Translate this page into:
Chronic Subdural Hematoma Caused by Calvarial and Dural Metastasis from Uterine Leiomyosarcoma
Wai Tseung Soo, MBBS, MRCSed General Surgery Resident, Department of General Surgery, University Malaya Medical Center Kuala Lumpur Malaysia ana_xago_ras@yahoo.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Uterine Leiomyosarcoma (uLMS) is an aggressive tumor with poor clinical outcome. Skull and dural metastasis from uterine uLMS is exceptionally rare. We report a 60-year-old woman who had a 6 months' history of per vaginal bleed and abdominal pain who presented to us in a confused state and raised intracranial pressure symptoms with swelling over her right frontal-temporal region. She underwent excision of the right frontal-temporal tumor and evacuation of a right subdural hematoma (SDH), which greatly improved her condition. Postoperatively, she underwent adjuvant radiotherapy and chemotherapy. This case highlights the importance of clinical suspicion to diagnose patients with this rare metastasis to this region and the appropriate subsequent treatment. We herein report a rare case of metastatic uLMS with skull and dural metastasis that presented with SDH.
Keywords
subdural hematoma
uterine leiomyosarcoma
dura
skull
Introduction
Uterine leiomyosarcoma (uLMS) is a rare clinical entity as it represents 3% of all uterine malignancies.1 uLMS is an aggressive gynecological malignancy with poor prognosis as there is frequent presence of micro-metastasis at the time of presentation. Curative treatment for uLMS remains a challenge even with complete radical surgical resection as relapse rates are high and 5-year overall survival ranges from 25 to 76%.1 We herein report a rare case of metastatic uLMS skull and dural metastasis that presented with subdural hematoma (SDH).
Case Description
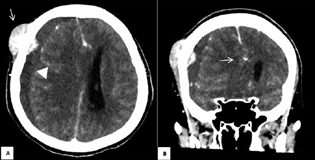
A 60-year-old woman underwent examination under anesthesia, cystoscopy, hysteroscopy, and removal of a submucosal fibroid due to post-menopausal bleed for 6 months. One month later, she presented with a right frontal-temporal scalp swelling, confusion, intense headache, lethargy, persistent per vaginal bleeding, and left-sided and lower abdominal pain. Physical examination revealed a right frontal-temporal swelling measuring 4 × 4 × 2 cm, huge palpable left upper quadrant abdominal mass, and a palpable pelvic mass sized at 18 weeks of gestation. Contrast-enhanced computerized tomography (CECT) of the brain, thorax, abdomen, and pelvis revealed right frontal-temporal skull lesion with soft tissue component and right frontotemporoparietal SDH (Fig. 1A). There was also a large uterine mass and a large heterogeneous irregular lobulated lesion at the left upper abdomen, suggestive of intra-abdominal malignancy with skull and dural metastasis causing chronic SDH, subfalcine shift (Fig. 1B) and midline shift. She underwent a right frontal-temporal craniectomy, excision of tumor, evacuation of SDH, and titanium mesh cranioplasty. The tumor was adherent to the surrounding skull bone. The surface of the tumor was smooth and had a firm consistency. There was no obvious vascular supply arising from the skin and subcutaneous tissue. The dura underlying the lesion appeared thickened and diseased with adhesions to the arachnoid mater. The tumor otherwise had not invaded the leptomeninges or underlying cerebral parenchyma. SDH was drained post duratomy. A titanium mesh cranioplasty was performed to cover the cranial defect. Postoperatively, she regained full consciousness and returned to her premorbid state with a Karnofsky performance status (KPS) scale of 90 to 100%. Her histopathological examination (HPE) findings of the cranial tumor and dura were revealed to be both leiomyosarcoma. Subsequent HPE of the submucosal fibroid concluded a uLMS with metastasis to the skull and dura. She subsequently underwent five cycles of whole brain radiation therapy and five cycles of doxorubicin for systemic chemotherapy. The patient remained in a good functional status at postoperative follow up at 6 months and a repeated magnetic resonance imaging scan showed no recurrence.
-
Fig. 1 (A) Contrast-enhanced computerized tomography (CECT) brain showing a right frontal-temporal skull lesion with soft tissue component (white arrow) and right frontotemporoparietal SDH (white arrow head). (B) CECT brain coronal cut showing the sub-falcine shift (white arrow).
Fig. 1 (A) Contrast-enhanced computerized tomography (CECT) brain showing a right frontal-temporal skull lesion with soft tissue component (white arrow) and right frontotemporoparietal SDH (white arrow head). (B) CECT brain coronal cut showing the sub-falcine shift (white arrow).
Discussion
So far, only six cases of skull and dural metastasis from primary uLMS without involvement of the brain parenchyma have been reported.2 3 4 5 However, to the best of our knowledge, there has never been any published case of SDH caused by skull and dural metastasis from a primary uLMS.
uLMS disseminates early through hematogenous spread for distant sites of metastasis such as the lungs and liver. While for peritoneal metastasis, direct implantation and nodal disease due to lymphatic spread were main methods for spread, for our cases, the skull and dural metastasis seems to arise from disseminated metastasis from diploic venous channels that expanded and eroded into the outer and inner tables of the skull and dura as reported by Chan et al.6
There are three postulated theories with regard to SDH associated with dural metastasis. The first theory is thought to arise due to edema formed by secreted materials from the tumor.7 The second theory is an angio-desmoplastic response to the tumor.8 Lastly, the most widely acceptable theory is by Russel et al that suggests impaired blood perfusion due to tumor embolism in the dural vein causes the dilation and breakdown of capillary vessels, resulting in SDH.9
At present, there is no way to diagnose uLMS preoperatively. Most patients present with common symptoms such as abnormal uterine bleeding and pain. The mainstay of staging is via CECT thorax, abdomen, and pelvis post confirmatory biopsy. A prospective study done in the US showed that there is only a 4% risk of metastasis to the brain in those with metastatic uLMS.10 Hence, there is no evidence for routine CECT brain, unless indicated.
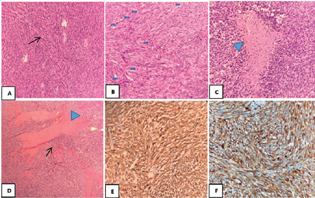
Macroscopically, uLMS presents as a single, soft, bulging, fleshy mass with a cut surface that is often necrotic and hemorrhagic. Microscopically, the diagnosis of uLMS requires the presence of two of the following three features: (1) marked cytological atypia (Fig. 2A), (2) ≥4 mitoses/mm2 (equating to ≥10 mitoses/10 HPF of 0.55 mm in diameter and 0.24 mm2 in area) (Fig. 2B), (3) tumor cell necrosis (Fig. 2C).11 These features were seen in our case. The tumor cells were also seen to infiltrate the dura (Fig. 2D) and showed diffused cytoplasmic positivity to smooth muscle actin (SMA) (Fig. 2E) and desmin (Fig. 2F).
-
Fig. 2 (A) Cellular tumor composed of spindle to oval cells arranged in fascicles (black arrow). (B) Mitotic activity is frequently seen (x20 magnification) (thick blue arrow). (C) Tumor displays coagulative tumor cell necrosis with a sharp interface between viable tumor and non-viable tumor (blue arrow head). (D) Tumor cells (black arrow) are seen to infiltrate through the densely hyalinized dura tissue (blue arrow head). (E) Tumor cells show diffuse cytoplasmic positivity for SMA. (F) Tumor cells show diffuse cytoplasmic positivity for desmin.
Fig. 2 (A) Cellular tumor composed of spindle to oval cells arranged in fascicles (black arrow). (B) Mitotic activity is frequently seen (x20 magnification) (thick blue arrow). (C) Tumor displays coagulative tumor cell necrosis with a sharp interface between viable tumor and non-viable tumor (blue arrow head). (D) Tumor cells (black arrow) are seen to infiltrate through the densely hyalinized dura tissue (blue arrow head). (E) Tumor cells show diffuse cytoplasmic positivity for SMA. (F) Tumor cells show diffuse cytoplasmic positivity for desmin.
Conclusion
Diagnosis of uLMS prior to biopsy remains a challenge. Surgical management in metastatic uLMS with skeletal and dural metastasis and SDH can greatly improve a patient's quality of life although long-term survival has yet to be determined. In our case, resection of the skull and dural lesion together with drainage of the SDH was the best option for the patient as it relieved the patient's symptoms and provided a diagnosis to guide subsequent treatment.
Conflict of Interest
None declared.
Funding None.
References
- Uterine leiomyosarcoma: a review of the literature and update on management options. Gynecol Oncol. 2018;151(3):562-572.
- [Google Scholar]
- Uterine leiomyosarcoma metastasis to the skull–case report. Neurol Med Chir (Tokyo). 1996;36(7):469-471.
- [Google Scholar]
- Skull metastasis from uterine leiomyosarcoma: a case report. Acta Neurol Taiwan. 2006;15(2):109-113.
- [Google Scholar]
- Skull metastasis from uterine leiomyosarcoma, a rare presentation for a rare tumor: a case report and review of the literature. Front Oncol. 2020;10:869.
- [Google Scholar]
- Treatment of skull metastasis from uterine leiomyosarcoma: a single-center experience with literature review. INAT. 2021;23:101004.
- [CrossRef] [Google Scholar]
- Unusual case of skull metastasis from hepatocellular carcinoma. ANZ J Surg. 2004;74(8):710-713.
- [Google Scholar]
- Subdural hematoma secondary to metastatic dural carcinomatosis. Case report. J Neurosurg. 1974;41(5):610-613.
- [Google Scholar]
- Subdural false membrane or haematoma (pachymeningitis interna haemorrhagica.) in carcinomatosis and sarcomatosis of the dura mater. Brain. 1934;57:32-48.
- [Google Scholar]
- Metastatic pattern of uterine leiomyosarcoma: retrospective analysis of the predictors and outcome in 113 patients. J Gynecol Oncol. 2014;25(4):306-312.
- [Google Scholar]
- WHO Classification of Tumours Female Genital Tumours. (5th ed.). Lyon: International Agency for Research on Cancer; 2020. p. :283-285.
- [Google Scholar]







