Translate this page into:
Concurrent Spinal Epidural Tubercular and Pyogenic Abscess of Cervical Spine without Bony Involvement
Address for correspondence: Dr. Batuk Diyora, Department of Neurosurgery, 2nd Floor, L.T.M.G. Hospital, Sion (W), Mumbai - 400 022, Maharashtra, India. E-mail: bddiyora@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Spinal epidural abscess (SEA) presents with vertebral body involvement. SEA is mostly pyogenic in developed countries, but in developing countries, tuberculosis is more common cause. Young female presented with fever, neck, and right upper limb pain for 1 month followed by acute onset weakness in the right upper limb. Magnetic resonance imaging study of cervical spine showed contrast-enhancing lesion in C2–C3 epidural region. Surgery-aided by initiation of antibacterial and antitubercular treatment based on culture and histopathological study of pus helped us to get good clinical outcome. One should always keep in mind possibility of tubercular abscess while treating cases of spinal epidural lesions, though it is rare in the absence of osseous involvement. Pyogenic and tubercular abscess can present concurrently and sending pus for culture and sensitivity is must as it plays important role in identifying dual organisms.
Keywords
Abscess
cervical
concurrent
epidural
isolated
pyogenic
spinal
tuberculosis
INTRODUCTION
Spinal tuberculosis (TB) accounts for 2% of TB cases and 10%–15% cases of extra-pulmonary TB.[1] Spinal TB is the most common form of skeletal TB accounting for almost 50% of skeletal TB cases.[2] Spinal TB is most common in thoracolumbar region whereas cervical spine is involved in 2%–3% cases only.[3] Similarly, cervical spine is infrequently affected in spinal epidural abscess (SEA).[4] Pyogenic organisms cause majority of SEA cases in developed countries, Staphylococcus aureaus being most common.[5] However, in developing countries, spinal TB is a leading cause.[6] Very few cases are reported in literature where both pathology are present concurrently. We are reporting a case which is the first case of concurrent epidural tubercular and pyogenic abscess of the cervical spine without bony involvement.
CASE REPORT
A 30-year-female admitted with complaints of neck and right upper limb pain with fever for 1 month. She had acute-onset right upper limb weakness 1 day before admission. On examination, she was thin built, febrile, and had tachycardia with painful restriction of the neck movements. Neurological examination revealed hypotonia in both upper limbs and hypertonia in both lower limbs. Bilateral upper limb power was Medical Research Council (MRC) grade 3/5 at shoulder, elbow, and wrist joints. Right handgrip was weaker than left. Bilateral upper limb reflexes deep tendon reflexes were hypo while bilateral lower limb reflexes were hyper. Planters were extensor on both sides. She had hypoesthesia over C2–C3 dermatome.
She was nondiabetic and nonimmunocompromised. Her cervical spine X-ray showed loss of cervical lordosis. Chest X-ray did not showed evidence of active or old pulmonary TB. Cervical spine contrast magnetic resonance imaging (MRI) showed 4.6 cm × 1.8 cm × 1.3 cm sized intra spinal anterior epidural collection from C2 to C3 with thick peripheral enhancement [Figure 1a-f]. It was causing significant cord compression with cord displacement toward left and posteroaterally. T2-weighted axial images showed C2–C3 cord hyperintense signal suggestive of spinal cord edema. Computed tomography (CT) of cervical spine was normal [Figure 2a and b].
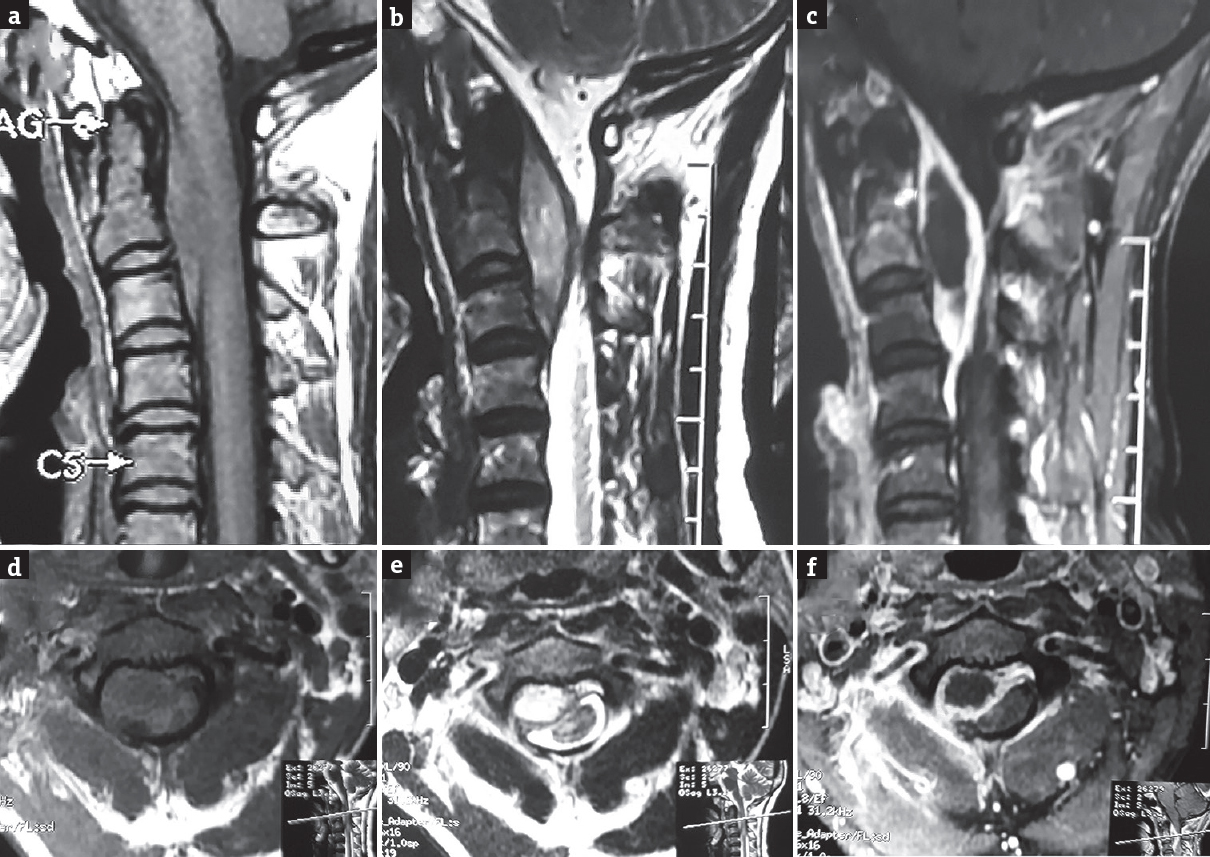
- Magnetic resonance imaging cervical spine sagittal and axial view showing C2–C3 anterior epidural lesion which is isointense on T1-weighted images (sagittal view a, axial view d), hyperintense on T2-weighted images (sagittal view b, axial view e). Lesion showing peripherally contrast enhancement with central hypointensity (sagittal view c, axial view f)
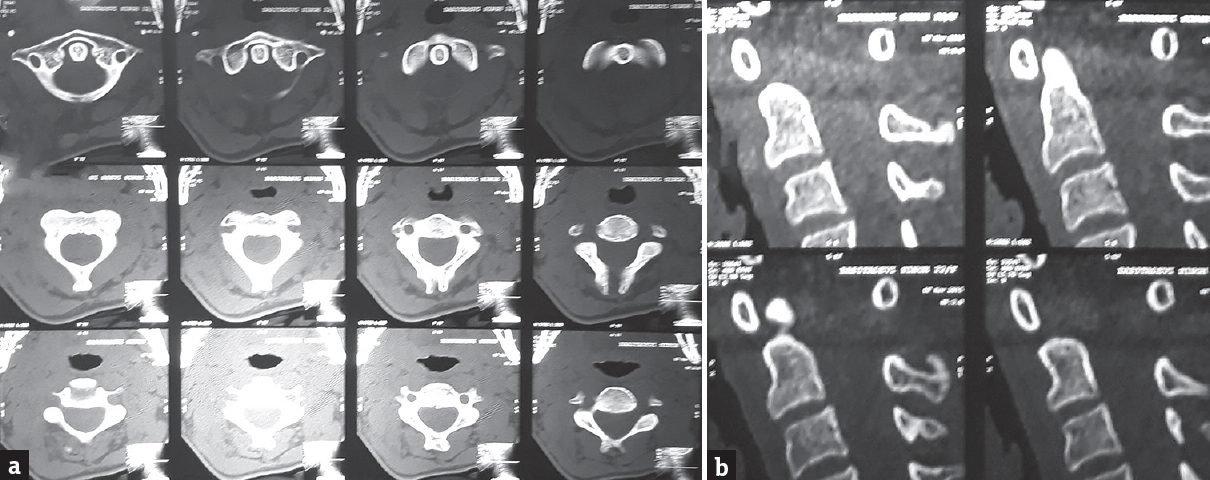
- Computed tomography scan upper cervical spine; axial and sagittal views (a and b) showing no bony abnormality
The patient underwent C2–C3 laminectomy with excision of abscess and its wall. Intraoperatively no osseous abnormality was noted, and the lesion was located in the right anterolateral spinal epidural space. It contained approximately 5 ml of liquefied purulent material. Abscess wall was densely adhered to dura. Acid-fast bacilli staining revealed acid-fast bacilli suggestive of tuberculous etiology. Interestingly, pus culture showed growth of methicillin-resistant Staphylococcus aureaus. Hence, our patient had both tuberculous and pyogenic abscess concurrently. Considering dual organism, we started both anti-microbial and anti-tubercular drugs. Postoperatively, she had significant relief from her neck and upper limb pain. Her right upper limb power improved from MRC grade 3/5 to MRC grade 4/5. Both handgrips strength also increased. Histopathological report suggested fibro-collagenous tissue with moderate lymphoplasmacytic infiltrate and necrosis with few scattered epitheloid such as cells confirming of tuberculous inflammation [Figure 3]. Antimicrobial drugs were continued for 6 weeks and anti-tubercular drugs were continued according to standard protocols. At 6 months clinical follow-up, the patient was asymptomatic with normal power in all four limbs. Follow-up contrast MRI cervical spine at 6 months did not show any signs of residual or recurrent abscess [Figure 4a-f].
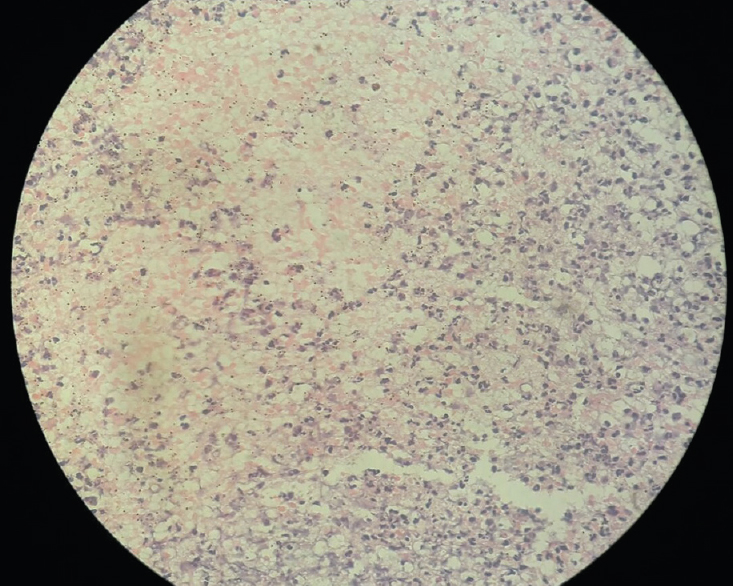
- Histological picture showing evidence of tuberculous inflammation
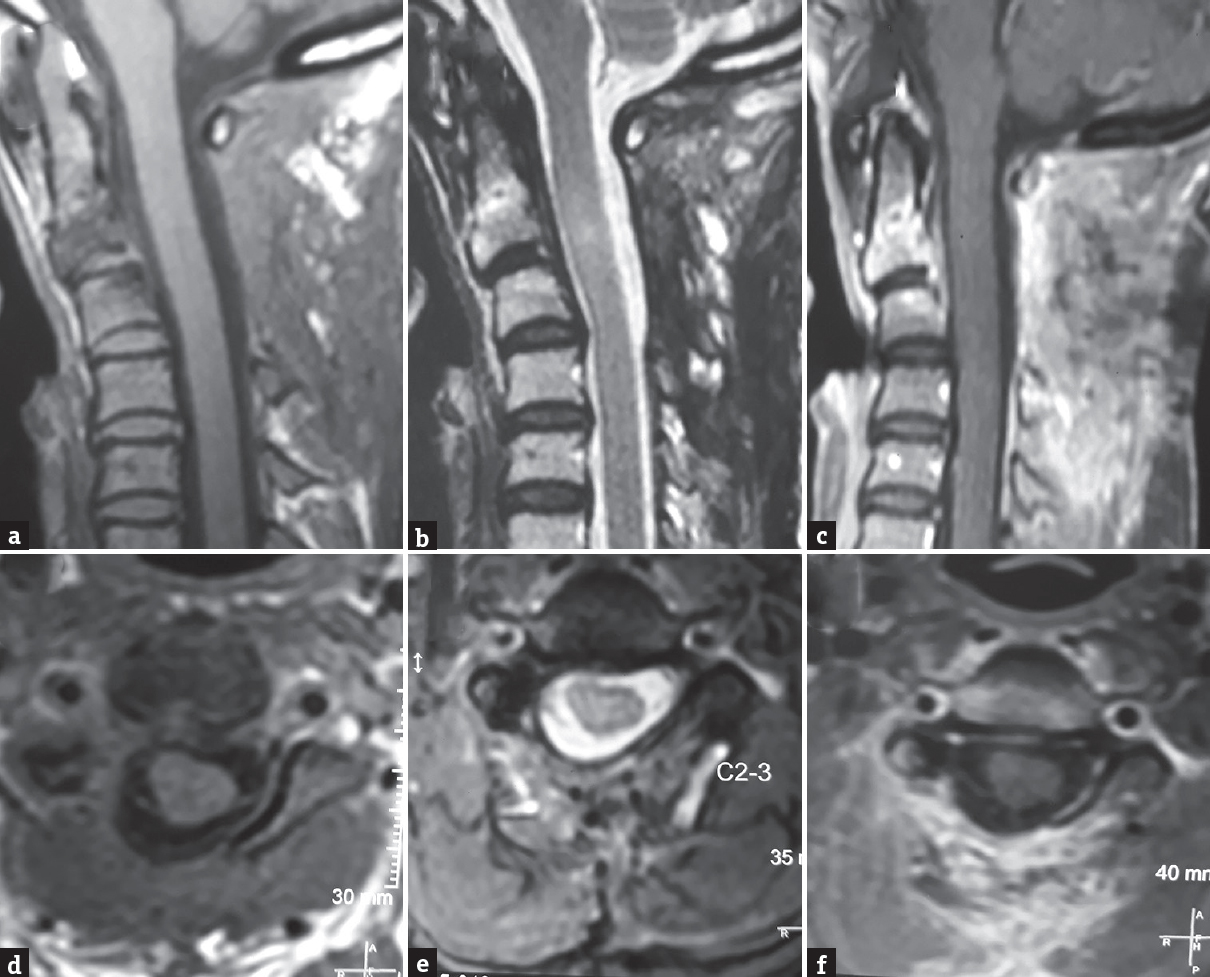
- Postoperative magnetic resonance imaging cervical spine; sagittal, and axial T1 images (a and d), T2 images (b and e) and postcontrast images (c and f) showing no evidence of lesion at C2–C3 level
DISCUSSION
Spinal TB can occur as primary tuberculous lesion or as downward extension of intracranial lesion and finally as a direct extension of vertebral TB which is a more common route.[7] It is usually a result of hematogenous spread of Mycobacterium tuberculosis, with primary lesion either of lungs or genitourinary system.[5] Our case was type II atypical spinal TB according to Babhulakar's classification and Type 1c according to Dastur.[89] Spinal TB involves either thoracic or lumbar regions predominantly and very rarely cervical spine.[10] Constitutional symptoms such as malaise, evening rise in temperature, loss of weight, and appetite are present in approximately 20%–30% of cases of spinal TB. Cervical TB patients present with neck pain, paresthesia and weakness of the upper and lower limbs. Dysphagia, hoarseness of voice, or respiratory distress can also occur due to formation retropharyngeal cold abscess. Our patient had isolated tubercular abscess in anterior epidural space from C2 to C3. Gupta et al. hypothesized that isolated epidural TB can occur due to hematogenous spread.[7] Pyogenic SEA may also present initially with nonspecific symptoms such as fever and localized pain. However, progression of abscess is rapid and is manifested by sensory loss, motor, and sphincter weakness. Concurrent pyogenic and tubercular abscess are reported sparsely in literature, usually it presents with bony involvement.[111213] Table 1 summarizes cases of concurrent spinal epidural tubercular and pyogenic abscess reported in literature.
| Authors | Age (years)/sex | Location | Concurrent infection | Vertebral involvement | Presentation |
|---|---|---|---|---|---|
| Fu et al., 1998[11] | 52/female | C3-C4 | Yes | Yes | Myelopathy |
| Nachimuthu et al., 2000[12] | 30/male | Multicentric TB of cervical, thoracolumbar, sacroiliac regions | Yes | Yes | Neck pain, bilateral upper limb weakness |
| Bhat et al., 2015[13] | 35/male | T11-T12 | Yes | Yes | Resistant psoas abscess |
| Our case | 30/female | C2-C3 | Yes | No | Neck pain, right upper limb weakness |
TB: Tuberculosis
In cases in with unknown primary source of infection, Nachimuthu et al. explained as this could be an early stage of bacterial coinfection.[12] Such bacterial coinfection can reduce response to standard anti-tubercular chemotherapy and lead rapid progression of disease. It can also lead to rapid increase in size of lesion causing acute devastating neurological complication such as quadriplegia or paraplegia. Till now, only three cases of concurrent tubercular and pyogenic spinal TB are reported in literature.[111213] All of these cases had vertebral body involvement and only one case was in cervical region.[11] Our case is probably the first case to be having concurrent tubercular and pyogenic infection of cervical spinal epidural space without vertebral involvement.
MRI and CT imaging of spine are prerequisite before deciding plan of treatment as they provide valuable information about location, the dimension of lesion, and associated bony involvement. Surgical decompression is the treatment of choice in the majority of cases. Neurological improvement is unlikely if the duration of paresis exceeds 24–36 h. Ideal duration of therapy is not well established and generally systemic antibiotics are recommended for 6 weeks in pyogenic SEA.[14] Anti-tubercular chemotherapy remains the mainstay for tubercular abscess. Initial intensive phase consists of four drugs (isoniazid, rifampicin, pyrazinamide and ethambutol), followed by isoniazid and rifampicin in continuation phase. There is controversy regarding optimal duration of chemotherapy. Suggested treatment programs can range from 6 to 18 months.[15] Patients respond well to timely surgical decompression, anti-tubercular drugs and can have good neurological recovery subsequently.
CONCLUSION
We should keep in mind the possibility of tubercular abscess while treating cases of spinal epidural lesions, though it is rare in absence of osseous involvement. Pyogenic and tubercular abscess can present concurrently and sending pus for culture, and sensitivity is must as it plays important role in identifying dual organisms, thus very critical for postsurgical management. Surgical decompression should be done as earliest as possible since these patients respond very well to timely surgical decompression and postoperative antitubercular and antimicrobial drugs.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Tuberculosis of the lower cervical spine (C2 to C7). A report on 40 cases. J Bone Joint Surg Br. 1984;66:1-5.
- [Google Scholar]
- Tuberculous lesions of the lumbosacral region. A 15-year follow-up of patients treated by ambulant chemotherapy. Spine (Phila Pa 1976). 1998;23:1163-7.
- [Google Scholar]
- The clinical presentation and impact of diagnostic delays on emergency department patients with spinal epidural abscess. J Emerg Med. 2004;26:285-91.
- [Google Scholar]
- Postoperative spinal wound infections and postprocedural diskitis. J Spinal Cord Med. 2007;30:441-51.
- [Google Scholar]
- Tuberculosis of the spine. In: Tuli SM, ed. Tuberculosis of the Skeletal System (Bones, Joints, Spine and Bursal Sheaths) (3rd ed). New Delhi: Jaypee Brothers Medical Publishers (P) Ltd; 2004. p. :191-343.
- [Google Scholar]
- A tuberculoma review with some personal experiences. II. Spinal cord and its coverings. Neurol India. 1972;20:127-31.
- [Google Scholar]
- Isolated extradural tuberculous granuloma of the cervical spine: A case report. Eur Spine J. 2012;21(Suppl 4):S467-70.
- [Google Scholar]
- Concomitant tuberculosis and pyogenic infection of the cervical spine. A case report. Spine (Phila Pa 1976). 1998;23:139-43.
- [Google Scholar]
- Multicentric spinal tuberculosis with a possible concomitant bacterial infection. Hosp Physician. 2000;36:61-6.
- [Google Scholar]
- Concomitant pyogenic spondylodiscitis with large psoas abcess in known case of tuberculosis spine presenting as refractory tuberculosis. J Spine. 2015;4:212.
- [Google Scholar]
- Vertebral osteomyelitis in Göteborg, Sweden: A retrospective study of patients during 1990-95. Scand J Infect Dis. 2001;33:527-32.
- [Google Scholar]
- Tuberculosis of the spine: A fresh look at an old disease. J Bone Joint Surg Br. 2010;92:905-13.
- [Google Scholar]






