Translate this page into:
Cisternostomy in Neurosurgery: A New Proposed General Classification Based on Mechanism and Indications of the Cisternostomy Proper
Address for correspondence: Dr. Luis Rafael Moscote-Salazar, Department of Neurosurgery, Red-Latino-Colombia. E-mail: mineurocirujano@aol.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Cerebral ventricular, subarachnoid, perivascular, and interstitial compartments constitute a continuum or a fluid functional unit.[1] Cisternostomy, a novel technique, incorporates knowledge of skull base and microvascular surgery.[2] Cisternostomy can be used in a variety of pathological conditions such as ruptured aneurysm, arteriovenous malformations (AVM), tumors and intracerebral hemorrhage,[3] management of hydrocephaly and, recently, in severe traumatic brain injury (TBI).[34]
CLASSIFICATION OF CISTERNOSTOMY ACCORDING TO THE MECHANISM OF ACTION
The cisternostomy as a procedure can be either an outflow corridor for the cerebrospinal fluid (CSF) from the ventricular system to the cisternal subarachnoid space or an inflow corridor for the atmospheric pressure to be opened on the basal cistern and equalize cisternal and external pressure aiming for brain relaxation, hence we suggest to classify cisternostomy into two broad categories as follows:
-
Outflow corridor: when the cisternostomy procedure provides a drainage pouch for the ventricular CSF and/or closed fluid containing compartments. This includes the following:
-
Ventriculocisternostomy: Shunt of the ventricular CSF is the only possible operation for obstructive hydrocephalus whenever the causal lesion cannot be eliminated. The choice of the procedure employed depends on the degree of permeability of the subarachnoid spaces. Ventriculocisternostomy has the greatest change of success if the subarachnoid spaces are permeable and if the third ventricular floor bulges into the interpeduncular cistern. If the subarachnoid spaces are not patent, a ventriculoatrial or ventriculoperitoneal shunt is indicated. This is, unfortunately, frequently the case in infancy and also in young or adult patients with the so-called “communicating” hydrocephalus secondary to meningitis or subarachnoid hemorrhage. Ventriculocisternostomy has two primary indications: (1) nontumoral aqueductal stenosis in young or adult patients – which is the ideal indication and (2) tumoral aqueductal stenosis – palliative procedure for inoperable tumors (for example, brainstem gliomas) or the first step before radiotherapy or surgical exploration of tumors of the pineal region.[4] This mechanism can be applied on the classic endoscopic third ventriculostomy and also for its emerging alternative procedures, these alternatives include subfrontal endoscopic fenestration of the lamina terminalis (EFLT), interhemispheric endoscopic fenestration of the lamina terminalis (IEFLT), and microsurgical third ventriculostomy by a minimally invasive supraorbital approach[56]
-
Cystocisternostomy: The intentional fenestration of the cyst into the subarachnoid space was done for arachnoid cysts and Rathke's cleft cysts, which were managed using drainage and cisternostomy[7]
-
-
Inflow corridor (cisternostomy proper): When the cisternostomy acts as a two-way drainage pathway to allow egress of CSF to relax the brain during the skull base and microvascular procedures (it can be used in a variety of pathological conditions such as ruptured aneurysm, AVM, tumors, and intracerebral hemorrhage)[3] and also to the blood in the cortical subarachnoid aiming to equalize the intraparenchymal pressure with the intracisternal pressure in severe TBI. (In the current common practice, the surgical measures for TBI include external ventricular drainage insertion and decompressive craniectomy [DHC]. There is evidence that both of these measures reduce intracranial pressure, but the effect on the outcome, particularly in the long term, is equivocal. A new line of evidence supports cisternostomy as an emerging surgical treatment for TBI.)[3]
Theoretically, the inflow cisternostomy can be categorized into convexity and basal cisternostomy and the latter can be divided into supratentorial and infratentorial, but the recent evidence considers the basal supratentorial cisternostomy is the cisternostomy proper [Figure 1].[8]
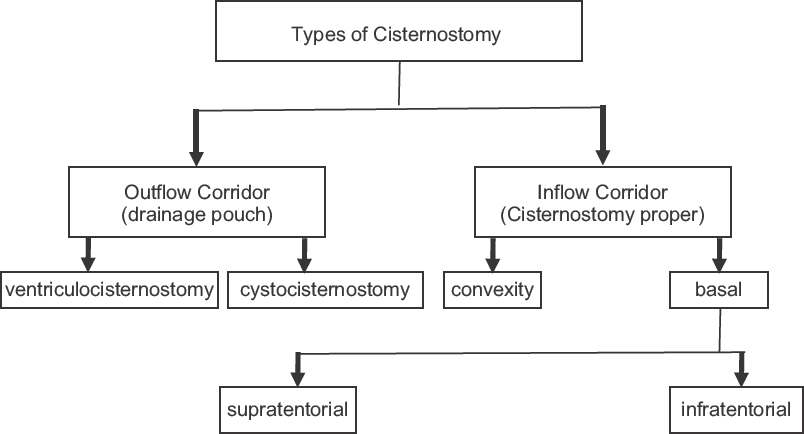
- Classification of cisternostomy according to the mechanism of action
CLASSIFICATION OF CISTERNOSTOMY PROPER ACCORDING TO THE INDICATIONS
The cisternostomy proper is defined as opening the supratentorial basal cistern on the infratentorial subarachnoid space through fenestration of the proximal sylvian, opticocarotid, chiasmatic, and suprasellar cisterns with fenestration of the Liliequist's membrane as defined by Cherian et al.[8] On review of the variable indication for cisternostomy mentioned in the literature, one can conclude two general groups of indications, either planned or unplanned cisternostomy.
The former includes the simple cisternostomy used in the skull base approaches for tumors and also for microvascular approaches for aneurysms, AVM, and intracerebral hemorrhages, and also, it can be applied for the new concept of CSF shift-edema which makes the cisternostomy as an alternative choice for the DHC. The evolution of modern neurosurgical techniques in TBI has been ongoing for the last two centuries. However, it has always been a challenge to obtain a satisfactory clinical outcome, especially those following severe traumatic brain injuries.[2] Interventions for traumatic intracranial lesions and/or raised intracranial pressure have been fairly standard, for example, medical management of raised intracranial pressure or ventricular catheterization, DHC surgical evacuation of hematoma, etc.[9] The new lines of evidence suggest that bifrontal craniectomy in those with severe TBI and refractory intracranial hypertension is not recommended. Decompressive hemicraniectomy of nondominant side in these patients is recommended. In addition, a large hemicraniectomy measuring at least 12 cm × 15 cm is recommended over a small hemicraniectomy.[10] Cisternostomy is defined as opening the basal cisterns to atmospheric pressure. This technique helps to reduce the intracranial pressure in severe head trauma as well as other conditions when the so-called sudden “brain swelling” troubles the surgeon.[8] Glymphatic system has proven that cerebrospinal fluid from the cisterns (and not from the ventricles) does communicate with the parenchyma through Virchow–Robin spaces.[1112] Glymphatic removal of excess of interstitial fluid is likely to be decreased following injury or infarction.[13] Recent evidence suggests that edema formation is also associated with CSF entrance into the brain parenchyma through the low-resistance para-arterial space or decreased interstitial fluid efflux or a combination of the two processes.[12] Accordingly, following TBI CSF could be shifted from the cerebral cisterns to the brain leading to a severe brain swelling. One of the reasons for this rapid shift may be the traumatic subarachnoid bleed, often associated with severe head trauma, causing a pressure gradient that is elevated in the cisterns and lower in the brain.[3]
The second group of indications is the unplanned cisternostomy which is applied for intraoperative brain swelling during craniotomy for and cerebral pathology. Here, the cisternostomy would reverse the direction of the CSF shift, allowing for a decrease in brain swelling. In addition, this technique would reduce the pressure in the paravascular spaces and interstitium, leading to a recovery of the functionality of the paravascular system[14] [Figure 2].
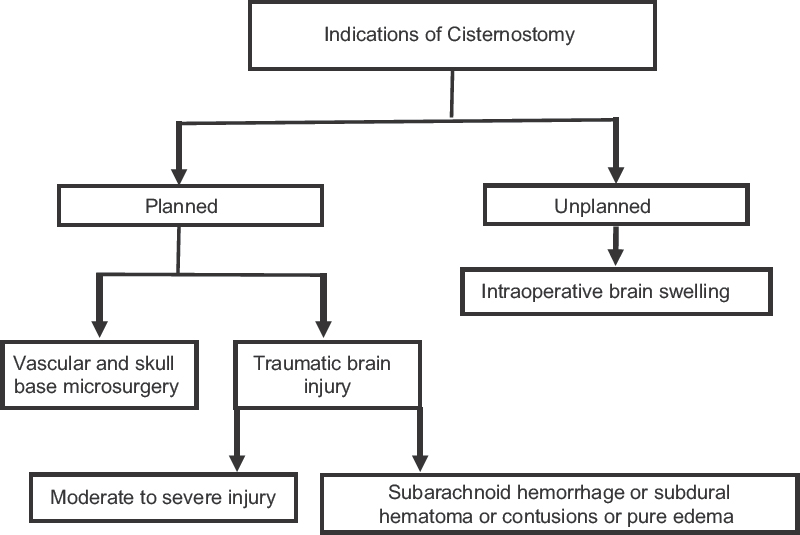
- Classification of cisternostomy proper according to the indications
CONCLUSION
Cisternostomy, a novel technique that incorporates knowledge of the skull base and microvascular surgery, has been proposed to decrease the brain swelling, mortality, and morbidity.[215] We describe two classification systems according to the mechanism of action of cisternostomy procedure and according to the indications and we think these classifications will enhance comprehension and understanding the aim and application of that procedure and also promote future laboratory research innovations aiming for maximum patient care and better quality of life.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Paravascular channels, cisterns, and the subarachnoid space in the rat brain: A single compartment with preferential pathways. J Cereb Blood Flow Metab. 2017;37:1374-85.
- [Google Scholar]
- Cisternostomy: Replacing the age old decompressive hemicraniectomy? Asian J Neurosurg. 2013;8:132-8.
- [Google Scholar]
- Cisternostomy for traumatic brain injury: Pathophysiologic mechanisms and surgical technical notes. World Neurosurg. 2016;89:51-7.
- [Google Scholar]
- Ventriculo-cisternostomy for stenosis of the aqueduct of sylvius. Puncture of the floor of the third ventricle with a leucotome under television control. Acta Neurochir (Wien). 1973;28:275-89.
- [Google Scholar]
- Microsurgical third ventriculocisternostomy as an alternative to ETV: Report of two cases. Childs Nerv Syst. 2008;24:757-61.
- [Google Scholar]
- Interhemispheric endoscopic fenestration of the lamina terminalis through a single frontal burr hole. J Neurol Surg B Skull Base. 2014;75:268-72.
- [Google Scholar]
- Endoscopic transsphenoidal cisternostomy for nonneoplastic sellar cysts. Biomed Res Int 2015 2015 389474
- [Google Scholar]
- Traumatic brain injury: Therapeutic challenges and new directions. Neurotherapeutics. 2010;7:1-2.
- [Google Scholar]
- Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80:6-15.
- [Google Scholar]
- Evaluating glymphatic pathway function utilizing clinically relevant intrathecal infusion of CSF tracer. J Transl Med. 2013;11:107.
- [Google Scholar]
- A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4:147ra111.
- [Google Scholar]
- Impairment of glymphatic pathway function promotes tau pathology after traumatic brain injury. J Neurosci. 2014;34:16180-93.
- [Google Scholar]
- Introducing the concept of “CSF-shift edema” in traumatic brain injury. J Neurosci Res. 2018;96:744-52.
- [Google Scholar]
- Surgical treatment for traumatic brain injury: Is it time for reappraisal? World Neurosurg. 2015;84:594.
- [Google Scholar]





