Translate this page into:
Depression in elderly patients with Alzheimer dementia or vascular dementia and its influence on their quality of life
Address for correspondence: Dr. Yaroslav Winter, Department of Neurology, Philipps-University Marburg, Baldingerstrasse, 35043 Marburg. E-mail: yaroslav.winter@med.uni-marburg.de
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Alzheimer dementia (AD) and vascular dementia (VD) are the most common causes of dementia in the elderly. Depression is an important co-morbid disorder in these diseases, which is often challenging to recognize. We investigated the prevalence of depression in patients with AD and VD and estimated the influence of depression on the health-related quality of life (HrQoL) in these patients.
Materials and Methods:
We evaluated prevalence of depression in consecutively recruited patients with AD or VD (n= 98). Depression was diagnosed according to criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and scored using the Geriatric Depression Scale. The EuroQol (EQ-5D and visual analogue scale) was applied to evaluate HrQoL. The severity of cognitive impairment was measured by the Mini-Mental State Examination (MMSE). Multiple regression analysis was used to identify factors predicting severity of depression.
Results:
The prevalence of depression in AD/VD was 87%. In comparison to the general population, HrQoL measured on the visual analogue scale was reduced by 54% in patients with AD/VD. In the dimension “anxiety/depression” of the EQ-5D, 81% of patients with AD/VD had moderate or severe problems. Depression showed significant association with reduced HrQoL (P<0.01). Independent predictors of more severe depression were older age, male gender, better MMSE scores and being not married.
Conclusions:
Depression is a prevalent psychiatric co-morbidity in patients with AD/VD, which is often under-diagnosed being masked by cognitive impairment. Depression is a predictor of reduced HrQoL in elder people with AD/VD. Therefore, they should be screened for presence of depressive symptoms and receive adequate antidepressant treatment.
Keywords
Alzheimer dementia
depression
health-related quality of life
prevalence
vascular dementia
Introduction
The ageing of the world population results in the increasing prevalence of neurodegenerative diseases in the elderly . Neurodegenerative diseases are among the major causes of disability and death in the elderly. Alzheimer's disease is the most common neurodegenerative disorder and the most prevalent cause of dementia in the elderly followed by vascular dementia. According to the World Alzheimer Report released by Alzheimer Disease International, the estimated number of people with dementia exceeded 35 million in 2010 and will double every 20 years to 65.7 million in 2030 and 115.4 million in 2050.[1]
Neurodegenerative diseases lead not only to impairment of cognitive and motor function but also to development of non-motor disorders, such as depression. Diagnosis of depression in neurodegenerative diseases that produce psychomotor impairment can be challenging and requires particular experience. The early diagnosis of depression is also important in the context of the health-related quality of life (HrQoL). Depression was identified in recent studies as an independent factor influencing HrQoL in a number of neurological diseases.[2–5] Health-related quality of life is a concept reflecting the self-perceived wellbeing that is related to health status.
The objective was to investigate the prevalence of depression in patients with Alzheimer dementia and vascular dementia and estimate the influence of depression on the health-related quality of life in these diseases.
Materials and Methods
Study design
We recruited consecutive patients with Alzheimer dementia (AD) or vascular dementia (VD) (n=98), which are the most prevalent types of dementia. Diagnosis of AD and VD was based on criteria proposed by the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer's Disease and Related Disorders Association (NINCDS-ADRDA Alzheimer's Criteria).[67]
Patients were recruited in the Department of Psychiatry and Psychosomatics, Sklifosovski Research Institute, Moscow, Russia. The study design was approved by the local ethic committees and all patients gave informed consent for participation.
Clinical evaluation
Patients with AD or VD received a complete medical and neurological examination performed by a specialist (study investigator) with at least five years experience in dementia.
All clinical and demographic data were documented in specially developed case report forms (CRFs). The CRF included the following parts:
-
Demographics and social data.
-
Clinical data (disease onset, duration of disease, time from first manifestation to diagnosis, severity scales and co-morbid disorders)
-
Depression scale (Geriatric Depression Scale)
-
Health-related quality of life measurements (EQ-5D).
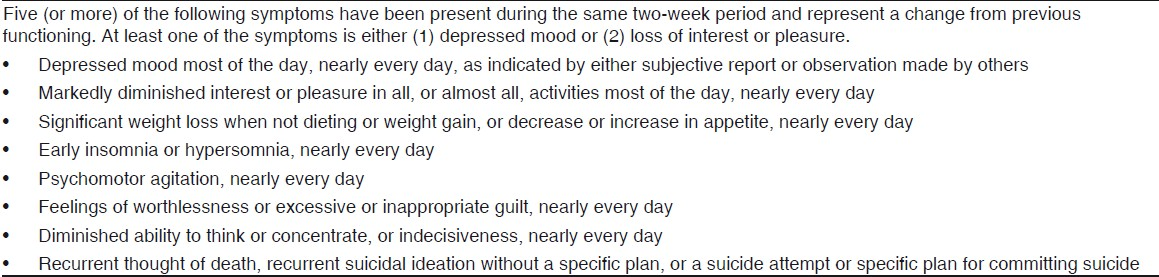
Severity of cognitive impairment was evaluated using the Mini-Mental State Examination (MMSE), which is a valid and most common tool for assessment of cognitive deficits in dementia.[8] Depression was diagnosed according to criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) [Table 1]. Severity of depressive symptoms was measured using the Geriatric Depression Scale. The Geriatric Depression Scale (GDS) is a standardized and validated self-report questionnaire used to identify depression in the elderly. It is based on yes-or-no questions regarding mood over the previous week with higher scores on GDS indicating more severe depression.[9] The test allows 84% sensitivity and 95% specificity in detection of depression. The following cut-offs for GDS were used: score of 0–9 is considered normal; 10–19 indicates mild depression, and a score ≥20 indicates severe depression.
Health-related quality of life
The evaluation of HrQoL was performed using EuroQol. The EuroQol is a valid standardized health state measure.[10] It consists of a self-classifier (EQ-5D) and a visual analogue scale (VAS). The self-classifier evaluates five dimensions of health: mobility, self-care, usual activities, pain/discomfort and anxiety/depression.[1112] Each dimension is divided into three levels of severity (1=no problem, 2=moderate problem, 3=severe problem). The EQ-5D-index score was calculated according to the European recommendations.[13] The visual analogue scale is a thermometer type scale ranging from 0 (worst imaginable health state) to 100 (best imaginable health state).[14]
Statistical analysis
Statistical analysis was performed using SPSS Version 15.0 (SPSS Inc., Chicago, IL, USA).All data are presented as mean, standard deviation (SD) and median. The Kolmogorov-Smirnov test was used to test the data for normal distribution. For group comparisons of data not following normal distribution, either the Mann-Whitney U test (two independent groups), the Kruskal Wallis test (more than two independent groups) or the Wilcoxon rank test (two dependent groups) were applied. Significance level was set at 5%. Multiple regression analysis was used to identify factors predicting severity of depression. The R2 method was used to explore the variability accounted for by predicting factors.[15]
Results
Sociodemographic and clinical data
The age of the study participants with AD or VD was 77.5±8.8 years. The proportion of female patients was 65.3%. Demographics and clinical data are shown in Table 2. More than 90% of patients were age retired. The proportion of widowed patients increased with growing age. Forty-four percent of patients (n=43) with AD or VD were widowed.
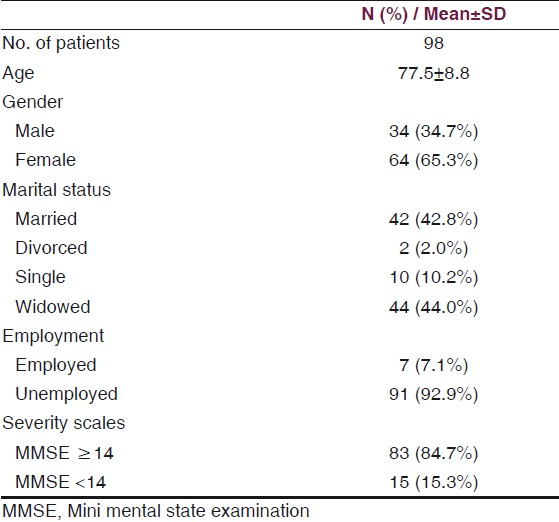
In study population, 84.7% (n=83) patients had moderate cognitive impairment (MMSE≥14) and 15.3% (n=15) had severe cognitive deficits (MMSE<14). Extrapyramidal symptoms had 73.5% (n=72) of patients. Behavioral disorders were present in 43.9% (n=43) patients.
Depression and health-related quality of life
The prevalence of depressive symptoms in patients with AD or VD was 86.7% (n=85). Fifty-six percent (n=55) of patients had moderate depression and 36% (n=35) of patients had severe depression as measured on the GDS. The prevalence of other mental disorders in the study population was lower: 30.6% (n=30) of patients had psychotic symptoms, 43.9% (n=43) of patients had behavioral disorders, 9.2% (n=9) of patients had alcohol dependency. Only 40% of patients with manifest depression were provided with adequate antidepressant treatment.
The health-related quality of life was considerably reduced in our patients with AD or VD. In dimensions of “mobility”, “self-care”, “usual activities”, “pain/discomfort” and “anxiety/depression” of the EQ-5D, severe problems were found in 25.5%, 32.7%, 36.7%, 14.3% and 20.4% of patients, respectively. The mean EQ-5D index score was 36.7±18.5. The mean score on the EQ-VAS was significantly decreased in comparison to the general population (34.0±13.8 versus 77.0±20.8, P<0.01).[16] The association between HrQoL and age is shown in Table 3. The values on the EQ-VAS and EQ-5D index decreased with increasing age. No associations between gender and HrQoL were revealed.
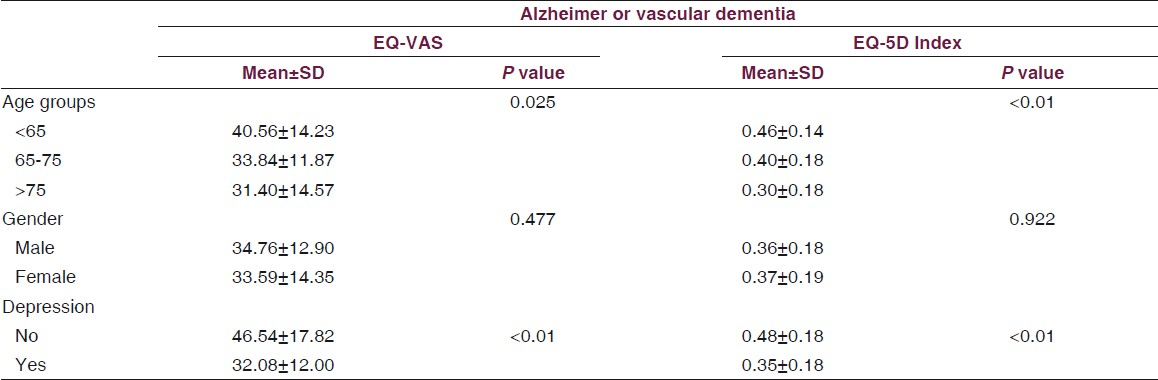
In the dimension “anxiety/depression” of the EQ-5D, 81% of patients with AD or VD had moderate or severe problems. Depression showed a strong association with reduced HrQoL [Table 3]. The presence of depression reduced the HrQoL in patients with AD or VD by 14% (P<0.01).
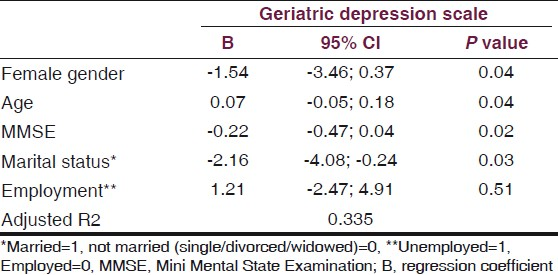
Multiple regression analysis identified age, gender, MMSE and marital status to be independent predictors of depression severity in AD or VD [Table 4]. All together, these four variables could explain 33.5% of variability in scores on the GDS. Older age and male gender were associated with more severe depression. Married patients had lower prevalence of depression. Employment status was not associated with depression. Interestingly, the severity of depression had a reverse association with severity of cognitive impairment [Table 4 and Figure 1].
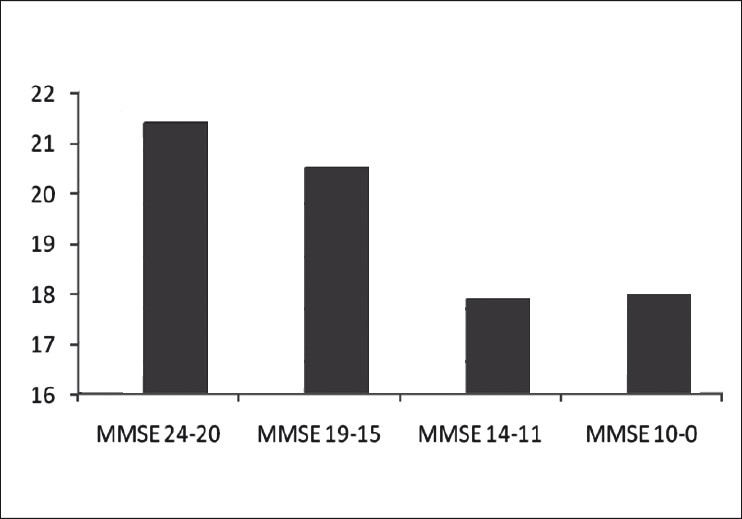
- Measures on the geriatric depression scale depending on severity of dementia
Discussion
In this study, we investigated the prevalence of depression in the most common types of dementia in elderly patients and its influence on their HrQoL. Depression was found to be the most prevalent psychiatric co-morbidity in AD or VD. Depressive symptoms were found in up to 87% of patients depending on the severity of cognitive impairment.
Depression in the elderly is a challenging condition being associated with an increased rate of morbidity and reduced life expectancy.[17–19] Depending on the country and study design (urban versus rural, outpatients versus inpatients), prevalence rates reported in the literature range from 1–40%.[1720] In the meta-analysis by Barua et al., mean prevalence of depression in the elderly population worldwide was 10.3%.[17] In rural communities, the prevalence of depression is often higher.[21] Our patients were recruited in Russia, where accessibility and quality of healthcare is reduced in comparison to Western European countries. Although there is a mandatory health insurance in Russia, it covers only essential medical services.[22] Lower accessibility and quality of healthcare is associated with higher prevalence of depression in elderly Russian population compared to population of the Western European countries. Correspondingly, elderly Russian patients with dementia in our study have higher prevalence of depression than it was shown in patients with dementia living in the Western Europe .[2324]
The prevalence of depressive symptoms in people with chronic illnesses or disability is increased.[19] In particular, prevalence rates of depression in the elderly with neurodegenerative diseases are strikingly high. For example, prevalence rates of depression in Parkinson's disease and AD reported in a recent review were 75% and 87%, respectively.[25] However, diagnosis of depression in neurological disorders is challenging due to overlapping of motor deficits and cognitive impairment.[26] Neuropsychiatric symptoms are prevalent in patients with AD or VD. In a recent prospective study from the Netherlands, they were found in 97% residents of 14 dementia special care units.[27] In our study, 86.7% of patients with AD or VD had depressive symptoms. Dementia was identified as a risk factor for depression in the elderly in a recent meta-analysis.[28] Compared to the elderly without dementia, elderly people with dementia had higher prevalence rates of depression (OR: 3.92, 95% CI: 1.93-7.99, respectively). Unfortunately, depression is often under-diagnosed in AD and VD. Depressive symptoms can be overlooked not only by physicians and nurses but also by caregivers providing daily care to demented patients. For example, loss of interest and apathy can be mistaken for symptoms of cognitive impairment. The results of a study by Watson et al., show that one-third of cases with manifest depression in patients with dementia were not identified by their caregivers.[29] The sensitivity of caregivers' accuracy in recognizing depression was 0.65 (95% CI: 0.55, 0.75). The specificity was 0.58 (95% CI: 0.50, 0.66). Caregivers also experienced depression related to caregiving. It was diagnosed in 12% of caregivers. However, the presence of a caregiver from family members can probably reduce the occurrence of depressive symptoms. In our study, being married was associated with lower prevalence of depression.
Depression in elderly people with neurodegenerative diseases is associated with decreased HRQoL. Corresponding with the results of studies by Banerjee et al., and Wetzels et al., depression was a predictor of reduced HRQoL in the elderly with AD or VD.[3031]
Our study has some limitations
Referral-based design was used for recruitment. An epidemiological study with door-to-door data collection would provide more precise data. We cannot exclude a selection bias towards more severe disease stages in our sample. Patients with minimal cognitive deficits (MCI) or those in early stages of dementia less often consult general practitioners, neurologists or psychiatrists. We applied a generic HRQoL instrument (EuroQol), which is less sensitive to disease-specific changes of health-related quality of life. However, we sought to evaluate the general HRQoL and provide data suitable for a comparison between these patients and the general population. Mini Mental State Examination is a less specific tool for assessment of cognitive deficits in AD than ADAS-Cog and is also less specific than VADAS-Cog in VD. However, MMSE is a valid and well-known measure for estimation of cognitive impairment in different types of dementia. We included patients with two different types of dementia and applied one standardized instrument (MMSE) instead of two disease-specific measures in order to collect homogenous neuropsychological data. The cross-sectional design of our study does not provide any information on changes in depression severity and HRQoL over time.
Conclusion
Depression is a prevalent psychiatric co-morbidity in the elderly with Alzheimer dementia or vascular dementia. Unfortunately, depressive symptoms are often under-recognized in these diseases being masked by cognitive impairment. Depression is a predictor of reduced HrQoL in elderly people with dementia, therefore, they should be screened for presence of depressive symptoms and receive adequate antidepressant therapy.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Alzheimer's Disease International. World Alzheimer Report. Available from: http://www.alz.co.uk/research/files/WorldAlzheimerReport-ExecutiveSummary.pdf
- [Google Scholar]
- Longitudinal study of the socioeconomic burden of Parkinson's disease in Germany. Eur J Neurol. 2010;17:1156-63.
- [Google Scholar]
- Health-related quality of life in ALS, myasthenia gravis and facioscapulohumeral muscular dystrophy. J Neurol. 2010;257:1473-81.
- [Google Scholar]
- Social and clinical determinants of quality of life in Parkinson's disease in Austria: A cohort study. J Neurol. 2010;257:638-45.
- [Google Scholar]
- Health-related quality of life in patients with subarachnoid haemorrhage. Cerebrovasc Dis. 2010;30:423-31.
- [Google Scholar]
- Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34:939-44.
- [Google Scholar]
- Vascular dementia: Diagnostic criteria for research studies: Report of the NINDS-AIREN International Workshop. Neurology. 1993;43:250-60.
- [Google Scholar]
- “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189-98.
- [Google Scholar]
- Development and validation of a geriatric depression screening scale: A preliminary report. J Psychiatr Res. 1982;17:37-49.
- [Google Scholar]
- Testing the validity of the EuroQoL and comparing it with the SF-36 health survey questionnaire. Qual Life Res. 1993;2:169-80.
- [Google Scholar]
- The EuroQol instrument: An index of health-related quality of life. In: Spilker B, ed. Quality of life and pharmacoeconomics in clinical trials. Philadelphia: Lippincott-Raven; 1996.
- [Google Scholar]
- The EuroQol Group. EuroQol: A new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199-208.
- [Google Scholar]
- A single European currency for EQ-5D health states: Results from a six-country study. Eur J Health Econ. 2003;4:222-31.
- [Google Scholar]
- Health Status of the German population: results of a representative survey using the EuroQol questionnaire. Gesundheitswesen. 2005;67:173-82.
- [Google Scholar]
- Comparison of population health status in six European countries: Results of a representative survey using the EQ-5D questionnaire. Med Care. 2009;47:255-61.
- [Google Scholar]
- Distribution of depressive disorders in the elderly. J Neurosci Rural Pract. 2010;1:67-73.
- [Google Scholar]
- Predictors of mortality among elderly people living in a south Indian urban community: A 10/66 Dementia Research Group prospective population-based cohort study. BMC Public Health. 2010;10:366.
- [Google Scholar]
- Comorbidity of late life depression: An opportunity for research on mechanisms and treatment. Biol Psychiatr. 2002;52:543-58.
- [Google Scholar]
- Prevalence and predictors of depression in populations of elderly: A review. Acta Psychiatr Scand. 2006;113:372-87.
- [Google Scholar]
- Nature, prevalence and factors associated with depression among the elderly in a rural south Indian community. Int Psychogeriatr. 2009;21:372-8.
- [Google Scholar]
- Costs of illness in a Russian cohort of patients with Parkinson's disease. Pharmacoeconomics. 2009;27:571-84.
- [Google Scholar]
- Neuropsychiatric symptoms and quality of life in patients with very mild and mild Alzheimer's disease. Int J Geriatr Psychiatry 2010 in press
- [Google Scholar]
- Prevalence of neuropsychiatric symptoms in a large sample of Dutch nursing home patients with dementia. Int J Geriatr Psychiatry. 2007;22:632-8.
- [Google Scholar]
- Assessment of depression in three medically ill, elderly populations: Alzheimer's disease, Parkinson's disease, and stroke. Clin Neuropsychol. 2009;23:205-30.
- [Google Scholar]
- Depression in neurological disorders: Parkinson's disease, multiple sclerosis, and stroke. J Neurol Neurosurg Psychiatry. 2005;76:i48-52.
- [Google Scholar]
- Course of neuropsychiatric symptoms in residents with dementia in nursing homes over 2-year period. Am J Geriatr Psychiatry. 2010;18:1054-65.
- [Google Scholar]
- Cognitive function and risk for depression in old age: A meta-analysis of published literature. Int Psychogeriatr. 2010;12:1-10.
- [Google Scholar]
- Perceptions of depression among dementia caregivers: Findings from the CATIE-AD trial. Int J Geriatr Psychiatry 2010 in press
- [Google Scholar]
- Quality of life in dementia: More than just cognition: An analysis of associations with quality of life in dementia. J Neurol Neurosurg Psychiatry. 2006;77:146-8.
- [Google Scholar]
- Determinants of quality of life in nursing home residents with dementia. Dement Geriatr Cogn Disord. 2010;29:189-97.
- [Google Scholar]






