Translate this page into:
Demography, types, outcome and relationship of surgically treated intracranial suppuration complicating chronic suppurative otitis media and bacterial rhinosinusitis
Address for correspondence: Dr. Olufemi Emmanuel Idowu, Department of Surgery, Neurosurgery Division, Lagos State University College of Medicine, Ikeja, Lagos, Nigeria. E-mail: oeidowu412@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Surgically treated intracranial suppurations (ICS) are uncommon, life-threatening neurosurgical emergencies. They can result from complication of chronic suppurative otitis media (CSOM) and bacterial rhinosinusitis (BRS). The objective of this study was to know the frequency of BRS and CSOM and relate it to its rare complication of surgically treated ICS while also describing the demography, type and outcome of ICS that resulted from BRS and CSOM.
Materials and Methods:
All patients that presented to the Otorhinolaryngological department and Neurosurgical unit of the same institution with clinical and radiological features of CSOM, BRS, and ICS were prospectively studied over a 5-year period. Patients were followed up for a minimum of 3 months.
Results:
Two thousand, two hundred and seventy-nine patients presented during the 5-year study period. Of all these patients, 1511 had CSOM (66.3%) and 768 (33.7%) presented with features of BRS. Eleven (0.73%) had ICS complicating their CSOM while 8 (1.04%) cases of surgically treated ICS followed BRS. Bacterial rhinosinusitis was not more likely to lead to ICS (P = 0.4348). The Odds ratio (OR) of a child ≤ 18 years of age with CSOM developing ICS was 5.24 (95% Confidence interval 1.13-24.34; P = 0.0345), while it was 7.60 (95% Confidence interval 1.52-37.97; P = 0.0134) for children with BRS.
Conclusions:
The most common type of ICS complicating CSOM and BRS was brain abscess and subdural empyema, respectively. Children are more prone to develop surgical ICS following CSOM and BRS. The proportion of males that had ICS was higher in both CSOM and BRS patients. Optimal outcome is achieved in patients that presented with GCS of 13 and above.
Keywords
Bacterial rhinosinusitis
brain abscess
chronic suppurative otitis media
epidural abscess
subdural empyemas
Introduction
Intracranial suppuration (ICS) following chronic suppurative otitis media (CSOM) and bacterial rhinosinusitis (BRS) are generally rare in the age of antibiotics and in the developed world; but when they occur they are potentially lethal.[1] It is associated with a mortality of about 5% in the antibiotic era as compared to 35% in pre-antibiotic period.[2]
CSOM which can affect all age groups is one of the most common childhood infectious diseases worldwide.[3] It is relatively uncommon in the developed world, with a prevalence of less than 1% in the United States of America.[4] In developing countries, the prevalence of CSOM is relatively high with most disease occurring in rural areas.[56] In developing countries a prevalence ranging from 6% to 46% in different populations has been reported.[789] One notion regarding the higher prevalence in developing countries is that the cost of treatment is prohibitive. In a Nigerian study, the cost of CSOM treatment per patient per year amounted to more than the national monthly minimum wage.[10] Public education and awareness in developing countries is low. This is depicted in a Bangladesh study of 203 mothers of children with CSOM living in two slums.[11]
The intracranial complication of BRS includes meningitis, encephalitis, cavernous or sagittal sinus thrombosis and ICS (epidural abscess, subdural empyema and intraparenchymal abscesses). In children, presentation with complications are said to be associated with socioeconomic incongruences.[12]
Adverse cultural beliefs and practices, disease awareness, low socioeconomic status, poor access to healthcare, inadequate or inappropriate treatment and sometimes late hospital presentation are prevailing factors in 3rd world countries. In the light of this, patients with CSOM and BRS may be more prevalent, likewise its associated complications which may include ICS.
The objective of this study was to know the frequency of BRS and CSOM and relate it to its rare complication of ICS while also describing the demography, type and outcome of surgically treated ICS that resulted from BRS and CSOM.
Materials and Methods
All patients with CSOM and BRS, and ICS which necessitated neurosurgical evacuation following CSOM and BRS at the Otorhinolaryngological department and the Neurosurgical unit of the Lagos State University Teaching Hospital (LASUTH), Ikeja, Lagos, Nigeria, were studied prospectively and consecutively after an informed patient consent. The institution is a 750-bed tropical tertiary hospital which is one of the two tertiary referral centres for Neurosurgical and otorhinolaryngological conditions in the country's most populated state, Lagos state. The state is a conurbation of cities. The study period was done over a 5-year period (between January 2009 and December 2013). Patients that discharged themselves against medical advice or died while awaiting confirmatory tests were excluded from the study.
In accordance with our canon, all patients in whom there was a clinical suspicion of ICS had a brain computed tomography (CT) scan or magnetic resonance imaging (MRI) done on admission. Other tests done included full blood count, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), pus microscopy (Gram stain, India ink, and acid-fast bacilli staining), culture and sensitivity, and blood culture. Apart from the clinical condition of the patient, the ESR, CRP levels and the temperature chart were used to determine the duration of antibiotic treatment and the need for repeat surgical evacuation of abscess. As a general principle, antibiotic therapy was continued for a minimum of 4 weeks after the abscess is drained and for longer periods until the C-reactive protein and or ESR is normal. A multidisciplinary approach was ensured in all the surgical patients. The outcome of surgical management was assessed 3months after surgery using the 5-scale Glasgow outcome score (GOS), where 1-dead, 2-persistent vegetative state (patient exhibits no obvious cortical function), 3-severe disability (conscious but disabled and dependent), 4-moderate disability (disabled but independent as far as daily life is concerned), 5-good recovery (resumption of normal activities even though there may be minor neurological or psychological deficits).
The following data were collected and recorded electronically: age (children classified as ≤18 years) and gender, clinical history, level of consciousness on admission using the Glasgow Coma Scale (GCS), and Glasgow outcome score. Patients were also grouped according to their ages and with respect to the etiology of ICS. We compared groups using Chi-square, Fisher's exact test, and t-test as appropriate. The Odds Ratio (OR) was used to compare risks and probability of getting ICS. Significance was judged at P < 0.05 level. The data werecomputed and analyzed using the Statistical Package for Social Sciences version 17 statistical software (SPSS Inc., Chicago, IL, USA). The study followed principles in the Declaration of Helsinki.
Results
Two thousand, two hundred and seventy-nine patients presented during the 5-year study period. Of all these patients, 1511 had CSOM (66.3%) and 768 (33.7%) presented with features of BRS. The male to female ratio was 1.1:1 for CSOM and 1:1.3 for BRS [Table 1]. Nineteen patients had surgical ICS, 11 (0.73%) of which followed CSOM complication and 8 (1.04%) secondary to BRS. Statistically, BRS was not more likely to lead to ICS when compared to CSOM (P = 0.4348).

Though almost equal frequency of males and females presented with CSOM, more males significantly had ICS complicating their disease compared to females (P = 0.0000). Similarly, the proportion of males that had ICS following BRS were significantly higher than their female counterparts (P = 0.0000), despite fewer males presenting with BRS [Figures 1 and 2]. The OR of a male patient with BRS developing ICS is 3.85 (95% Confidence interval 0.77-19.18; P = 0.1003) compared to a female patient with OR of 0.26 (95% Confidence interval 0.05-1.30). In CSOM cases, for the male patient developing ICS, the OR is 2.51 (95% Confidence interval 0.66-9.49; P = 0.1757), compared to 0.40 for females (95% Confidence interval 0.11-1.51).
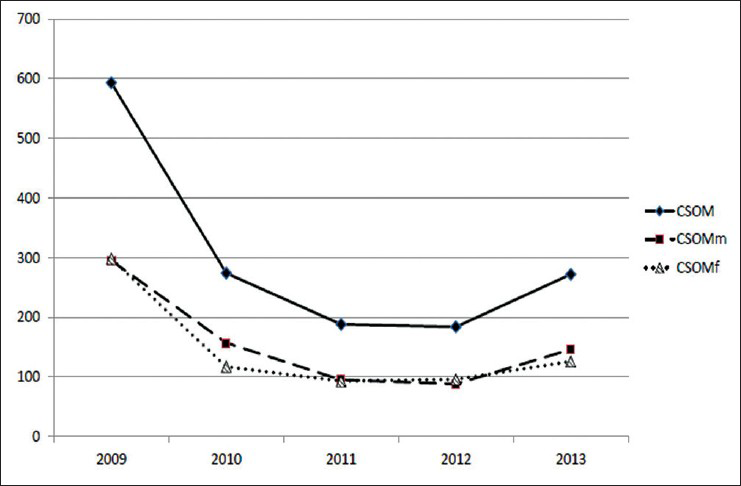
- Gender comparison in patients with chronic suppurative otitis media (CSOM). *CSOMm-Chronic suppurative otitis media, males, **CSOMf-Chronic suppurative otitis media, females
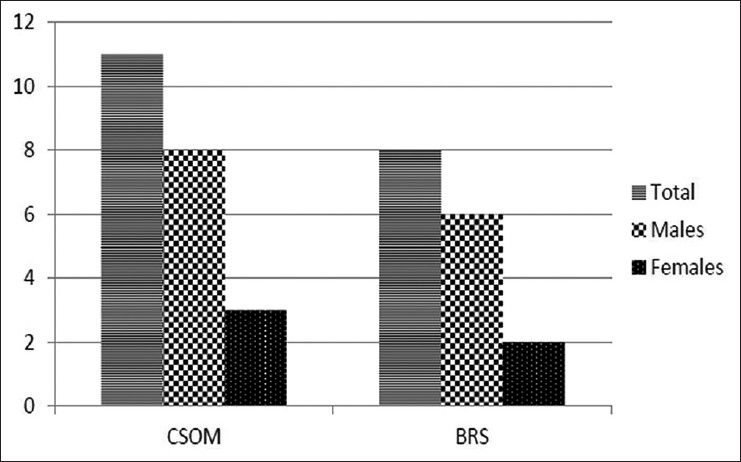
- Frequency of patients with surgical intracranial suppuration following chronic suppurative otitis media (CSOM) and bacterial rhinosinusitis (BRS) with respect to gender
About 50% of the patients with CSOM were children (≤18 years) while 28.8% of the children had BRS [Table 1]. ICS was more common in children (15 out of 19 cases). Nine out of 11 patients with CSOM were ≤18 years. The proportion of patients who were ≤18 years that had ICS from CSOM were significantly higher (P = 0.0000) compared to those above 18 years of age, though no difference in presentation based on age group in all patients with CSOM. However, in the BRS group, 6 patients were ≤ 18 years out of the 8 patients with ICS. The OR of a patient ≤ 18 years of age with CSOM developing ICS is 5.24 (95% Confidence interval 1.13-24.34; P = 0.0345) compared to those older with OR of 0.19 (95% Confidence interval 0.04-0.89). For BRS, the OR for ≤18 years patient developing ICS was 7.60 (95% Confidence interval 1.52-37.97; P = 0.0134), compared to 0.13 (95% Confidence interval 0.03-0.66) for patients more than 18 years of age.
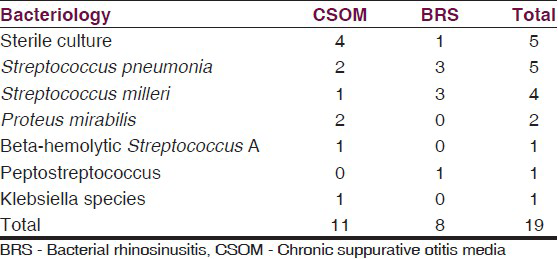
In the patients with ICS, the admission GCS score was 13-15 in 13 patients, 9-12 in 4 and 3-8 in 2 patients. Eleven and sevenpatients had brain abscess and subdural empyema, respectively [Table 1 and Figure 3]. Bacterial organisms were isolated in 14 samples (73.7%) [Table 2]. Seventeen patients had good recovery outcome while twopatients died, giving a mortality rate of 10.5%. One of the dead patients had subperiostal abscess with osteomyelitis complicated with subdural empyema while the other had brain abscess, both presenting with an admission GCS 5 and 6, respectively.
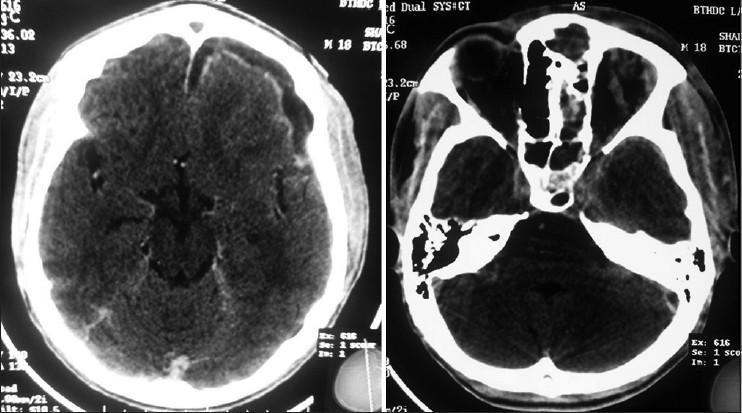
- Brain and bone window of cranial tomographic scan of a patient with ethmoidal sinusitis and subdural empyema
Discussion
Children are prone to developing upper respiratory tract infections, which often result in bacterial complications such as CSOM and BRS. Both are two of the most common bacterial complications of upper respiratory tract infections in children.
The prevalence of CSOM and BRS varies in different countries. In this study we noted a higher frequency of CSOM when compared to BRS (2:1). In a study from the Netherlands, the yearly incidence of CSOM was estimated to be 39 cases per 100,000 in children and adolescents aged 15 years and younger.[13] In Indonesia, the prevalence of CSOM is relatively high with most disease occurring in rural areas; of the 7005 children studied, 116 (1.7%) had CSOM.[5] The rates per 1000 of CSOM in rural Bali and Bandung were significantly higher (75 and 25, respectively) than in the rest of Indonesia (P < 0.05). In rural Bali the rate per 1000 children of inactive CSOM was 63 in 6-9 year olds, compared with 37 in children aged 13-15 years.[5] Most studies have found that males and females are equally affected, although some have found a male predominance.[141516] In our study, though male preponderance was noted, this was slight [Table 1]. Also of note in this study is that the frequency of CSOM in children and adult was almost equal, but BRS was more in adults.
In the present era of antibiotics, complications from CSOM and BRS are rarely seen because of early antibiotic intervention. CSOM without prompt, proper treatment can progress to a variety of mild to life-threatening complications that can be separated into twosubgroups: Intratemporal and intracranial.[17]
ICS generally results from direct spread from contiguous structures, retrograde thrombophlebitis, penetrating head trauma, following cranial surgery, haematological spread (suppurative lung diseases, cyanotic heart diseases) and sometimes cryptogenic.[181920] The spread from contiguous structures emanates from infected sinuses (mastoid, ethmoid, sphenoid, and frontal sinusitis), CSOM, orbital cellulitis, sagittal sinus phlebitis, and cranial osteomyelitis.[3212223] For CSOM, the mechanism of infection of the middle ear cleft is postulated to be translocation of bacteria from the external auditory canal through a perforation into the middle ear. Some authors suggest that the pathogenic organisms may enter through reflux of the eustachian tube. Brain abscesses occur as the infection spreads through the tegmen tympani or mastoideum to the temporal lobe or the cerebellum. Their presentation may be indolent, as this disease initially grows in “silent” areas of the brain. When these complications occur they are best treated early and aggressively- imaging, neurosurgical drainage, and antibiotic therapy.[24]
The complications that follow BRS include toxic shock syndrome, chemosis, orbital cellulitis, proptosis, ophthalmoplegia, orbital abscess, subperiosteal abscess, and intracranial complications. Sedaghatet al. noted 0.7% of children 18 years of age or younger diagnosed with BRS had orbital or intracranial complications.[12] Such complications were more common in boys (odds ratio [OR]: 1.65, P < .001) and children with chronic rhinosinusitis (OR: 7.89, P < .001) and intracranial complications were associated with Medicaid (OR: 2.96, P < .001) or no insurance at all (OR: 3.73, P = .001).This is similar to our study where we noted that males were significantly more affected than females; the OR of a male patient with BRS developing ICS is 3.85. Piatt also noted that boys were affected much more commonly than girls and black children were affected out of proportion to their presence in the population, with the overall incidence seemed to peak in early adolescence.[25]
In conclusion, the most common type of ICS complicating CSOM and BRS was brain abscess and subdural empyema, respectively. The proportion of males that had surgically treated ICS was higher in both CSOM and BRS patients. Patients that are ≤ 18 years of age are more prone to develop surgically treated ICS following CSOM and BRS. Optimal outcome is achieved in patients that present with GCS of 13 and above following urgent neurosurgical drainage and antibiotic therapy. Efforts at early diagnosis and treatment should target providers of care at primary and secondary centers. Such interventions will improve outcomes of patients with surgically treated ICS following BRS and CSOM complications.
All authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Chronic suppurative otitis media: A review. Int J PediatrOtorhinolaryngol. 2006;70:1-12.
- [Google Scholar]
- Epidemiology and pathogenesis of chronic suppurative otitis media: Implications for prevention and treatment. Int J PediatrOtorhinolaryngol. 1998;42:207-23.
- [Google Scholar]
- Otitis media in Indonesian urban and rural school children. Pediatr Infect Dis J 2014 Epub ahead of print
- [Google Scholar]
- Comparison of chronic suppurative otitis media in rural and urban primary school children in Bangladesh. J LaryngolOtol. 2014;128:499-503.
- [Google Scholar]
- Chronic suppurative otitis media in a birth cohort of children in Greenland: Population-based study of incidence and risk factors. Pediatr Infect Dis J. 2011;30:25-9.
- [Google Scholar]
- Chronic suppurative otitis media in a children's hospital in Addis Ababa, Ethiopia. Ethiop Med J. 1999;37:237-46.
- [Google Scholar]
- Chronic suppurative otitis media: Prevalence and practices among rural South Indian children. Int J PediatrOtorhinolaryngol. 1999;48:217-21.
- [Google Scholar]
- Chronic suppurative otitis media: Socio-economic implications in a tertiary hospital in Northern Nigeria. Pan Afr Med J. 2010;4:3.
- [Google Scholar]
- Prevalence of chronic suppurative otitis media among the children living in two selected slums of Dhaka City. Bangladesh Med Res Counc Bull. 2004;30:95-104.
- [Google Scholar]
- Socioeconomic disparities in the presentation of acute bacterial sinusitis complications in children. Laryngoscope. 2014;124:1700-6.
- [Google Scholar]
- Predictors of chronic suppurative otitis media in children. Arch Otolaryngol Head Neck Surg. 2006;132:1115-8.
- [Google Scholar]
- Chronic suppurative otitis media in the Solomon Islands: A prospective, microbiological, audiometric and therapeutic survey. N Z Med J. 1986;99:812-5.
- [Google Scholar]
- Clinico-epidemiological profile of chronic suppurative otitis media patients attending a tertiary care hospital. J Indian Med Assoc. 2011;109:324-6.
- [Google Scholar]
- Chronic suppurative otitis media in Sudanese patients. East Afr Med J. 1990;67:4-8.
- [Google Scholar]
- Complications of chronic otitis media and cholesteatoma. OtolaryngolClin North Am. 2006;39:1237-55.
- [Google Scholar]
- Otogenic cerebral abscess: An unusual complication of otitis media. Ear Nose Throat J. 2011;90:E11-2.
- [Google Scholar]
- Microbiology of chronic suppurative otitis media. Ann OtolRhinolLaryngol. 1988;97:9-10.
- [Google Scholar]
- Intracranial suppuration: A modern decade of postoperative subdural empyema and epidural abscess. Neurosurgery. 1994;34:974-81.
- [Google Scholar]
- Surgical treatment of brain abscess and subdural empyema. J Neurosurg. 1973;38:198-203.
- [Google Scholar]
- Pediatricotogenic intracranial abscesses. Otolaryngol Head Neck Surg. 2010;142:434-7.
- [Google Scholar]
- Intracranial suppuration complicating sinusitis among children: An epidemiological and clinical study. J NeurosurgPediatr. 2011;7:567-74.
- [Google Scholar]






