biol Psychiatry. 2009;10:772-7.
- [Google Scholar]
- Use of electroconvulsive therapy in a state hospital: A 10-year review. J Clin Psychiatry. 2000;61:534-9.
- [Google Scholar]
- A retrospective chart audit of electroconvulsive therapy at a regional Australian hospital. Australas Psychiatry. 2016;24:493-6.
- [Google Scholar]
- Electrical dose and seizure threshold: Relations to clinical outcome and cognitive effects in bifrontal, bitemporal, and right unilateral ECT. J ECT. 2000;16:361-9.
- [Google Scholar]
- Effects of stimulus intensity on the efficacy and safety of twice-weekly, bilateral electroconvulsive therapy (ECT) combined with antipsychotics in acute mania: A randomised controlled trial. Bipolar Disord. 2009;11:126-34.
- [Google Scholar]
- Electroconvulsive therapy clinical database: Influence of age and gender on the electrical charge. Rev Psiquiatr Salud Ment 2016 pii: S1888-989100191-3
- [Google Scholar]
- Is There a Role of Gender in Electroconvulsive Therapy Response? Klinik Psikofarmakoloji Bülteni-Bulletin of Clinical Psychopharmacology. 2015;25:228-32.
- [Google Scholar]
- Sex diffeferences relating to psychiatric treatment. Can J Psychiatry. 1999;44:362-7.
- [Google Scholar]






