Translate this page into:
Cerebral Coenurosis Masquerading as Malignancy: A Rare Case Report from India
Address for correspondence: Dr. P. Somashekara Reddy, Sagar Hospital, Tilak Nagar, Jayanagar Extension, Bengaluru - 560 041, Karnataka, India. E-mail: psreddy70@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Human coenurosis is a rare zoonotic disease caused by the larvae of Tinea multiceps seen in sheep-rearing countries. We report the case of a 63-year-old male who was referred to our hospital with a working diagnosis of skull base chondrosarcoma. Histopathological examination after surgical excision revealed characteristic feature of coenurus with multiple scolices invaginating from the outer cuticular layer. Coenuri are often mistaken for giant cysticercal cysts and hydatid cysts. Despite its wide prevalence in cattle, only two cases of human coenurosis are reported from India till date. We report the third case from India.
Keywords
Coenurosis
skull base
Tinea multiceps
INTRODUCTION
Human coenurosis is a rare zoonotic disease caused by the larval stage of taenia species such as Taenia multiceps, T. serialis, T. brauni, and T. glomerata.[1] The infection is common in sheep-rearing countries such as Africa, the Mediterranean, and the Middle East and endemic in Israel.
The lifecycle of this parasite is similar to T. solium and T. saginata, with dogs, coyotes, and foxes being definitive hosts, while rabbits, rodents, sheep, and cows being intermediate hosts.[23] Humans get accidently infected by ingesting food contaminated with the eggs from the definitive or intermediate hosts with cystic larva developing in the central nervous system (CNS), eye, subcutaneous tissue, intramuscular tissue, and abdominal or pericardial cavity.[45] In humans, coenuri produce large giant cysts that are frequently mistaken for giant cysticercal cysts or hydatid cysts and hence are probably underdiagnosed. Coenurosis is often reported in cattle in India.[1]
CASE REPORT
A 63-year-old male was referred to our hospital with complaints of blurring of vision, hearing loss, and trigeminal neuralgia on the left side for 6 months. He was an agriculturist who reared sheep and cattle, in addition to having a pet dog. Examination revealed wasting of the left temporalis muscle and sensory loss in the distribution of the left V1, V2, and V3 divisions of the trigeminal nerve. No other sensory and motor deficits were noted. Hematological, biochemical parameters, chest X-ray, and ultrasonography abdomen did not reveal any abnormalities. Multidetector computed tomography (CT) and magnetic resonance imaging (MRI) with contrast of the brain revealed a large heterogeneously enhancing mass arising from the skull base, predominantly involving the left petro-spheno-clival junction and petrous apex. There was evidence of intracranial extension and infiltration to the surrounding bones [Figure 1]. A diagnosis of chondrosarcoma was considered, and the patient was taken up for surgery. Through a left temporal craniotomy with subtemporal extra and intradural approaches, decompression of the lesion was done. Multiple lytic areas of temporal bone destruction with lesion extending to the infratemporal fossa were noted. The extradural portion was firm and vascular. The intradural portion was soft and avascular with a good plane of cleavage. The resected tissue was submitted for histopathological examination.
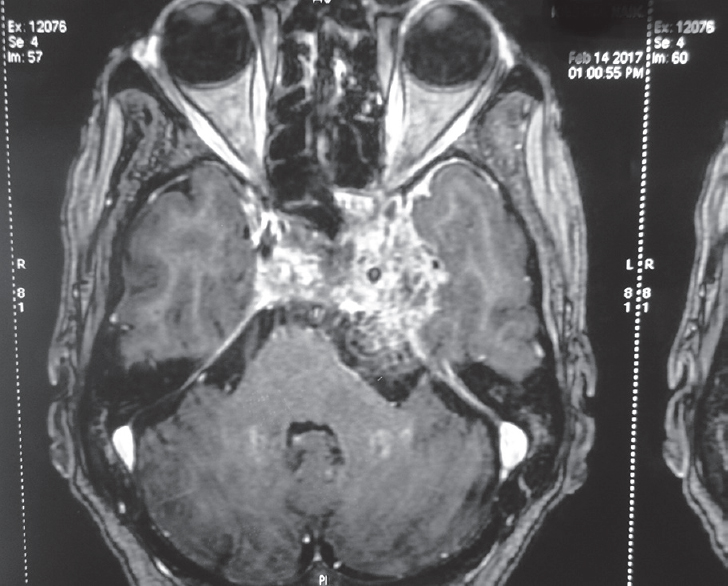
- Multidetector computed tomography with contrast magnetic resonance imaging-heterogeneous lesion arising from the central skull base bones with intracranial extension and infiltration to the surrounding bones
Gross examination revealed multiple pearly-white membranous tissue bits measuring about 3 cm × 2 cm with numerous patches along the surface [Figure 2]. Histological examination revealed a cystic lesion seen as multiple fragments focally seen to be destroying bone [Figure 3]. Each fragment had a villus configuration lined along the outer aspect by a cuticle, which was seen to invaginate internally to produce branching tubular structures. Beneath the cuticular layer was a layer of subtegumental cytons [Figure 4]. The internal aspect of the cyst revealed multiple variably sized protoscolices seen as cavitary spaces lined by the cuticular layer and surrounded by the eosinophilic coagulative proteinaceous fluid filling the cystic cavities. There were multiple protoscolices with extensive hydropic degeneration lacking intact suckers or hooklets. Some of them showed evagination of the neck [Figure 5]. At places, cyst had elicited a mixed inflammatory response reaction and focal giant cell reaction [Figure 6]. No calcification was noted. These histological features were diagnostic of coenurosis caused by T. multiceps.

- Gross: Excised thin membranous cyst wall with numerous small patches along the surface
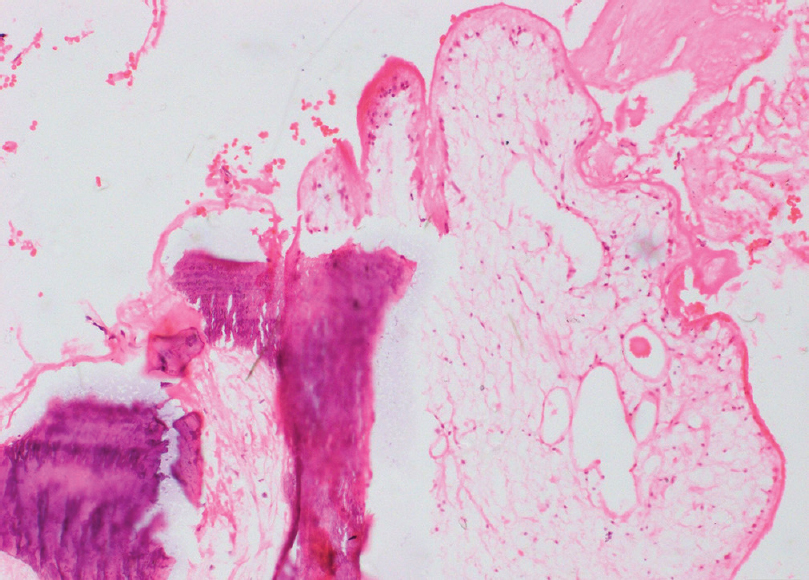
- Cyst destroying the bone (H and E, ×100)
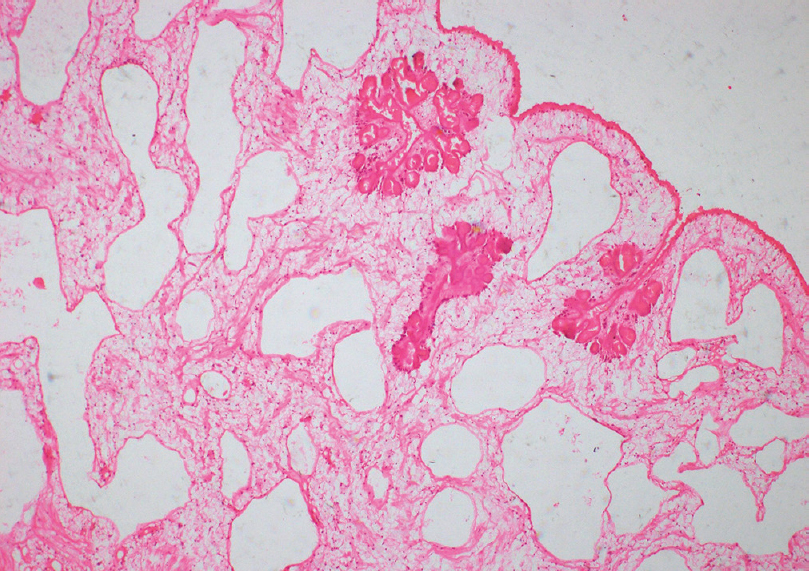
- Coenurus with outer cuticular layer, subtegumental cyton, and invaginating scolices (H and E, ×40)
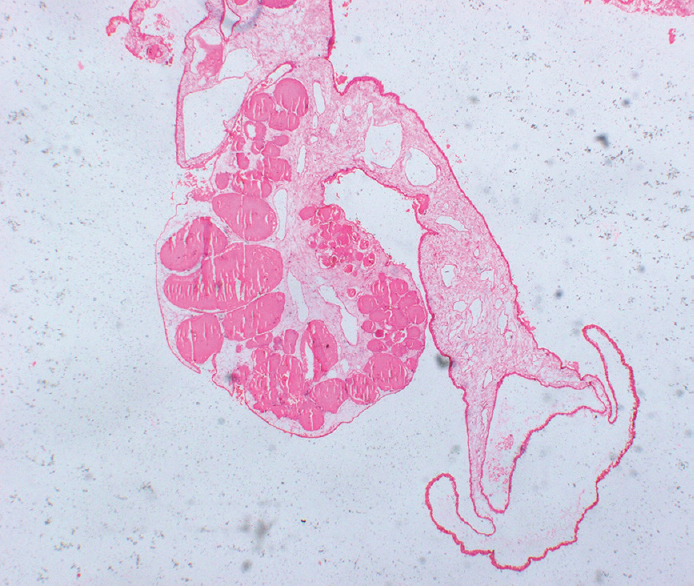
- Larva with evagination of the neck and hydropic degeneration of the scolices (H and E, ×40)
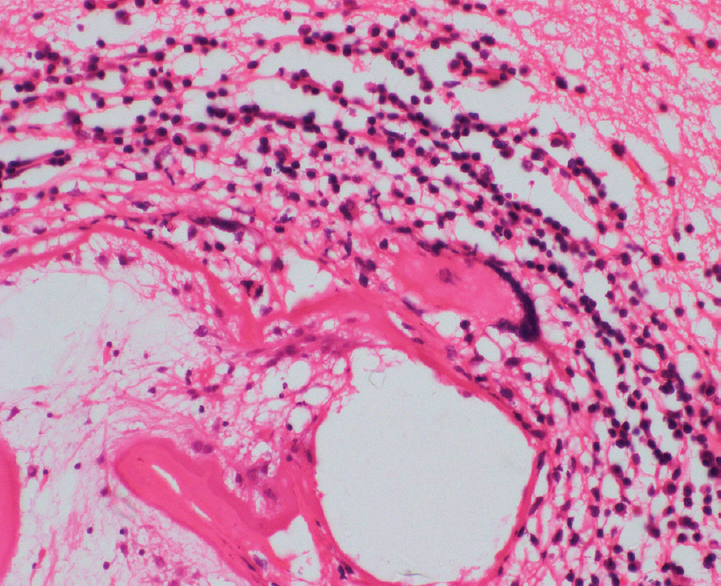
- Mixed inflammatory cell response and giant cell reaction to the cyst (H and E, ×100)
The patient recovered well and was discharged on the 4th-postoperative day. He was reviewed on the 10th day and was put on albendazole for 1 month after the histopathology report.
DISCUSSION
Human coenurosis was first reported by Brumpt in 1913. Most of the cases of human coenurosis are reported from Africa.[3] The parasite is a two-host zoonotic cestode. The definitive host is a carnivore such as dog or fox and intermediate hosts are herbivores that include sheep, rabbits, rodents, and cows. Humans become accidental intermediate hosts by ingesting eggs passed in the excrement of a definitive host through contaminated fruits and vegetables. The ingested eggs release oncospheres in the intestine of the host that penetrate the intestinal wall and pass through the blood stream toward the target organs.[4]
Coenurosis involves CNS, muscle, and subcutaneous tissues in humans, similar to cysticercosis. The clinical features depend on the anatomical area; the larva is lodged. In the CNS, seizures, headache, vomiting, and papilledema are the presenting symptoms. It can also cause cranial nerve palsy, hemiplegia, and paraplegia. Arachnoiditis and ependymitis result from the involvement of the cerebrospinal fluid (CSF) pathways.[5] Our patient presented with visual defects and trigeminal involvement. The parasite can also present as paravertebral mass, subcutaneous cysts, and intraperitoneal disease causing extrinsic biliary compression and obstructive jaundice.[3] Ibechukwu and Onwukeme have reported ocular coenurosis from Nigeria.[6]
Histopathology remains the gold standard for diagnosis. The histopathology of coenuri is similar to other cestodes with an outer cuticular layer and an inner reticular layer. The outer cuticular layer is undulating with microvilli and invaginated to form protoscolices. Protoscolices contain daughter cysts lined by germinal epithelium. The cuticular wall with multiple protoscolices is the characteristic feature of T. multiceps, whereas T. solium has a single scolex. The body wall exhibits myxoid matrix and calcareous bodies, which was not seen in our case. T. multiceps can grow up to 100 cm. The scolex has four cup-shaped suckers and bears a rostellum, which has two rows of birefringent hooklets. The number of hooks in each varies from 22 to 32. Length of large hooks varies from 180 to 190 μm and small hooks 108–126 μm.[4] Differentiation of the species based on microscopy is difficult. Subtyping is based on the rostellar size and numbers, but holds no clinical significance.[1] Cross-reactivity with echinococcal antigen is reported, but no definite serological test is available.[1] Polymerase chain reaction-based restriction fragment length polymorphism to differentiate various species of taenid cestodes appears promising for epidemiological and diagnostic purposes.[3]
On CT, viable cysts are visualized as lucent lesions with rim enhancement. Small cysts can also be easily recognized. Cyst fluid on MRI is of similar intensity as CSF.[3] Our case showed an abnormally heterogeneous enhancing lesion from the skull base with intracranial extension and bone involvement. It was misdiagnosed as skull base tumor-chondrosarcoma probably because of intracranial extension and bony infiltration.
Cysticercosis and echinococcosis are the most common parasitic diseases of the CNS that need to be excluded before coenurosis is considered. These cysts are usually filled with clear fluid. Coenurus cysts are large, white, round, or oval with multiple inverted protoscolices attached to the internal membrane. Cysticercosis is usually 1–2 cm in size with giant racemose forms rarely exceeding 10 cm in size. Hydatid cysts are large and unilocular and have lamellated ectocyst with scolices and daughter cysts floating in the lumen.[1] Sparganosis is not usually cystic and may produce subcutaneous and intracerebral masses.[3] Differential diagnosis also includes other low- and high-grade neoplastic lesions, abscesses, and neuroglia cyst.[7]
Literature search shows only two cases of human coenurosis reported till date from India.[1] The first case reported from India was of a 55-year-old male who presented with progressive weakness of the left upper and lower limbs of 1-year duration along with reduced sensory and visual perception. MRI revealed a large well-defined lesion in the right parieto-occipital region measuring 6.3 cm × 4 cm, hypointense on T1W1 and hypointense on T2. Multpile cysts were seen around the main lesion. The second case was a 36-year-old male who presented with an intractable headache and vomiting of 2 weeks’ duration. Cranial CT scan revealed a well-circumscribed cystic lesion in the left temporal trigonal region causing loculation of the temporal horn of the lateral ventricle. Both were mistaken for hydatid cysts on radiography. They were treated with albendazole following surgery and histopathological examination. They were symptom free on discharge after 2 weeks and on follow-up.
Vaccination with recombinant antigens Tm16 and Tm18 prepared from oncosphere of T. multiceps protected sheep from T. multiceps infection. These developments are hopeful for the development of effective vaccines against cestodes including T. multiceps.[2]
Albendazole alone or combined with praziquantel to prevent dissemination is used. No treatment recommendations are available.[1]
CONCLUSION
This case is reported because of its rarity in India. Despite its wide prevalence in animals, there have been only two cases of human coenurosis reported from India. Awareness of this entity is necessary, as they are misdiagnosed as giant cysticercal cysts or hydatid cysts.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Cerebral coenurosis mimicking hydatid disease – Report of two cases from South India. Clin Neuropathol. 2011;30:28-32.
- [Google Scholar]
- Taenia multiceps: A rare human cestode infection in Israel. Vet Ital. 2008;44:621-31.
- [Google Scholar]
- Human coenurosis in North America: Case reports and review. Clin Infect Dis. 1998;27:519-23.
- [Google Scholar]
- Disseminated human subarachnoid coenurosis: Computed tomographic appearance. AJNR Am J Neuroradiol. 1985;6:638-40.
- [Google Scholar]
- AIRP best cases in radiologic-pathologic correlation: Human coenurosis (Taenia larva) Radiographics. 2012;32:517-21.
- [Google Scholar]






