Translate this page into:
Comparison of Efficacy of Intraoperative Indocyanine Green Videoangiography in Clipping of Anterior Circulation Aneurysms with Postoperative Digital Subtraction Angiography
Address for correspondence: Dr. Anita Jagetia, Department of Neurosurgery, G. B. Pant Institute of Postgraduate Medical Education and Research, 1, J. L. N. Marg, New Delhi - 110 002, India. E-mail: anitajagetia@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
The aim of this study is to assess the efficacy of intraoperative indocyanine green videoangiography (ICG-VA) using postoperative digital subtraction angiography (DSA) in clipped anterior circulation aneurysms.
Materials and Methods:
A prospective study was conducted for 1 year which included thirty patients of anterior circulation aneurysm treated by clipping of aneurysm. Intraoperative ICG-VA was performed on all the patients. Postoperative DSA was performed to assess the efficacy of ICG-VA.
Results:
Intraoperative ICG-VA revealed the occlusion of aneurysm in all the thirty patients. Postoperative DSA revealed aneurysm neck remnant in two patients and demonstrated no branch occlusion.
Conclusions:
Intraoperative ICG-VA is useful in assessing the completeness of clipping of cerebral aneurysms and ensures patency of branch vessels, thus providing a better postoperative outcome. It replaces the need for invasive postoperative angiographic imaging in a selected group of patients and is also cost effective.
Keywords
Digital subtraction angiography
indocyanine green videoangiography
intracranial aneurysm
subarachnoid hemorrhage
INTRODUCTION
The aim of aneurysm surgery is the obliteration of aneurysm with preservation of blood flow in the parent artery, its branches, and perforators[12] Intraoperative or postoperative digital subtraction angiography (DSA) is the most reliable method to evaluate the cerebral blood flow and completeness of the clipping of aneurysm as it provides a three-dimensional (3D) view of any vessel or aneurysm. However, intraoperative indocyanine green videoangiography (ICG-VA) – a noninvasive procedure – also promises to fulfill the said requirement of aneurysm surgery. In some cases, ICG-VA is used as an adjunct in addition to intraoperative or postoperative DSA, and in other cases, it is used as the sole method to confirm the complete obliteration of clipped intracranial aneurysm. The only limitation of ICG-VA is the nonvisibility of vessels which are not in the operative field and can provide false information. Therefore, this study was conducted to assess the effectiveness and reliability of intraoperative ICG-VA in clipping of anterior circulation aneurysm by doing a postoperative DSA.
MATERIALS AND METHODS
This was a prospective study conducted for a period of 1 year (April 2014–April 2015) at a tertiary care hospital. It included 31 aneurysms in 30 patients of either sex undergoing craniotomy and clipping for anterior circulation aneurysms. Intraoperative ICG-VA was performed in all cases during the surgery before and after clip placement following sensitivity test with the ICG dye. It was also performed after clip readjustment. The final ICG-VA images were reviewed after a complete dissection of aneurysm all around. The dose of ICG given was 0.2–0.5 mg/kg through peripheral intravenous access. The angiographic images were assessed intraoperatively on the monitor of a microscope and recorded. All patients underwent postoperative DSA within 1 week of the clipping. The arterial injection of contrast was given manually and the views taken were anteroposterior, lateral, and oblique. The images were studied and if there was any remnant aneurysm, the patient was re-explored and clip was readjusted.
Statistical analysis was performed using a GraphPad Software, Inc., USA for calculating sensitivity, specificity, and P value.
RESULTS
There were 13 (43.3%) females and 17 (56.7%) males ranging from 25 to 70 years (mean, 44.4 years). All the patients presented with subarachnoid hemorrhage and 15 (50%) patients were in Hunt and Hess grade, 6 (20%) in Grade II, 6 (20%) in Grade III, and 3 (10%) in Grade IV. There were a total of 31 aneurysms in 30 patients. Multiple aneurysms were present in 1 patient-one aneurysm at the anterior communicating artery and the other at A1 and A2 junction.
Intraoperative ICG-VA demonstrated complete occlusion of aneurysm in all the thirty patients. Twenty-two (73.3%) patients did not require a clip adjustment after ICG-VA, whereas in 8 (26.6%) patients, clip adjustment was required based on ICG-VA. Of these eight patients, 7 (23.3%) had residual neck and in 1 (3.3%) major vessel was entrapped in the clip. Immediately following clip readjustment, ICG-VA demonstrated complete occlusion of aneurysm and release of entrapped vessel [Table 1]. There were no side effects of the ICG dye observed during this study.
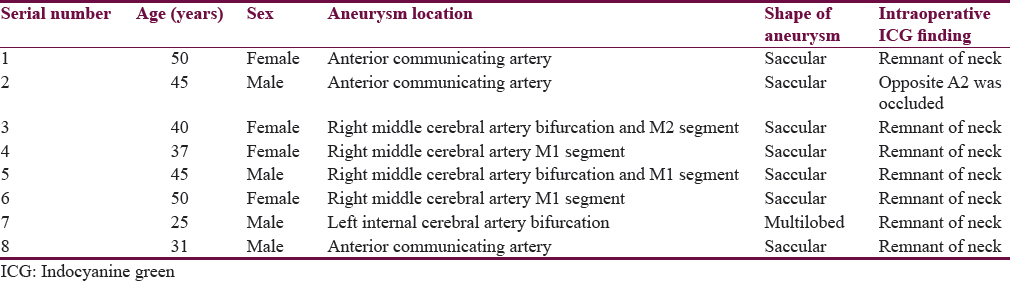
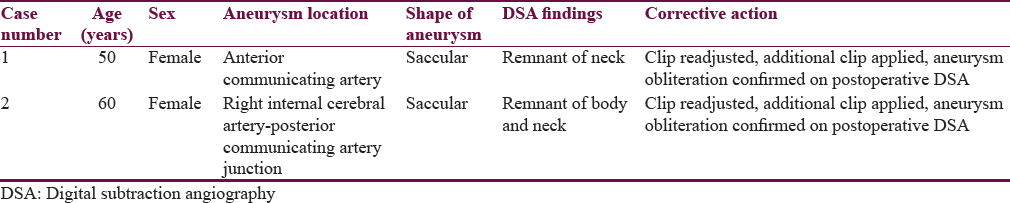
Postoperative DSA showed aneurysm remnant in two patients [Table 2] although intraoperative ICG-VA did not show any remnant during the first operative intervention. These patients were reoperated, the aneurysm remnants were identified under ICG-VA, and complete occlusion of aneurysm was performed with readjustment of the original clip with an extra clip placement [Figure 1a-e]. Repeat postoperative DSA did not reveal any aneurysm remnant. In this study, 1 (3.3%) patient had complication following DSA in the form of hemiparesis.
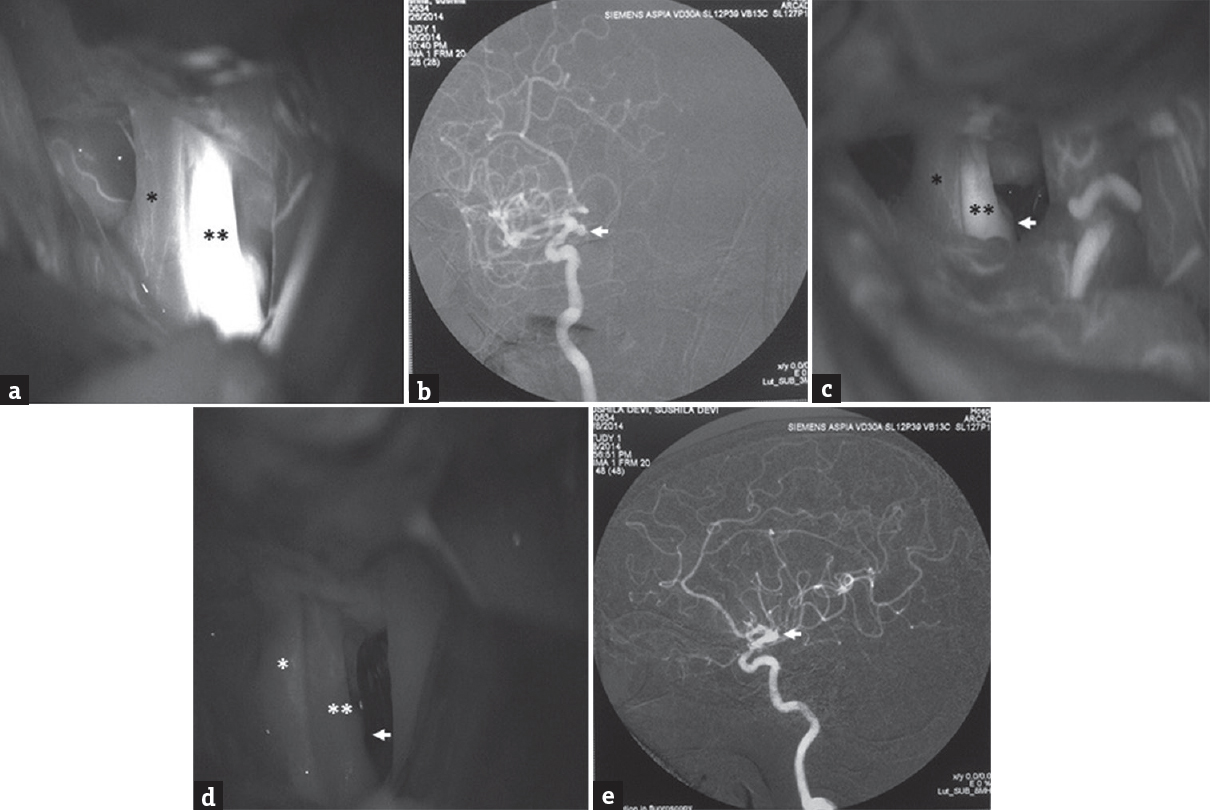
- (Case 1): (a) Intraoperative indocyanine green videoangiography showing the right optic nerve (*), right internal carotid artery (**), and internal carotid artery-posterior communicating artery junction aneurysm before applying the clip during the first surgery; (b) postoperative digital subtraction angiography, oblique view, and showing the remnant of body and neck of aneurysm at right internal carotid artery-posterior communicating artery junction (arrowhead) after first surgery; (c) intraoperative indocyanine green videoangiography showing the right optic nerve (*), right internal carotid artery (**), and internal carotid artery-posterior communicating artery junction aneurysm remnant (arrowhead) single aneurysm clip during the second surgery; (d) delayed phase of intraoperative indocyanine green videoangiography showing the right optic nerve (*), right internal carotid artery (**), and internal carotid artery-posterior communicating artery junction aneurysm showing no aneurysm remnant (arrowhead) after the adjustment of clip with an additional clip placement during the second surgery; (e) postoperative digital subtraction angiography, lateral view, showing complete obliteration of aneurysm at the right internal carotid artery-posterior communicating artery junction (arrowhead) after the second surgery
The sensitivity of intraoperative ICG-VA was 91.7% and the specificity was 93.3% with the P <0.0001.
DISCUSSION
Intraoperative or postoperative cerebral angiography is required to ascertain the completeness of clipping to avoid rebleed from residual aneurysm if it exists and to ascertain inadvertent vessel or perforator occlusion. The rebleed rate reported by Drake et al. in long-term follow-up of the patients with extremely complex aneurysms was 10%.[3] Macdonald et al. reported 11.5% incidence of compromised blood flow due to accidental stenosis and 10.3% eventually suffered a serious stroke or death.[4] Alexander et al. found that approximately 12% of cases with intracranial aneurysm clipping were associated with unexpected residual aneurysm with major arterial occlusion.[5] In these studies, no intraoperative imaging was used to confirm the completeness of clipping of an aneurysm with sparing of any vessel from the clip. The present study detected 23.3% incidence of the residual neck during intraoperative ICG-VA and 3.3% incidence of entrapment of major vessel in the clip. These patients would have been potential candidates for rebleed or appearance of the new neurological deficit. The sensitivity and specificity of intraoperative ICG-VA in the present study signifies the importance and need of intraoperative ICG-VA.
In a retrospective study, Kivisaari et al. reported incomplete aneurysm occlusion and vessel occlusion in one-sixth of the patients on postoperative angiography even in experienced hands.[6] Various studies have reported aneurysmal remnants on perioperative angiography ranging from 1.8% to 36% and unintended vessel occlusion in 1.6%–21% of cases, resulting in rebleed risk in 3.7%–47% of cases in the former group, and postoperative stroke in 16%–50% of cases in the latter group.[478910]
The discordance between ICG-VA and intraoperative DSA reported by Caplan et al.[11] was 10.8%, whereas Washington et al.[12] reported this to be 14.3%. The incidence of discordance between ICG-VA and postoperative DSA reported by Doss et al.[13] was 21.07%. In our study, the discordance between ICG-VA and postoperative DSA was 6.7% and is statistically significant (P < 0.0001). The less incidence in the present study perhaps is due to better dissection and trying to see aneurysm all around while seeing under ICG-VA.
DSA is considered to be gold standard to evaluate the completeness of the clipping of aneurysm; however, it has its limitation of a complication rate of 0.4%–3.5% in the form of neurological deficits, groin or retroperitoneal hematoma, arterial dissection or occlusion, pseudoaneurysm at the puncture site, or contrast allergy. In our study, 1 (3.3%) patient had post-DSA complication.
Intraoperative ICG-VA has its limitation of not providing 3D imaging of vessels and aneurysms. The vessels directly visible in the operative field can only be assessed; vessels that are covered by blood clots and aneurysm or brain tissue are not visible. Calcifications, atherosclerotic plaque, or thick wall of the aneurysm may attenuate the fluorescent signals and affect the results. During the ICG-VA process, the surgeon may need to retract the brain tissue and vessels gently or adjust the angle of microscope to get the optimal view of different vessels. The surgeon should be well versed with the anatomy and the specific vessels that are to be seen. In this study, the cause of discordance on ICG-VA and postoperative DSA could be due to reduced clip pressure resulting in the displacement of clip postoperatively or increased blood pressure in the postoperative period leading to the displacement of clip or due to incomplete occlusion of aneurysm which was not detected by the ICG-VA.
CONCLUSIONS
Intraoperative ICG-VA is a sensitive, specific, and costeffective tool for the assessment of completeness of microsurgical clipping of intracranial aneurysms leading to better outcomes and decreased complications. It can replace the requirement of postoperative imaging in a selected group of patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Prospective comparison of intraoperative vascular monitoring technologies during cerebral aneurysm surgery. Neurosurgery. 2011;68:657-73.
- [Google Scholar]
- Subtemporal approach to basilar tip aneurysm with division of posterior communicating artery: Technical note. Vasc Health Risk Manag. 2008;4:931-5.
- [Google Scholar]
- Surgery of Vertebrobasilar Aneurysms: London, Ontario Experience on 1,767 Patients. New York: Springer-Verlag; 1996.
- Intraoperative angiography in cerebral aneurysm surgery: A prospective study of 100 craniotomies. Neurosurgery. 1996;39:10-7.
- [Google Scholar]
- Routine cerebral angiography after surgery for saccular aneurysms: Is it worth it? Neurosurgery. 2004;55:1015-24.
- [Google Scholar]
- Late angiographic follow-up review of surgically treated aneurysms. J Neurosurg. 1999;91:396-401.
- [Google Scholar]
- Optimal clip application and intraoperative angiography for intracranial aneurysms. Surg Neurol. 1999;51:117-24.
- [Google Scholar]
- Ischemic complications of surgery for anterior choroidal artery aneurysms. J Neurosurg. 2001;94:565-72.
- [Google Scholar]
- Impact of indocyanine green videoangiography on rate of clip adjustments following intraoperative angiography. Neurosurgery. 2014;75:437-43.
- [Google Scholar]
- Comparing indocyanine green videoangiography to the gold standard of intraoperative digital subtraction angiography used in aneurysm surgery. J Neurosurg. 2013;118:420-7.
- [Google Scholar]
- Comparison of intraoperative indocyanine green angiography and digital subtraction angiography for clipping of intracranial aneurysms. Interv Neurol. 2015;3:129-34.
- [Google Scholar]






