Translate this page into:
Disseminated neurocysticercosis presenting as affective mood disorder with chronic tension type headache
Address for correspondence: Dr. Krishnarpan Chatterjee, Room No. 210, Doctor's Hostel, Dr. RML Hospital, New Delhi - 110 001, India. E-mail: krishnarpan.chatterjee@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Neurocysticercosis is a common parasitic infection in India presenting usually with seizues, headache, focal neurological deficits. Neurocysticercosis presenting as a psychiatric illness is rare. Disseminated cysticercosis with involvement of central nervous system and head and neck muscles is rare even in endemic areas. We present a case of disseminated cysticercosis, which presented with chronic tension type headache and affective mood disorder. Treatment with cysticidal drugs led to complete remission of psychiatric complaints. In endemic areas history suggestive of mood disorder should not be used as supportive evidence of a primary headache syndome like tension type headche without ruling out secondary causes. Making an early diagnosis can prevent morbidity.
Keywords
Affective mood disorder
chronic tension type headache
disseminated cysticercosis
Introduction
Cysticercosis is caused by the encysted larvae of the pork tapeworm, Taenia solium. We present a case of disseminated cysticercosis with extensive central nervous system (CNS) involvement and extracranial dissemination in a young woman, which presented as a case of affective mood disorder with the chronic tension type headache. The extra-cranial dissemination involved atypical head and neck regions such as posterior pharyngeal wall, masseter, pterygoids, paravertebral neck muscles and tongue. Treatment of cysticercosis led to remission of the depressive episode and primary headache disorder. Though cysticercosis is the most common helminthic infection of the, CNS disseminated cysticercosis is rare.[12] Less than 50 cases of disseminated cysticercosis have been reported world-wide.[3] A few cases of neurocysticercosis presenting with psychiatric complaints have been reported, but there have been no reported cases of disseminated neurocysticercosis presenting with depression.[4]
Case Report
A 21-year-old woman residing in New Delhi presented to the Department of Medicine with a history of insidious onset, progressive headache on and off for the past 6 months. The headache was bilateral, dull aching in nature occurring at any time of the day and had no special character or precipitating factors. It was not associated with vomiting. It was associated with fatigue, low mood, irritability and loss of appetite, multiple somatic pains and crying spells. Initially, the headache was relieved by over the counter analgesics, but it used to recur after a few days. After 2 months of persistent symptoms, she had consulted a physician where she had been diagnosed to have tension type headache. A formal psychiatric evaluation done at that time revealed minor depressive episode. When her symptoms did not abate she was started on amitriptyline 25 mg once daily for prophylaxis of chronic tension type headache. When she presented to our hospital her headache had worsened in severity and frequency. There was no history of blurring of vision, diplopia, squint, pain, redness or watering of eyes. There was no history suggestive of any other cranial nerve palsy. There was no history of vomiting or seizures. There were no medical comorbidities. Her elder sister had a history of seizure disorder for which she had been taking anti-epileptic drugs for the past 2 years. The general examination was unremarkable. There were no subcutaneous swellings. Visual acuity was 6/6 in both eyes. Visual fields were normal. Cranial nerve examination was normal. There were no signs of meningeal irritation. Rest of the CNS examination was normal and fundoscopy was normal. Rest of the systemic examination was normal. Raised intracranial tension (ICT) leading to secondary headache was suspected. A non-contrast computed tomography of the head showed multiple hypodense lesions. A contrast enhanced magnetic resonance imaging was done, which showed multiple cystic lesions with eccentric nodules in bilateral basal ganglia, cerebellum, brainstem, cerebral hemispheres; a few of them indenting the lateral ventricle. Many ring enhancing lesions were also visualized throughout the brain parenchyma. Similar lesions were seen in the scalp, posterior pharyngeal wall, masseter, pterygoids, paravertebral neck muscles and tongue [Figure 1]. There was a single lesion in left orbit abutting the superior rectus and a single lesion in the right orbit abutting the optic nerve [Figures 2 and 3]. X-ray of the thigh showed multiple cigar shaped calcifications [Figure 4]. Her complete blood count, liver function test, kidney function test were within the normal limits. Based on the imaging findings a definite diagnosis of neurocysticercosis with extra-cranial dissemination was made. Amitriptyline was stopped. She was started on albendazole with oral steroids and neuroimaging follow-up was planned. After 2 months follow-up, her headache had decreased and she did not complain of any myalgia. There was remission of her affective mood disorder as documented by a psychiatry consultation.
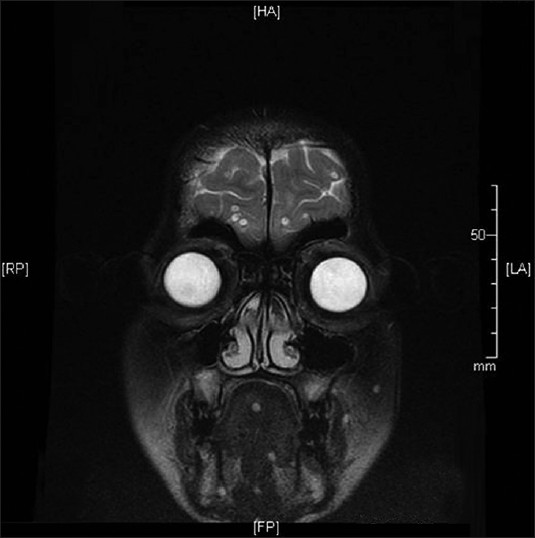
- Magnetic resonance imaging showing cystic lesions in masseter, pterygoids, tongue and cerebral hemispheres
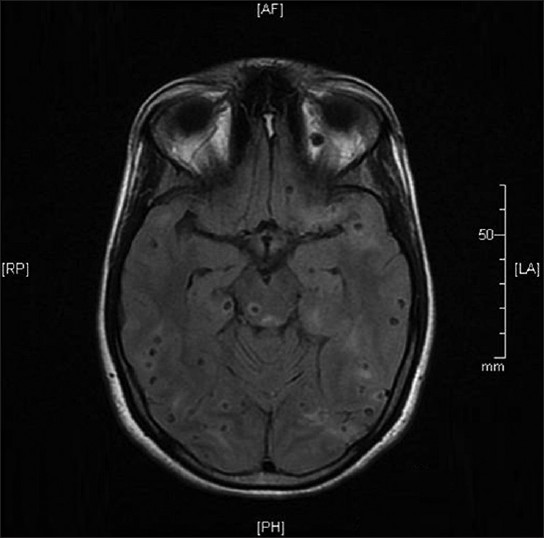
- Magnetic resonance imaging brain showing multiple hypodense lesions in bilateral brain parenchyma with scolices and surrounding edema. Single cystic lesion in left orbit abutting optic nerve
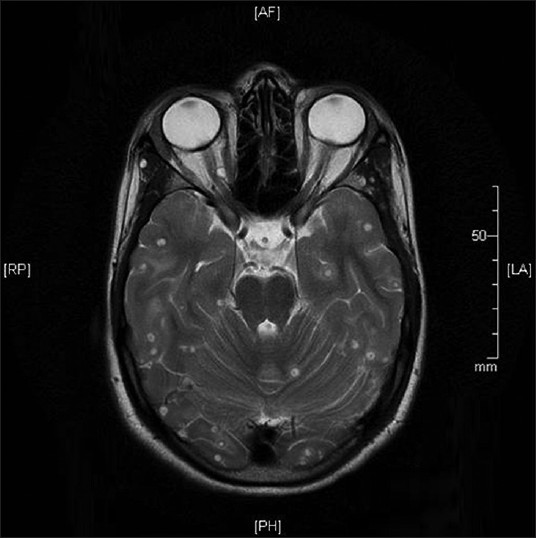
- Magnetic resonance imaging brain with cystic lesion in right orbit compressing optic nerve and superior oblique muscle

- Plain X-ray of thigh showing multiple cigar-shaped calcifications
Discussion
Cysticercosis occurs due to the feco-oral transmission of the T. solium egg. Consumption of measly pork containing cysticerci leads to intestinal teniasis, but does not directly cause cysticercosis. When cysticerci involve the CNS it leads to neurocysticercosis. Brain parenchyma is the most commonly involved site in the CNS. Cysticerci also occur in the skeletal muscles. Cases of disseminated cysticercosis have been reported from India with involvement of subcutaneous tissues, skeletal muscles, heart, lungs, spleen, pancreas and liver.[56] Cysticerci are uncommon in the head and neck region apart from the orbit but cases of cysticerci of tongue, masseter, mylohyoid, lower lip, soft palate and sternocleidomastoid have been reported previously.[78]
Neurocysticercosis can present with seizures, headache, focal neurological deficit, encephalitis, dementia.[910] Neurocysticercosis presenting as extrapyramidal disease (Parkinsonism and focal dystonia), Kluver-Bucy syndrome, Weber's syndrome and cortical blindness have also been reported.[11] There have also been reports of neurocysticercosis presenting as psychosis or psychiatric illness.[412] Hamed and El-Metaal reported a case of neurocysticercosis presenting with depressive manifestations together with disturbance of writing, mild deep sensory loss, limb-kinetic apraxia, lack of coordination and dystonia of the right upper limb.[13] Disseminated cysticercosis presenting as a mood disorder and mimicking a primary headache disorder has not been reported before. In our patient, the multiple somatic pains could be attributed to skeletal muscle cysticerci. These complaints as well as the minor depressive episode resolved with treatment of cysticercosis. Treatment of neurocysticercosis remains controversial. Our patient was treated with albendazole and oral steroids according to the consensus guidelines published by García et al.[14]
The diagnosis of tension type headache is clinical and relies on characteristic symptoms.[15] A detailed history and thorough examination to rule out secondary causes is mandatory. Traditionally, tension type headache has been believed to have a psychological basis. Even though studies have proved the neurobiological basis of these headaches, the psychological connotations of this diagnosis remain in the minds of physicians and it is easy to leap to this diagnosis in a clinical background of low mood, crying spells and other psychiatric complaints. Our case report highlights the pitfalls of rushing into such a diagnosis. Routine use of imaging modalities may be justified to rule out neurocysticercosis in endemic areas before making a diagnosis of a primary headache disorder. An early diagnosis of cysticercosis and cysticidal treatment can prevent considerable morbidity in this setting.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Neurocysticercosis: Updates on epidemiology, pathogenesis, diagnosis, and management. Annu Rev Med. 2000;51:187-206.
- [Google Scholar]
- Disseminated cysticercosis in a child: Whole-body MR diagnosis with the use of parallel imaging. Pediatr Radiol. 2010;40:223-7.
- [Google Scholar]
- Neurocysticercosis presenting with psychosis. J Assoc Physicians India. 2004;52:663-5.
- [Google Scholar]
- Disseminated cysticercosis with pulmonary and cardiac involvement. Indian J Radiol Imaging. 2010;20:310-3.
- [Google Scholar]
- Imaging findings of disseminated cysticercosis with unusual involvement of spleen and pancreas. J Glob Infect Dis. 2011;3:306-8.
- [Google Scholar]
- Isolated cysticercosis cellulosae of sternocleidomastoid muscle: A case report with review of literature. Indian J Otolaryngol Head Neck Surg. 2011;63:127-30.
- [Google Scholar]
- Mylohyoid cysticercosis: A rare submandibular mass. Ear Nose Throat J. 2009;88:1218-20.
- [Google Scholar]
- The clinical spectrum of neurocysticercosis in the Uttaranchal region. J Assoc Physicians India. 2002;50:1398-400.
- [Google Scholar]
- Neurocysticercosis: A review of current status and management. J Clin Neurosci. 2009;16:867-76.
- [Google Scholar]
- Pleomorphism of the clinical manifestations of neurocysticercosis. Trans R Soc Trop Med Hyg. 2006;100:134-41.
- [Google Scholar]
- Neurocysticercosis presenting as psychiatric illness. Indian J Pediatr. 2001;68:1073-4.
- [Google Scholar]
- Current consensus guidelines for treatment of neurocysticercosis. Clin Microbiol Rev. 2002;15:747-56.
- [Google Scholar]






