Translate this page into:
Commentary
Address for correspondence: Dr. Alessandro Squizzato, U.O. Medicina 1, Ospedale di Circolo, Viale Borri 57, Varese, 21100, Italy. E-mail: alessandro.squizzato@uninsubria.it
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Intracranial hemorrhage (ICH) is a broad term which includes four anatomical locations of bleeding (intracerebral, subarachnoid, subdural and epidural) with different pathogenetic mechanisms.[1] Hypertension and cerebral amyloid angiopathy are the most common risk factors for spontaneous intracerebral hemorrhage, and arterial-venous malformations, tumors, and vasculopathies are associated with secondary intracerebral hemorrhage. Coagulopathies and antithrombotic drugs increase the risk of both events.[2] Subarachnoid hemorrhage, defined as bleeding into the space between the pia and the arachnoid membranes, is mainly due to rupture of cerebral aneurysms.[1] Subdural hematoma located between the dura and the arachnoid and epidural hematoma located between the dura and the bone, are usually caused by traumatic injuries.[1] Among the rare causes of ICH, infections are also mentioned.
In the current issue of the Journal of Neurosciences in Rural Practice, the authors describe the case of a young male co-infected with leptospirosis and Dengue, who developed an intracerebral hemorrhage.[3] Several mechanisms are involved in the hemorrhagic manifestations associated with these infections. Leptospirosis may not only cause coagulopathy and thrombocytopenia, but also cerebral arteritis;[3] while in patients with Dengue virus, bleeding may result from a combination of thrombocytopenia, dysfunctional platelets and increased fibrinolysis, or from disseminated intravascular coagulation.[4] Moreover, the synergistic action of these two microorganisms may result in endothelial dysfunction. Leptospira components activate leukocytes and stimulate the production of pro-inflammatory cytokines, with increased synthesis of nitric oxide, one of the major mediators of endothelial dysfunction in sepsis. In Dengue hemorrhagic fever, the immunopathological mechanism plays a major role. The Dengue virus, detected in the endothelium, does not cause a direct damage: Antibodies against the virus cross-react with endothelial cells, leading to the expression of cytokines and adhesion molecules and resulting in altered hemostatic system.[3]
Other infective causes of ICH have been described in the literature. Catastrophic ICHs have been reported during the course of perinatal enterovirus or herpes simplex virus sepsis.[5] The pathogenic mechanism is likely due to direct infection of the central nervous system, in combination with virus-induced thrombocytopenia and coagulopathy. ICH may also complicate cytomegalovirus infections, especially in neonates with vitamin K deficiency due to viral hepatitis and cholestasis.[6] In adult patients, Varicella-Zoster virus may invade the vessel wall and may induce a non-cytolytic infection of the smooth muscle cells in the media and a functional damage to the vascular endothelium. The result may be a necrotizing cerebral vasculitis with ICH.[7]
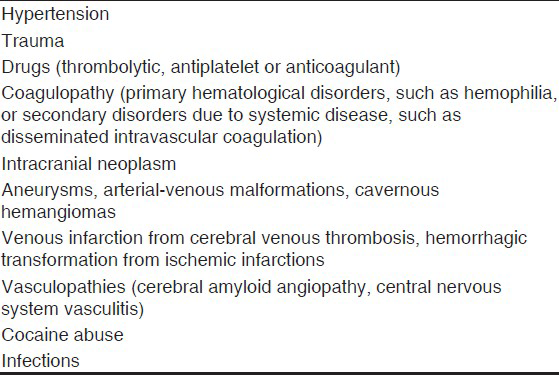
Among bacterial infections, cerebrovascular diseases are frequent complications of infective endocarditis. Three different mechanisms may result in ICH: Hemorrhagic transformation of ischemic infarcts from sterile emboli; acute erosive arteritis from septic emboli during uncontrolled infections; development of mycotic aneurysms from continuous arterial wall injury caused by the septic emboli during the effective antimicrobial therapy.[8] ICH is also a rare, but devastating complication in patients with community-associated bacterial meningitis, caused by Streptococcus pneumoniae, Staphylococcus aureus, Pseudomonas aeruginosa and Listeria monocytogenes.[9] The underlying pathophysiological mechanisms are microvascular damage, vasculitis and cerebral infarction. The dysregulation of both coagulation and fibrinolytic pathways, after massive clotting in the central nervous system, may hypothetically result in local depletion of coagulation factors.[9] Finally, ICHs have been described also in young people with typhoid fever. Salmonella endotoxin may stimulate the phagocytosis of neutrophils, red blood cells and platelets by the histiocytes in the bone marrow, resulting in pancytopenia.[10] Moreover, thrombocytopenia is worsened by decreased production and immune-mediated destruction of platelets.[10] In conclusion, viral and bacterial infections are rare causes of ICH. The evaluation of a patient with ICH should take into consideration the potential different causes, beginning with the most common risk factors, such as hypertension, amyloid angiopathy; trauma and coagulopathy [Table 1]. The location of intracranial bleeding might also help in the overview. ICH as the only presentation of Leptospirosis or Dengue fever is rare. However, in the presence of signs or symptoms of infection (e.g., fever, leukocytosis), preceding the development of ICH, an infective aetiopathogenesis should be investigated. Dengue fever should be suspected in patients coming from endemic areas for the Aedes aegypti mosquito, the vector of Dengue virus, such as Southeastern Asia, Central and Southern America or Eastern Africa. Leptospirosis is a zoonosis transmitted by feral and domestic animals and has a worldwide distribution, being endemic mainly in countries with humid subtropical or tropical climate. In these areas, the appropriate diagnostic tests need to be done for the correct management.
References
- Intracranial haemorrhage in a patient co-infected with dengue and leptospirosis. J Neurosci Rural Pract. 2013;4:366-67.
- [Google Scholar]
- Coagulation abnormalities in dengue hemorrhagic Fever: Serial investigations in 167 Vietnamese children with dengue shock syndrome. Clin Infect Dis. 2002;35:277-85.
- [Google Scholar]
- Catastrophic intracranial hemorrhage complicating perinatal viral infections. Pediatr Infect Dis J. 2000;19:556-9.
- [Google Scholar]
- Vitamin K-deficient intracranial hemorrhage as the first symptom of cytomegalovirus hepatitis with cholestasis. Tohoku J Exp Med. 2007;212:335-9.
- [Google Scholar]
- Varicella-zoster vasculitis presenting with intracranial hemorrhage. AJNR Am J Neuroradiol. 2003;24:971-4.
- [Google Scholar]
- Mechanisms of intracranial hemorrhage in infective endocarditis. Stroke. 1987;18:1048-56.
- [Google Scholar]
- Intracerebral hemorrhages in adults with community associated bacterial meningitis in adults: Should we reconsider anticoagulant therapy? PLoS One. 2012;7:e45271.
- [Google Scholar]
- Intracranial haemorrhage in typhoid fever. J Coll Physicians Surg Pak. 2008;18:522-3.
- [Google Scholar]





