Translate this page into:
Clinical Predictors of Vibrator-Assisted Ejaculation following Spinal Cord Injury: A Prospective Observational Study
Bobeena Rachel Chandy, MD, DNB (PMR) Department of Physical Medicine and Rehabilitation, Christian Medical College Vellore 632004, Tamil Nadu India bobeenachandy@cmcvellore.ac.in
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Introduction Infertility in men with spinal cord injury (SCI) occurs due to combination of factors like erectile dysfunction, ejaculatory failure, and semen abnormalities. Penile vibratory stimulation (PVS) is a known method of treatment for anejaculation. Predicting successful outcome of PVS depends on several clinical factors, which assess the intactness of the neural arc pertaining to the spinal ejaculation pattern generator. This study reports the clinical predictors for successful candidacy for a PVS trial in males with SCI.
Methods Twenty-three males with SCI, satisfying the inclusion criteria, were recruited in this prospective observational study. Participants underwent two trials of PVS with single high-amplitude vibrator. The clinical predictors recorded were neurological level, superficial abdominal reflex, cremasteric reflex, bulbocavernosus reflex, plantar reflex, ankle jerk, knee jerk, lower abdominal sensation, and hip flexor response. In addition, somatic responses during PVS were recorded and corelated. Participants who had successful ejaculation were “responders” and the others were termed as “nonresponders.” Binary logistic regression analysis of the clinical parameters was done to compare responders against nonresponders.
Results Of the twenty-three males (mean age 33.2 ± 6.8 years) with paraplegia, all four persons with neurological level above T9 had successful ejaculation with PVS. Among all the clinical parameters in the study, presence of somatic responses showed statistical significance in predicting successful ejaculation (p-value = 0.02).
Conclusion This study reports that in men with SCI, along with the level of injury, somatic responses and other clinical reflexes, should be considered concurrently to predict the outcome of vibrator assisted ejaculation.
Keywords
penile vibratory stimulation
spinal cord injury
ejaculation
Introduction
The life-span of individuals with spinal cord injury (SCI) has improved significantly over the years.1 The incidence of SCI varies globally with changing epidemiological trends.2 3 A systematic review done by van den Berg et al showed an incidence range of 12.1 per million to 57.8 per million with a bimodal age distribution.2 In India, the incidence is estimated to be 15 to 20 per million per year population.4 Worldwide, males are more commonly affected than females.5 Males with SCI may have erectile function preserved but up to 95% men have an impairment of ejaculatory function.6 Individuals with paraplegia following SCI have rated regaining of sexual function as an important priority, irrespective of time since injury.7 Sexual rehabilitation comprises family counseling followed by trial of medications and injectable agents to assist sexual function and vibrator-assisted erection/ejaculation. This aspect of rehabilitation is offered to individuals during their inpatient stay or outpatient visits.8 The factors causing reduced fertility among males with SCI are impaired genital arousal (erection), ejaculatory dysfunction, and abnormal quality of semen.9 Infertility is a major concern in males with SCI and often require alternate methods to aid in collection of semen for assisted reproduction.10 Penile vibratory stimulation (PVS) and electroejaculation are well-known techniques for semen collection.11 PVS is noninvasive and does not require any major equipment or technical assistance. The present study aimed to assess the response to PVS in males with SCI, and if the outcome can be predicted with clinical evaluation.
Methods
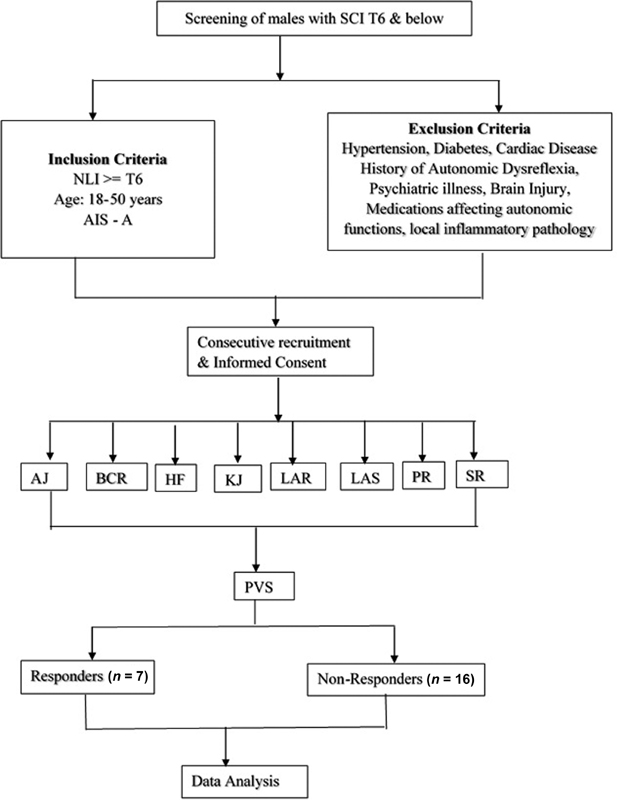
Males with SCI undergoing inpatient rehabilitation were recruited after a valid and informed consent, which adhered to the ethical guidelines of the Declaration of Helsinki and its amendments. The study was approved by the Institutional Review Board and Ethics Committee of a tertiary care teaching hospital in south India where the study was conducted. Males with complete spinal cord injury (ASIA impairment scale [AIS] A) in the age group 18 to 50 years who have been injured for more than 6 months, and with neurological level of injury T6 and below, were included in the study. Participants with a neurological level above T6 are vulnerable for autonomic dysreflexia during ejaculation and hence were excluded from the study.12 Subjects with untreated hypertension, diabetes, cardiac disease, history of autonomic dysreflexia, coexisting psychiatric illness or brain injury, on regular medications affecting the autonomic functions, or those with local acute inflammatory pathology were also excluded from the study. Further, all participants included were AIS A to maintain uniformity in the group (Fig. 1). Incomplete injuries with partially preserved reflex pathways would confound the inference to be drawn from the study.
-
Fig. 1 Study flow diagram. AJ, ankle jerk; BCR, bulbocavernosus reflex; HF, hip flexor response; KJ, knee jerk; LAR, lower abdominal response; PR, plantar reflex; PVS, penile vibratory response; SR, somatic response; SCI, spinal cord injury.
Fig. 1 Study flow diagram. AJ, ankle jerk; BCR, bulbocavernosus reflex; HF, hip flexor response; KJ, knee jerk; LAR, lower abdominal response; PR, plantar reflex; PVS, penile vibratory response; SR, somatic response; SCI, spinal cord injury.
Participants fulfilling the inclusion criteria underwent a detailed clinical neurological examination (including superficial reflexes, deep tendon jerks, hip flexor response) in accordance with current practice and international guidelines (Fig. 1).13 14 Firmly stroking the sole of the foot causes a hip flexion response, which is a pathological flexion reflex. This is commonly seen in individuals with SCI and demonstrates the integrity of spinal cord up to L2 segment.15
The primary outcome of the study was response to PVS and secondary outcome measure was somatic responses during PVS. The clinical predictors recorded were neurological level, superficial abdominal reflex (T6-T12), cremasteric reflex (L1, L2), bulbocavernous reflex (S2-S3), plantar reflex (S1), ankle jerk (S1-S2), knee jerk (L2-L4), lower abdominal sensation (T10-T12), and hip flexor response (L2, S2). During PVS, the somatic responses that were observed included abdominal contraction (T6-T12), hip flexion (L2), hip adduction (L2), lower limb withdrawal (hip flexion accompanied by knee flexion and adduction of the thigh), lower extremity spasms, and piloerection. These responses and reflexes were selected to confirm the integrity of the spinal segments conveying these responses as well as their afferent and efferent pathways. The presence or absence of these somatic responses were documented, and correlation was drawn with the ejaculatory response.
Patients were positioned supine, and their vitals (blood pressure and heart rate) were measured with an automated monitoring device. It has been reported that success to PVS is greater with a higher amplitude vibrator.16 In this study, a high amplitude vibrator (FERTICARE personal, Multicept, Denmark) having 3.5 mm amplitude of vibration and frequency of 100 Hz was used. The vibratory stimulation was given for 5 minutes, followed by a period of 5-minute rest. This cycle was repeated twice. The stimulation was stopped on ejaculation, or if there was anejaculation in the presence of signs suggestive of sympathetic activation, like increased blood pressure, increase in heart rate, sweating, headache, and piloerection.17 As the males with SCI may not have sensation, a successful response may not be felt and reported by the patient. Moreover, the uncoordinated internal and external urethral sphincter may result in the semen flowing into the urinary bladder in a retrograde manner.18 Hence, catheterization was done for all patients before PVS to ensure that the bladder was empty. For individuals with retrograde ejaculation, postprocedure catheterization was done to collect urine, which was then examined for the presence of spermatozoa. The males who had a successful response to PVS were classified as “responders,” and those who did not have any ejaculatory response were considered as “nonresponders.”
The data for responders and nonresponders to PVS was compared by binary logistic regression analysis of the clinical parameters. A p-value less than 0.05 was considered statistically significant.
Results
The present study included 23 men with paraplegia mean (standard deviation [SD]) age was 33.2 ± 6.8 years. The most common cause of SCI was fall from height (n = 14), followed by road traffic accident (n = 8) and heavy object falling on the body (n = 1). The mean duration since injury was 45 months. All the participants reported normal erection and ejaculation prior to the SCI. Most participants in this study were married (n = 15) as shown in Table 1. The mean (SD) age of responders was 34.1 ± 7.8 years and that of nonresponders was 32.8 (6.6) years. Following SCI, 19 (82%) participants reported that they had erection and six (26%) individuals had successful ejaculatory response to natural methods (Table 1).
|
Age (years) |
Mean ± SD |
33 ± 6.8 |
|
Median (range) |
28 (24 - 47) |
|
|
Duration since trauma (months) |
Mean ± SD |
45 ± 52 |
|
Median (range) |
32 (6 - 226) |
|
|
n (%) |
||
|
Marital status |
Married |
15 (65.2) |
|
Unmarried |
8 (34.7) |
|
|
Sexual function after SCI |
Erection + ve |
19 (82.6) |
|
Erection – ve |
4 (17.4) |
|
|
Ejaculation + ve |
6 (26.0) |
|
|
Ejaculation – ve |
17 (74) |
|
|
Mode of trauma |
Fall from height |
10 (43.4) |
|
Road traffic accident |
8 (34.7) |
|
|
Fall after electrocution |
4 (17.3) |
|
|
Fall of heavy object on back |
1 (4.3) |
|
|
Neurological level |
T6-T8 |
4 |
|
T9-T12 |
19 |
Abbreviations: SD, standard deviation; SCI, spinal cord injury.
It was observed that all the four participants with higher level of injury (T6-T8) were responders (100%), whereas among the 19 individuals with a lower neurological level (T9-T12), only three (18%) were responders. The neurological level of injury and response to PVS has been shown (Table 2). Of the 23 participants, there were 4 responders among 14 patients with absent knee jerk, and 3 responders among 9 persons with preserved knee jerk. The plantar reflexes were absent in 14 (with four responders) and preserved in nine patients (with three responders). The ankle jerks were absent in 16 patients (with five responders) and present in seven (with two responders). Lower abdominal sensations and reflexes were preserved in 8 patients, of whom three persons had a successful response to PVS. Bulbocavernosus reflex was present in 15 patients, of whom five were responders, and absent in eight subjects with two responders. Cremasteric reflex was absent in all patients.
|
Neurological level |
Responders to PVS |
Nonresponders to PVS |
|---|---|---|
|
T6-T8 |
4 |
0 |
|
T9-T12 |
3 |
16 |
|
Total |
7 |
16 |
Abbreviation: PVS, penile vibratory stimulation.
The somatic responses that were observed were abdominal contraction alone in two participants, hip flexion alone in one participant, and abdominal contraction with hip flexion in two persons. The somatic responses were seen in 11 patients (with five responders), whereas among 12 participants who had absent somatic responses, only one person had successful ejaculation. Thus, presence of somatic responses during PVS was able to predict successful vibrator-assisted ejaculation (p = 0.02). Table 3 summarizes the results obtained from various clinical predictors. Lower extremity spasms, withdrawal response, and piloerection were not observed among the participants. Urine microscopy postprocedure for the 16 nonresponders did not show the presence of spermatozoa. Of the 7 responders, only one participant was found to have live spermatozoa in urine postprocedure.
|
Clinical predictors |
Response to PVS |
p-value |
||
|---|---|---|---|---|
|
Yes |
No |
|||
|
Knee jerk |
Present |
3 |
6 |
0.7437 |
|
Absent |
4 |
10 |
||
|
Ankle jerk |
Present |
2 |
5 |
0.2958 |
|
Absent |
5 |
11 |
||
|
Plantar reflex |
Present |
3 |
6 |
0.3752 |
|
Absent |
4 |
10 |
||
|
Lower abdominal reflex |
Present |
3 |
5 |
0.7584 |
|
Absent |
4 |
11 |
||
|
Bulbocavernosus reflex |
Present |
5 |
10 |
0.7584 |
|
Absent |
2 |
6 |
||
|
Hip flexor response |
Present |
2 |
5 |
0.2481 |
|
Absent |
5 |
11 |
||
|
Lower abdominal sensation |
Present |
3 |
5 |
0.7584 |
|
Absent |
4 |
11 |
||
|
Somatic response |
Present |
5 |
5 |
0.02057 |
|
Absent |
1 |
12 |
||
Abbreviation: PVS, penile vibratory stimulation.
Discussion
Infertility is often a frustrating problem encountered by males with SCI. A variety of factors including ill sustained erection, ejaculatory failure, or poor semen quality contribute to this complex situation. Since a considerable population of males with SCI are young, the anxieties and apprehensions toward their fertility is a major concern encountered during rehabilitation. This study addresses the frequent question raised during sexual counseling, whether vibrator assistance could result in successful ejaculation. The study was designed to assess whether ejaculatory response to PVS can be predicted with clinical assessment.
In our study, participants with higher neurological level of injury had successful response to stimulation. All four patients with neurological level of injury T6-T8 were responders, whereas among the 19 individuals with a lower neurological level (T9-T12), only three were responders. In persons with higher level of injury, the presence of an intact thoracolumbar (T10-L2) and sacral (S2-S4) centers along with intact neural pathways to these centers may have resulted in their better response to PVS.
The neurological pathways of erection and ejaculation have been elaborated in literature. These two pathways are independent of each other, wherein erection may not lead to ejaculation, and ejaculation can occur without erection as well.19 For erection, there is arteriolar vasodilatation of corpora cavernosa, mediated by the parasympathetic neurons located at sacral segments (S2-S4). This conveys signals through cholinergic pelvic nerve to the postganglionic neurons which, in turn, releases nitric oxide as a neurotransmitter, leading to intense vasodilatation of the cavernosal arteries causing erection. Sensory afferents from the genitalia is conveyed through pudendal nerve through the sacral segments (S2-S4), the stimulation of which can cause reflex erections. Contraction of ischiocavernosus sustains the erection, whereas rhythmic contractions of bulbospongiosus causes propulsive anterograde ejaculation.20 Concurrent bladder neck contraction prevents retrograde ejaculation.
Sustained erection increases the secretion of seminal vesicles and prostrate, causing emission through sympathetic adrenergic stimulation. High pressures generated in the prostatic urethra elicits ejaculation, activating the somatic pathways and causing contractions of bulbospongiosus and anterograde expulsion of semen. A spinal reflex ejaculation center has been proposed at the thoracolumbar segments of the spinal cord. Patients with SCI present with disorders of erection or ejaculation, depending on the extent and level of the injury. Since the pathways of erection and ejaculation involve several spinal segments and nerves, a series of reflex and somatic responses were elicited in patients with SCI in our study to interrogate the integrity of these pathways.
In a retrospective study published in 2007 by Brackett et al, 49% individuals with level T10 and 57% above this level had successful response to PVS, using one vibrator stimulation. However, only 15% individuals with neurological level T11 and below showed a successful response.21 The same authors in another study published in 2010, on treatment of ejaculatory dysfunction in men with SCI, noted that in persons with T10 and caudal neurological injury level, PVS failure may be attributed to disrupted ejaculatory reflex arc, which relies on the intactness of T11-S4 spinal segments of the spinal cord.22 Bird et al reported overall success of 73% and 35% with PVS for persons with neurological level T1-T6 and T6-T12, respectively.15 Similar observations were made in an Asian population by Zamli et al, in which 66.7% and 33.3% of the participants with neurological level above T6 and below T6, respectively, had successful response to PVS.23 Our study corroborates these observations. All the four participants with higher level of injury (T6-T8) were responders (100%), whereas among the 19 participants with a lower neurological level (T9-T12), only three (18%) were responders.
In our study, the bulbocavernosus reflex was absent in eight participants, denoting that the sacral (S2-S4) pathway was affected. However, even in the absence of bulbocavernosus reflex, two individuals responded to PVS. This may be due to sparing of spinal pattern generator (L3-L5) for ejaculation as documented in literature.24
The clinical parameters which can be used for assessing the intactness of spinal ejaculation pattern generator (L3-L5) are hip flexor response (L2–S1) and the knee jerk (L2-L4). The hip flexor response was observed in seven patients, among whom only two were responders. There were three responders among the nine subjects whose knee jerk was not preserved. The preservation of spinal ejaculation pattern generator (L3-L5) will aid in initiating ejaculation and facilitating synchronous activity of sympathetic, parasympathetic and somatic centers.24 The findings in our study suggest that in persons with clinical examination suggestive of disruption of neural arcs to the spinal ejaculation pattern generator, the possibility of a negative response to PVS is higher.
We found that in the seven participants with positive bulbocavernosus reflex and hip flexor response, only two persons (28%) responded to PVS. In eight participants with absent bulbocavernosus reflex and hip flexor response, two individuals (25%) were responders to PVS. This was unlike a previous study by Bird et al, where four out five patients (80%) with positive bulbocavernosus reflex and hip flexor response had ejaculation with PVS. Moreover, only 8% participants with negative bulbocavernosus reflex and hip flexor response had positive response to PVS in their study.15
Somatic responses that were observed among the participants were abdominal contraction, hip flexion, and hip adduction. Lower extremity spasms, withdrawal response, and piloerection were not observed among our participants, as reported in a prior study done at Miami by Bird et al.15 In the present study, among the12 participants who did not have somatic responses, only one had successful ejaculation to PVS. Thus, somatic responses were found to be statistically significant (p = 0.02) in predicting the outcome of PVS. Our observations suggest that PVS trial is likely to be unsuccessful when somatic responses are absent.
It has been observed that the efficacy of PVS increases with the use of two devices simultaneously.21 25 The present study used a single high-amplitude vibrator as compared with vibratory stimulation with two devices simultaneously. In addition, no medications were administered (midodrine, ephedrine, physostigmine) to facilitate ejaculation.
Conclusion
In our study of 23 spinal cord injured participants to assess the clinical predictors of successful response to vibrator-assisted ejaculation, it was observed that persons with a neurological level of injury above T9 responded to PVS, suggesting that the intactness of the thoracolumbar (T10-L2) and sacral centers were associated with successful outcome of the procedure. When determining the candidacy for a trial with PVS, the level of injury should not be the sole factor; in addition, the presence or absence of the clinical reflexes such as somatic responses should also be considered concurrently.
We observed that in persons with SCI, clinical examination suggestive of disruption of neural arc to the spinal ejaculation pattern generator (absence of hip flexion response and knee jerk) and absence of somatic responses are negative predictors for vibrator-assisted ejaculation. Further, the presence of somatic reflexes during the PVS trial should aid in deciding to continue with the trial or offer a repeat trial if there was no successful ejaculation initially.
Acknowledgments
The authors thank the Institutional Fluid Research Grant, Christian Medical College, Vellore for funding the study.
Conflict of Interest
None declared.
Funding This study was supported by the Institutional Fluid Research Grant, Christian Medical College, Vellore.
References
- Long-term survival after traumatic spinal cord injury: a 70-year British study. Spinal Cord. 2017;55(7):651-658.
- [Google Scholar]
- Incidence of spinal cord injury worldwide: a systematic review. Neuroepidemiology. 2010;34(3):184-192. , discussion 192
- [Google Scholar]
- Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol. 2014;6:309-331.
- [Google Scholar]
- Epidemiology of traumatic spinal cord injury. Int J Mol Biol Biochem.. 2015;3:9-22.
- [Google Scholar]
- Gender differences in spinal injuries: causes and location of injury. J Womens Health (Larchmt). 2018;27(7):946-951.
- [Google Scholar]
- Impact of spinal cord injury on sexuality: broad-based clinical practice intervention and practical application. J Spinal Cord Med. 2012;35(4):211-218.
- [Google Scholar]
- Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004;21(10):1371-1383.
- [Google Scholar]
- Reproductive health of men with spinal cord injury. Top Spinal Cord Inj Rehabil. 2017;23(1):31-41.
- [Google Scholar]
- Advances in the management of infertility in men with spinal cord injury. Asian J Androl. 2016;18(3):382-390.
- [Google Scholar]
- Electroejaculation versus vibratory stimulation in spinal cord injured men: sperm quality and patient preference. J Urol. 1997;157(6):2147-2149.
- [Google Scholar]
- Sexual function and autonomic dysreflexia in men with spinal cord injuries: how should we treat? Spinal Cord. 2012;50(12):869-877.
- [Google Scholar]
- International Standards for Neurological Classification of Spinal Cord Injury (revised 2011) J Spinal Cord Med. 2011;34(6):535-546.
- [Google Scholar]
- Reflexes and somatic responses as predictors of ejaculation by penile vibratory stimulation in men with spinal cord injury. Spinal Cord. 2001;39(10):514-519.
- [Google Scholar]
- An analysis of 653 trials of penile vibratory stimulation in men with spinal cord injury. J Urol. 1998;159(6):1931-1934.
- [Google Scholar]
- Clinical observations in vibratory stimulation of the penis of men with spinal cord injury. Arch Sex Behav. 1989;18(6):461-474.
- [Google Scholar]
- Ejaculatory dysfunction in spinal cord injury men is suggestive of dyssynergic ejaculation. Eur J Phys Rehabil Med. 2011;47(4):677-681.
- [Google Scholar]
- Neuroanatomy and neurophysiology related to sexual dysfunction in male neurogenic patients with lesions to the spinal cord or peripheral nerves. Spinal Cord. 2010;48(3):182-191.
- [Google Scholar]
- Application of 2 vibrators salvages ejaculatory failures to 1 vibrator during penile vibratory stimulation in men with spinal cord injuries. J Urol. 2007;177(2):660-663.
- [Google Scholar]
- Treatment for ejaculatory dysfunction in men with spinal cord injury: an 18-year single center experience. J Urol. 2010;183(6):2304-2308.
- [Google Scholar]
- Retrospective review on effectiveness of high-amplitude penile vibratory stimulation for conservative sperm retrieval in anejaculatory men with spinal cord injury: an Asian case series. Spinal Cord Ser Cases. 2016;2:15038.
- [Google Scholar]
- Comparison of three methods of penile vibratory stimulation for semen retrieval in men with spinal cord injury. Spinal Cord. 2017;55(10):921-925.
- [Google Scholar]






