Translate this page into:
Current Profile of Physical Impairments in Children with Cerebral Palsy in Inclusive Education Settings: A Cross-Sectional Study
Suresh Mani, PT, PhD Department of Physiotherapy, Lovely Professional University Phagwara, Punjab 144401 India suresh.22315@lpu.co.in vemsuresh@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Introduction Cerebral palsy (CP) excerpts a heterogeneous corral of neurological disorders occurring due to injury to the developing brain leading to motor dysfunctions. The CP children enjoy success and progress in normal school education and curriculum program. The principle of inclusive education has been acknowledged over recent decades in all countries supporting the schooling of children with disabilities into mainstream settings for constructing an inclusive society.
Objective The objective of this study was to determine the current status of physical impairments in children with CP in inclusive education settings in district Mandi, Himachal Pradesh.
Materials and Methods A survey using the physical examination of all CP children (n = 20) between the age group of 6 and 12 years in inclusive education settings with an organized interview of special educators in school settings was conducted. Descriptive analysis was conducted by using SPSS IBM 22.
Results A total of 20 CP children (11 boys and 9 girls, with the mean age of 9.8 ± 1.69) were enrolled in the study. Mean and standard deviation of Visual Analog Scale (6.5 ± 0.82), Pediatric Balance Scale (21.4 ± 17.1), Gross Motor Function Classification System, Expanded and Revised (2.8 ± 1.46), Manual Ability Classification System (2.5 ± 1.1), Gross Motor Function Measurement-88 (36.40 ± 22.94), and Goal Attainment Scale (35.9 ± 0.40) with the total WeeFIM score (75.7 ± 3.4) were analyzed as the score of all outcome measures.
Conclusion Right to Education act promotes the compulsory education of such children, and limiting disability by knowing the current profile of impairments could help in improving physical and functional status in children.
Keywords
therapy programs
neurological disorders
inclusive education
cerebral palsy
rehabilitation
ICF core sets
spastic
non-progressive motor disorder
topographical
Introduction
Cerebral palsy (CP) is a familiar neurodevelopmental malady in kids with the incidence of 2 to 2.5 per 1,000 live births globally.1 Societal affairs in particular gender-specific disparity, family nurturance, and socio-economical dignity affect treatment revealing a relationship between the socio-demographic profiles of families belonging to CP patients.2 An Indian study conducted at Rajasthan endowed that CP is the prime cause of disability in developing countries like India.3 These children with CP, in such ambience, confront economical, topographical, as well as communal hurdles in retrieving medical or rehabilitation interventions.4 CP is a non-progressive motor disorder associated with poor perception, cognition, and related musculoskeletal problems like sitting, standing, and walking.5 Impairments in such children can be of spastic, athetoid, and ataxic types which could be due to injury in different parts of brain. The child can be hemiplegic, diplegic, or quadriplegic based on the number of limbs involved.6
The fundamental of comprehensive inclusive education has been progressively recognized in the last 10 years, and virtually all countries promote the mainstreaming of children with disabilities because it is the most effective way of creating an inclusive society and ensuring that all children receive education.1 7 8 In educational settings, physical demands and needs of children can be fulfilled by providing regular therapy programs in least restrictive barrier-free environment.9 10 The therapists work within the groups or separately with a child including the teacher and parents who may be advised and explained treatment techniques.11 12 The children with CP show their potential in a more commendable school environment and achieve academic success in a traditional school setting and enjoy success in normal school education and curriculum.13 14 The appropriate schooling option for a child with CP is determined by the existence and severity of physical disabilities, as well as the available facilities in the area for schooling.15 Providing the rehabilitation services in inclusive education settings would require information on the physical status of CP children along with demographic profile and such information would contribute to delineate the magnitude of the problem. The population-based data of CP are very limited, and no such clinical registry system of disease has been observed in India. Keeping this in mind, the present study is an effort and has been planned to explore the physical profiles of CP children in district Mandi of Himachal Pradesh (HP), India. Mandi district is a major town and municipal corporation in the Indian state of HP, located 145 km (90 mi) to the north of the state capital Shimla in the northwestern Himalayas at an average altitude of 880, 31°72′N latitude, and 76° 92′E longitude with the temperature typically ranging from 6.7°C (44.06°F) to 39.6°C (103.28°F) over the course of year. District Mandi is home to many educational institutions offering the basic education of primary, secondary, and higher educational system, along with small-scale woolen and hotel industries which are the backbone of the district.
The objective of this study was to determine the current status of physical impairments in children with CP in the inclusive education system in district Mandi, HP, India.
Materials and Methods
This was a descriptive kind of study performed by obtaining preliminary data from Unified-District Information System For Education statistics from the District Institution of Education and Training (DIET), Mandi, HP, regarding CP children.16 A purposive sampling method was used for data collection.
Formal written consent was obtained from the concerned authority of DIET, Mandi. These children were selected through survey from those already screened out by the special educators based on disability certificate. After explaining the objectives, purpose and the method of study, subject's and parent's informed consents were obtained.
-
Clinical assessment and examination: After making appointments with special educators, each student was assessed and examined individually based on standardized tests.
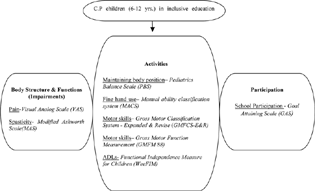
Organized interview with parents and special educators: Detailed questionnaire including demographic data was filled by the investigator with the help of the class special educators and parents. The initial draft of the questionnaire was prepared after a literature review, and in-depth interviews from special educators and parents were validated for contents by experts. The ICF core sets are based on the International Classification of Functioning, Disability, and Health (ICF). The ICF core sets based on the ICF-Children and Youth model, with eight categories monitoring physical impairments in school-aged CP children between 6 and 12 years of age, were considered as outcome measures as shown in Fig. 1 for study.17
-
Fig. 1 Flowchart revealing outcome measures using the ICF Model in CP. ICF, International Classification of Functioning, Disability, and Health.
Fig. 1 Flowchart revealing outcome measures using the ICF Model in CP. ICF, International Classification of Functioning, Disability, and Health.
Inclusion Criteria
Inclusion criteria were as follows.
-
CP students of all types and both sex (6–12 years) diagnosed with minimum 40% on disability certificates by pediatrician /neurologist,
-
CP children with mild mental retardation (intelligence quotient level 50–70%),18
-
classified with all grades of Gross Motor Function Classification System—Expanded and Revised (GMFCS-E&R) for CP children,19
-
CP students of primary and middle classes of all sections in government schools of district Mandi, HP, and
-
subjects and their parents/guardians giving consent to participate in study.
Exclusion Criteria
Exclusion criteria were as follows.
-
CP children of secondary and senior secondary classes,
-
children with developmental delay, down syndrome, autism and epilepsy, or undergone surgery or having Botox injections within 6 months before therapy, and
-
CP with hearing and visual impairments and moderate and severe/profound mental retardation.
Results
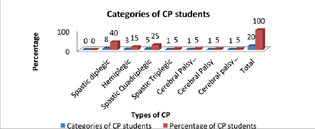
Descriptive statistics analysis of CP characteristics was performed using SPSS 22 (IBM Corp. United States). In the present study, 11 males (55%) and nine females (45%) with CP in the inclusive school settings of district Mandi, HP, were included. The study included CP children with an average age of 9.8 ± 1.69 years. Most of the cases (80%) were from the lower economic class with the annual income of 1,343.20 US $/year, indicating that the poor socioeconomic status of parents is greatly associated with CP. Most of the CP cases (55%) were term delivery by doctors with different complications. The risk of CP among term infants may be relatively low, but most children with CP are the product of term deliveries. Of all, 25% CP cases were wheelchair bound, 20% were using rollators, 10% were using CP chair and crutches, and 35% cases were not using any mobility aids. The distribution of CP according to various age groups revealed single child (5%) in the age group of 6 to 7 years, two children (10%) in 8 years age group, three children (15%) in 9 years age group, six children (30%) in 10 years age group, three children (15%) in 11 years age group, and four children (20%) in 12 years age group. Spastic diplegic CP was most common (40%), followed by spastic quadriplegic (25%), hemiplegic (15%), and triplegic and paraplegic with the percentage of 5% each as shown in Fig. 2. No cases of ataxic, athetoid, and mixed kinds were noticed as the sample was small in inclusive settings of a particular age group.
-
Fig. 2 Categorical percentage of CP children. CP, cerebral palsy.
Fig. 2 Categorical percentage of CP children. CP, cerebral palsy.
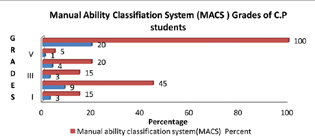
Among all 20 children, fine motor abilities were assessed with MACS showing 15% children with grade I, 45% with grade II, 15% with grade III, 20% with grade IV, and 5% with grade V of MACS level as in Fig. 3.
-
Fig. 3 CP children with MACS grades. CP, cerebral palsy; MACS, Manual Ability Classification System.
Fig. 3 CP children with MACS grades. CP, cerebral palsy; MACS, Manual Ability Classification System.
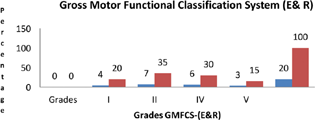
In Fig. 4, 35% of children were noticed with grade II, 30% with grade IV, 20% with grade I, no child with grade III, and 15% with grade IV of GMFCS-E&R.
-
Fig. 4 CP children with GMFCS-E&R grades. CP, cerebral palsy; GMFCS-E&R, Gross Motor Function Classification System—Expanded & Revised.
Fig. 4 CP children with GMFCS-E&R grades. CP, cerebral palsy; GMFCS-E&R, Gross Motor Function Classification System—Expanded & Revised.
Table 1 reveals the score of various associated domains of CP as the means/standard deviation of VAS (6.5 ± 0.82), PBS (21.4 ± 17.1), GMFCS-E&R (2.8 ± 1.46), MACS (2.5 ± 1.1), GMFM-88 (56.40 ± 22.94), GAS (35.9 ± 0.40), and total WeeFIM score (75.7 ± 3.4).
|
S. no. |
Domains of physical impairments (CP) |
Mean |
Standard error |
SD |
|---|---|---|---|---|
|
1 |
VAS |
6.5 |
0.18496 |
0.82717 |
|
2 |
PBS |
21.4 |
3.83365 |
17.14459 |
|
3 |
GMFCS-E&R |
2.85 |
0.32667 |
1.46089 |
|
4 |
MACS |
2.55 |
0.25624 |
1.14593 |
|
5 |
GMFM-88 |
56.404 |
5.13153 |
22.94888 |
|
6 |
GAS |
35.99 |
0.09058 |
0.4051 |
|
7 |
WeeFIM sphincter control |
10.45 |
1.53978 |
6.8861 |
|
8 |
WeeFIM transfers |
11.45 |
1.55 |
6.93181 |
|
9 |
WeeFIM locomotion |
7.3 |
0.96818 |
4.32982 |
|
10 |
WeeFIM communication |
10.75 |
0.62355 |
2.7886 |
|
11 |
WeeFIM self-care |
20.5 |
2.06665 |
9.24235 |
|
12 |
WeeFIM social cognition |
15.25 |
0.98375 |
4.39946 |
|
13 |
WeeFIM total score |
75.7 |
7.03604 |
31.46611 |
Abbreviations: CP, cerebral palsy; GAS, Goal Attainment Scale; GMFCS-E&R, Gross Motor Function Classification System—Expanded & Revised; GMFM, Gross Motor Function Measurement-88; MACS, Manual Ability Classification System; PBS, Pediatric Balance Scale; SD, standard deviation; VAS, Visual Analog Scale.
Table 2 reveals the percentages of the sub-parameters such as body structures (s), body functions (b), activities and participation (d) included in the core set used in this study. The ICF encompasses qualifiers to enumerate the level of functioning or ferocity of problems in various ICF categories designated as: 0 = no problem; 1 = mild problem; 2 = moderate problem; 3 = severe problem; 4 = complete problem, 8 = not specified, and 9 = not applicable.
|
Structures and function |
ICF category sub-parameters |
ICF codes |
0 |
1 |
2 |
3 |
4 |
8 |
9 |
|---|---|---|---|---|---|---|---|---|---|
|
Structure brain |
s 110 |
– |
– |
– |
– |
– |
– |
– |
|
|
Body functions |
Sensation of pain |
b 280 |
14(70%) |
3(15%) |
3(15%) |
0 |
0 |
0 |
0 |
|
Muscle tone function |
b 735 |
0 |
15(75%) |
3(15%) |
2(10%) |
0 |
0 |
0 |
|
|
Control of voluntary movement functions |
b760 |
0 |
7(35%) |
11(55%) |
2(10%) |
0 |
0 |
0 |
|
|
Activities |
Maintaining a body position |
d 415 |
0 |
5(25%) |
7(35%) |
8(40%) |
0 |
0 |
0 |
|
Walking |
d 450 |
0 |
5(25%) |
8(40%) |
7(35%) |
0 |
0 |
0 |
|
|
Toileting |
d 530 |
3(15%) |
2(10%) |
11(55%) |
4(20%) |
0 |
0 |
0 |
|
|
Eating |
d 550 |
4(20%) |
11(55%) |
4(20%) |
1(5%) |
0 |
0 |
0 |
|
|
Fine hand use |
d 440 |
2(10%) |
10(50%) |
7(35%) |
1(5%) |
0 |
0 |
0 |
|
|
Participation |
School education and participation |
d 820 |
0 |
11(55%) |
8(40%) |
0 |
1(5%) |
0 |
0 |
Abbreviation: ICF, International Classification of Functioning, Disability, and Health.
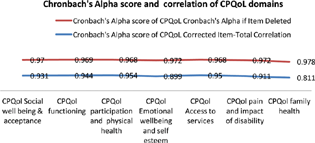
Fig. 5 shows the overall scale mean and Cronbach's α score of all subscales of the quality of life of CP children. For internal consistency and reliability, Cronbach's α score of >0.7 is regarded as good. A value of >0.7 for Cronbach's α is considered good for internal consistency and reliability. In all domains of cerebral palsy: quality of life (CPQol), Cronbach's α revealed a good correlation between the values >0.7 indicating good quality in subscales of CP.
-
Fig. 5 Cronbach's alpha score and the correlation of CPQoL (cerebral palsy: quality of life) domains.
Fig. 5 Cronbach's alpha score and the correlation of CPQoL (cerebral palsy: quality of life) domains.
Discussion
This descriptive study in inclusive education settings of CP children between 6 and 12 years in Mandi district of HP provides the data of the current profile of physical impairments of CP children. Most of the cases, i.e., 80% cases of CP were from lower economic class with an annual income of 1 lac/annum indicating that poor socioeconomic status of parents is greatly associated with CP, as a study done by Forthun et al (2018) supports that a lower incidence of CP is associated with a higher level of parental educational achievement.20 Most of CP cases (55%) were term delivery conducted by doctors associated with different complications. A study having done by Moster et al (2010) revealed that the risk of CP among term infants may be relatively low but most children with CP are the product of term deliveries.21 In this study, male to female percentage was 55% male and 45% female CP children which is in accordance with previous studies revealing that CP is the common problem in boys than girls.22 The spastic type of CP was the most common in all topographical categories which is in accordance with other studies.23 However, no cases of monoplegic, ataxic, and athetoid or mixed CP were seen in medical certificates of children. This disparity can be observed due to a limited sample found in school settings in district Mandi. This shows the geographical condition of HP, poor profile of parents in terms of economic status, and rural population unaware of medical and educational facilities available in district Mandi, HP, despite being a large district of the state.24 The quality of life of CP children is very much associated with gross and fine motor skills. The present study revealed all domains of CPQol by Cronbach's α score depicting a good correlation between subscales of CP. A similar study conducted by Das et al (2017) showed that motor function does not affect the quality of life of CP children but it varies with age and education supporting the present study results in CPQol.25
A significant dilemma that must be dealt with is regarding the development of a school environment which promotes participation in inclusive education settings while providing individualized support to students with participation restriction.26 The present study supports the observation of Wood and Rosenbaum in regard to GMFCS which depicts that meaningful distinction in gross motor development helps the therapists in therapeutic planning at the school level. The application of this system in the present cross-sectional study would serve in forming CP clinical registry and effective intervention plan in inclusive education settings.27 28 This clinical profile of CP children in school settings was evaluated as the government of India is pushing every disabled child to be enrolled in school and get education under Right to Education act.29
Because the CP children have the ability to learn, the state education system must provide them with opportunities and the necessary support. The pioneering legislation known as IDEA 1975 (Individuals with Disabilities Education Act) in the United States is a model step in this issue.30
Conclusion
The study highlights the physical profile of CP children in school settings. These physical impairments in this particular age really hamper the academics, and this could be better age for intervention. Therapeutic services in school settings could be a boom to such children in limiting their impairments and disabilities and gaining functional independence.
Acknowledgments
The author would like to thank all the special educators, children with CP, and their parents along with higher authorities of DIET, Mandi, HP.
Conflict of Interest
None declared.
Funding Self-funded by authors.
References
- Aetiology and epidemiology of cerebral palsy. Paediatr Child Heal. 2016;26(9):367-372.
- [Google Scholar]
- Socio-demographic profile of cerebral palsy affected patients: an Indian scenario. J Curr Res Rev. 2015;7:15-18.
- [Google Scholar]
- A clinico-epidemiological study of cerebral palsy in western Rajasthan. Int J Contemp Pediatr. 2017;4:1146-1152.
- [Google Scholar]
- Community-based parent-delivered early detection and intervention programme for infants at high risk of cerebral palsy in a low-resource country (Learning through Everyday Activities with Parents (LEAP-CP): protocol for a randomised controlled trial. BMJ Open. 2018;8(6):e021186.
- [Google Scholar]
- Relationship between gross motor function and daily functional skill in children with cerebral palsy. Ann Rehabil Med. 2013;37(1):41-49.
- [Google Scholar]
- Including children with cerebral palsy in mainstream physical education lessons: a case study of student and teacher experiences. Graduate Journal of Sports, Exercise and Physical Education Research. 2012;1:1-15.
- [Google Scholar]
- Determinants of inclusive education of 8-12 year-old children with cerebral palsy in 9 European regions. Res Dev Disabil. 2013;34(1):588-595.
- [Google Scholar]
- Inclusive education and education for all. Int J Res Analyt Rev. 2018;5(3):605-608.
- [Google Scholar]
- Factors influencing postural management for children with cerebral palsy in the special school setting. Disabil Rehabil. 2011;33(2):146-158.
- [Google Scholar]
- Developing an All-School Model for Elementary Integrative Music Learning. Dissertation.Com;. :358.
- [Google Scholar]
- Preventive physiotherapy in schools. Delivered at the XIV Biennial Congress of the Australian Physiotherapy Association, Sydney, August 1975. Aust J Physiother. 1975;21:138-142.
- [Google Scholar]
- The need for physiotherapy support for teachers in inclusive education for the inclusion of learners with physical disabilities in selected schools in Zambia.
- [Google Scholar]
- Bruck I School inclusion of children and adolescents with cerebral palsy: is this possible for all of them in our days? Rev Paul Pediatr. 2011;29(3):314-319.
- [Google Scholar]
- Energy expenditure in adults with cerebral palsy playing Wii Sports. Arch Phys Med Rehabil. 2010;91(10):1577-1581.
- [Google Scholar]
- Coping with cerebral palsy: answers to questions parents often ask. Accessed September 2018 at:
- [Publisher] [Google Scholar]
- Statistical data. Gen Stat Off Vietnam [Internet] Accessed March 2019 at:
- [Publisher] [Google Scholar]
- Appication of ICF-CY brief core set for cerebral palsy on a school age child. Acta fisiatrica. 2016;23(1):46-50.
- [Google Scholar]
- The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva 1992
- [Google Scholar]
- Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39(4):214-223.
- [Google Scholar]
- Parental socioeconomic status and risk of cerebral palsy in the child: evidence from two Nordic population-based cohorts. Int J Epidemiol. 2018;47(4):1298-1306.
- [Google Scholar]
- Sex differences in cerebral palsy on neuromotor outcome: a critical review. Dev Med Child Neurol. 2016;58(8):809-813.
- [Google Scholar]
- Cerebral palsy: a mini review cerebral palsy: a mini review abstract. Ann Saudi Med. 2016;26(2):123-132.
- [Google Scholar]
- Quality of life in Indian children with cerebral palsy using cerebral palsy-quality of life questionnaire. J Pediatr Neurosci. 2017;12(3):251-254.
- [Google Scholar]
- Participation and Disability: A Study of Participation in School for Children and Youth with Disabilities. 2006. Stockholm
- [Google Scholar]
- The gross motor function classification system for cerebral palsy: a study of reliability and stability over time. Dev Med Child Neurol. 2000;42(5):292-296.
- [Google Scholar]
- Validation of a model of gross motor function for children with cerebral palsy. Phys Ther. 2000;80(10):974-985.
- [Google Scholar]
- Impact of an educational program on parental knowledge of cerebral palsy. Indian J Pediatr. 2008;75(9):901-906.
- [Google Scholar]
- The Individuals With Disabilities Education Act (IDEA) for children with special educational needs. Pediatrics. 2015;136(6):e1650-e1662.
- [Google Scholar]






