Translate this page into:
Cerebral and Coronary Vasculature in Disease Associations and Dissociations in the South Indian Population
Address for correspondence: Dr. Sadanandavalli Retnaswami Chandra, Department of Neurology, Faculty Block, Neurocentre, National Institute of Mental Health and Neurosciences, Bengaluru - 560 029, Karnataka, India. E-mail: drchandrasasi@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Cerebrovascular accidents constitute the most common cause of disability all over the world. In India prevalence rate is 545 per 100000 and mortality rate is around 7.5 per thousand. Therefore the authors undertook a study on patients who underwent coronary artery bypass surgery (CABG). They were investigated for clinical and/or radiological evidence of cerebrovascular disease (CVD) with the aim to decide on early neurological intervention.
Patients and Methods:
210 patients who had undergone CABG were evaluated with neck vessel Doppler using high resolution duplex scanner system and computed tomography (CT) scan as well as MR angiogram (MRA) in addition to assessment of co morbid risk factors.
Results:
91% of patients who had undergone CABG had radiological evidence of CVD. The most common risk associated with CAD and CVD was Hypertension (HT), DM, dyslipidemia and combined HT and DM in that order. Neck vessels were normal in 59%. Significant disease was found in only 7.2%. Internal carotids were abnormal in 82%. Infarcts were seen in 82.1%.
Discussion:
This study reveals patients with CAD have a high degree of asymptomatic CVD. It is mostly due to small vessel disease including internal carotids but not so much with large vessels. Therefore, patients with CAD carry a high risk of vascular cognitive dysfunction. This can be reduced by effective management of the systemic risk factors. Screening for large vessel disease which is commonly done is likely to give a false sense of security.
Conclusion:
As against western population Indians seem to have small and medium sized vessels disease in the setting of CAD.
Keywords
Carotids
common features
coronary arteries
vascular cognitive impairment
INTRODUCTION
Coronary artery disease (CAD) and cerebrovascular diseases (CVDs) are diseases due to common pathology causing blockage of blood supply to their respective end organs. Cerebrovascular accidents (CVAs) constitute the most common cause of disability all over the world.[1] In India, prevalence rate is 545/100,000 and mortality rate is around 7.5/1000.[2] However, the process of vascular disease starts much earlier than the symptom comes. Early detection of vascular disease can help in preventive treatments that will salvage the two vital organs involved. However, there is wide variation in the pattern of disease occurrence in different parts of the world. Extracranial carotid artery disease is most common in the west.[3] Both CAD and CVDs are related to alterations in intima-media thickness as per literature.[4] Various risk factors in these disorders have been studied and factors which are modifiable have been looked into.[5] In patients with carotid stenosis of more than 75%, the annual stroke incidence is 1.3%. Therefore, management of asymptomatic carotid artery disease will reduce the incidence of strokes by 0.34%.[6] However, the risk of intracranial atherosclerosis is high in Asians. Patients who have stenosis of more than 50% in the intracranial vessels carry a 40% risk of stroke in the next 2 years.[7] The small vessels of brain constitute the penetrating branches of cortical vessels which are about 70–80 μ and capillary networks of brain in human beings which are about 8–10 μ in diameter. Artery-to-artery communication is limited to vessels smaller than 20 μ.[8] When mean arterial pressure increases, the diameter of vessels becomes smaller and blood flow remains constant despite changes in perfusion pressure by virtue of this autoregulation. Vasa nervorum of the larger blood vessels also probably have a role. Cerebrovascular (CV) resistance is a mathematical concept derived from perfusion pressure and blood flow and influenced by intracranial pressure (ICP), viscosity, etc. In ischemic vessels, autoregulatory response is not seen, and therefore, diameter does not change with change in blood pressure or PCO2, and passive dependence on perfusion pressure occurs. Paradoxical responses such as decreased flow with high PCO2 and increased perfusion pressure can occur when ICP is increased. Prognosis depends on the degree of small vessel disease (SVD). Therefore, integrity of the small vessels should be ensured before attempting any intervention for incidental large vessel disease (LVD) identified. We analyzed the incidence of neck vessel disease and CVD in both symptomatic and asymptomatic in patients who underwent coronary artery bypass surgery (CABG) patients to identify CV risk factors in these patients and probable methods to prevent vascular cognitive impairment. Literature reports double the risk of dementia in post-CABG patients in 6-year follow-up as compared to non-CABG patients.[9]
Heart–brain interaction in vascular pathology
About 1% of patients with strokes suffer myocardial infarction (MI) during acute stroke presentation, and strokes themselves can affect the heart in older persons in the form of tall T-waves and QT changes and are considered as bad prognostic markers. No cardiac history is obtained in approximately 70% of patients with CV.[1011] However, unrecognized heart disease is reported in 50% patients with CVA and of this significant heart disease of which 30% is overt and 15%–20% is latent. On the other hand, cardiac disease as the cause of stroke is generally considered as cardioembolic due to intracardiac clots, arrhythmias, etc. There are therapeutic decision-making issues in patients with non-ST elevation MI. These patients need catheter-based treatment for cardiac management, and the MATCH study revealed compared to clopidogrel alone that addition of aspirin increases the risk of life-threatening intracranial bleeds by 3% with very marginal protection. Because of shared risk factors, CVD and CADs often coexist and early recognition can help in improving the quality of life in patients with this concurrent comorbidity. Apart from assessing cardiac disease in patients with CVA, it is worth looking for CV and peripheral vascular pathology in patients with CAD.[12] This study indicates need for looking for SVD and intracranial medium-sized vessel disease than looking for disease of neck vessels, especially in Asians.
Patients and Methods
A cross-sectional descriptive study of 210 patients who underwent CABG in Madurai Apollo Hospital and Sri Ramachandra Medical Centre, Chennai, for 1 year between November 1998 and November 1999 were evaluated after proper informed consent and institutional ethical approval. All patients above 40 years who underwent CABG and willing to undergo the assessment were included in the study. The patients underwent thorough clinical examination, demographic details, complete blood counts, blood sugar glycated hemoglobin (HBA1c), lipid profile, renal and liver function tests, and electrolytes. The presence of high-density lipoprotein <40 mg/dl and low-density lipoprotein >130 mg/dl was considered dyslipidemic and HBA1c >6 as hyperglycemic. The criteria for high blood pressure were as recommended by the Joint National Committee V1 and V11, diabetes mellitus (DM) as defined by the WHO criteria and dyslipidemia as per the NIH, USA Guidelines. Other risk factors which were assessed with oral questioning were alcohol, smoking, and family history. They all underwent magnetic resonance imaging (MRI) of the brain with 1.5 Tesla machine T1, T2, T2-fluid-attenuated inversion recovery, magnetic resonance angiography (MRA), neck vessel Doppler for four vessels with plaques, and stenosis assessment as well as computed tomography scan in most patients. Data were entered into Excel Sheet and descriptive statistics was applied with IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. Degree of occlusion was measured visually; LVD involving extracranial and intracranial vessels was assessed; and large artery infarcts, SVD, and mixed LVD and SVD were categorized. The Fazekas scale is used to quantify the amount of white matter T2 hyperintense lesions usually attributed to SVD.
-
Periventricular white matter
0 = Absent
1= “Caps” or pencil-thin lining
2 = Smooth “halo”
3 = Irregular periventricular signal
-
Deep white matter
0 = Absent
1 = Punctate foci
2 = Beginning confluence
3 = Large confluent areas.
RESULTS
There were a total of 210 patients who underwent CABG comprising 161 males and 49 females. Their mean age was 55.8 ± 12.1 years [Table 1].
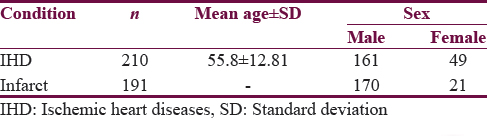
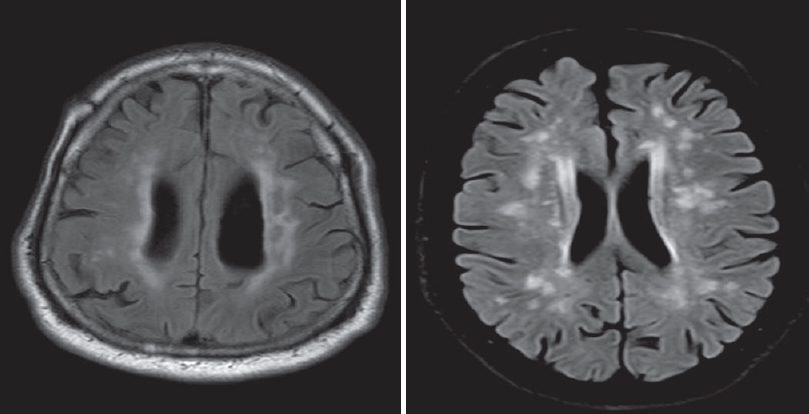
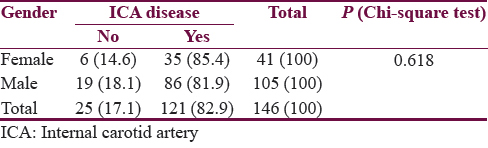
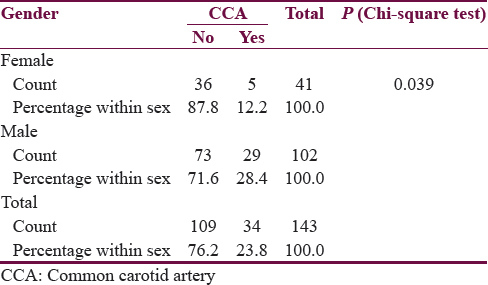
Risk factors among CABG patients are enclosed in Tables 2 and 3. No risk factor was identified in 20% patients. Only 4% patients were smokers in this group. DM was seen in 11% and hypertension (HT) in 19%. Combined DM and HT was seen in 37%. Dyslipidemia was seen in 57%. Maximum number of patients who had CVD also had both DM and HT. Right-sided weakness was seen in 41% of patients, left-sided weakness was seen in 35% patients, posterior circulation strokes were seen in 12%, and lacunar lesions were seen in 12%. Neck vessel Doppler revealed normal vessels in 59%. There were significant disease in 7.2% and nonsignificant disease in the rest [Figure 1]. MRI revealed cerebral SVD [Figure 2]. Figure 3 shows asymptomatic intracranial middle cerebral artery occlusion and large vessel infarct. Out of total 210 patients, 191 patients with CABG showed varying degrees of both symptomatic and asymptomatic CVD. However, the extracranial vessels were normal in 59% as per Doppler study and the rest showed some evidence of atherosclerosis. Significant occlusion of extracranial vessels was seen only in 7.2% of patients. MRA revealed completely normal neck vessels in 64 persons out of 210, and combined common carotid and left or right internal carotid artery (ICA) disease was seen in 36 and 35 persons, respectively. Other regions were involved infrequently. Sensitivity of MRA is probably better than Doppler in picking up minor disease. It was observed that changes in ICA were associated with the evidence of cerebral vascular changes than in patients who showed evidence of LVD. Male gender seems to have more evidence of CVD than female.

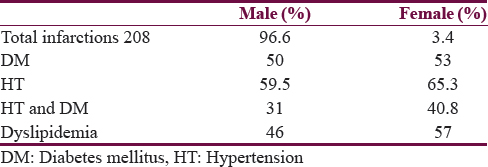
- Cerebral small vessel disease

- Right middle cerebral artery occlusion
- Rare occurrence of large vessel disease
In patients with CABG and CVD, the most common risk factor seems to be HT, DM, their combined occurrence, and dyslipidemia. There is a very high occurrence of CVD in patients who suffer from CAD, both symptomatic and asymptomatic. In this study, maximum abnormality is found in intracranial medium-sized vessels and small vessels and only rarely the large vessels. Extracranial neck vessels are very rarely involved in these patients. Females and males carry the same degree of risk of SVD with reference to brain and probably a increasing trend toward CAD in postmenopausal age group in females, and males carry greater risk of LVD [Table 4]. The total number of females in the whole study is very less as compared to males and needs to be studied in a larger population with equal gender distribution. Major neck vessel showed males more affected than females even though the total number of significant neck vessel disease was small in both groups.
DISCUSSION
The cause of CVD in these patients is mostly due to cerebral SVD. Maximum risk for CAD is dyslipidemia and the second common cause is combined DM and HT. In patients with CVD, maximum patients belong to group of combined DM and HT group. Therefore, this study reveals that the most common CV event in patients who have undergone CABG is SVD which is a major risk for vascular cognitive impairment and the best strategy to prevent is effective management of the risk factors and other interventions are very rarely indicated.
CONCLUSION
Carotid artery disease and CAD are closely linked. Both can be silent or symptomatic. We have larger carotids and smaller coronaries, and this study reveals that both symptomatic and asymptomatic strokes are common in patients with CAD, but abnormality in major vessels is seen in only <7.2%, indicating that they are mostly related to SVD in India as against the west. Therefore, CAD is a major risk indicator of cerebral SVD and vascular cognitive decline and less often major vessel disease.
SVD behaves differently from LVD in the following ways. SVDs behave as progressive frontal lobe syndrome resembling degeneration with executive function dysfunction, whereas an LVD presents with acute-onset and step-like course. Neuropsychologically, SVD shows executive function involvement, whereas in LVD, the defect is based on the region involved and treatment options are based on the window period and risk factors, whereas in SVD, it is risk management and cognitive enhancement, and thus, these two types of vascular insults have entirely different clinical features, course, outcome, and treatment options, which make the information conveyed through the paper very relevant.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Department of Cardiology, Apollo Hospital, Madurai, and Sri Ramachandra Medical Centre, Chennai, South India. We acknowledge with gratitude for permission given to utilize their post coronary artery bypass surgery patients for the study.
REFERENCES
- Correlation of intracranial atherosclerosis with carotid stenosis in ischemic stroke patients. Ann Indian Acad Neurol. 2015;18:412-4.
- [Google Scholar]
- Prevention of coronary heart disease in clinical practice. Summary of recommendations of the Second Joint Task Force of European and other Societies on coronary prevention. The Eur J Gen Pract. 1999;5:154-61.
- [Google Scholar]
- Arterial wall thickness is associated with prevalent cardiovascular disease in middle-aged adults. The Atherosclerosis Risk in Communities (ARIC) Study. Stroke. 1995;26:386-91.
- [Google Scholar]
- Relation of intima-media thickness to atherosclerotic plaques in carotid arteries. The Vascular Aging (EVA) Study. Arterioscler Thromb Vasc Biol. 1996;16:310-6.
- [Google Scholar]
- Asymptomatic carotid stenosis: Identifying patients at high enough risk to warrant endarterectomy or stenting. Stroke. 2014;45:655-7.
- [Google Scholar]
- Small vessels of the central nervous system: Physiology and pathophysiology. In: Hilal SK, ed. Small Vessel Angiography: Imaging, Morphology, Physiology, and Clinical Applications. St. Louis: Mosby; 1973. p. :207-18.
- [Google Scholar]
- Evaluation of the novel factor Xa inhibitor edoxaban compared with warfarin in patients with atrial fibrillation: Design and rationale for the Effective aNticoaGulation with factor xA next GEneration in Atrial Fibrillation-Thrombolysis In Myocardial Infarction study 48 (ENGAGE AF-TIMI 48) Am Heart J. 2010;160:635-41.
- [Google Scholar]
- Cardiac autonomic derangement and arrhythmias in right-sided stroke with insular involvement. Stroke. 2004;35:2094-8.
- [Google Scholar]
- Coronary, peripheral and cerebrovascular disease: A complex relationship. Herz. 2008;33:475-80.
- [Google Scholar]






