Translate this page into:
Candida albicans spondylodiscitis in an immunocompetent patient
Address for correspondence: Dr. Tapan N Joshi, Department of Spinal Cord Injury, VA Central Iowa Healthcare System, 3600, 30th Street, Des Moines, IA 50310, USA. E-mail: tapan.joshi@va.gov
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Spondylodiscitis is a condition that involves extradural components of the spine. Its non-pyogenic etiologies include fungal infection which is mainly caused by Candida albicans. Candidemia and resultant deep-seated infections are frequent in immunocompromised patients.[1] Here, I would like to present a case of candida spondylodiscitis (CSD) in a non-immunocompromised subject.
A 63-year-old man with a history of COPD, hepatitis C and chronic alcoholism underwent a scheduled vascular surgery. Post-operatively, he was admitted in the ICU for delirium for 2 weeks where a central venous catheter was placed. Upon discharge, he resumed his light duty work. Four weeks later, he started having low back pain after lifting his toddler son. He was treated symptomatically by emergency room physicians for 1 month and ultimately was referred to the outpatient clinic. He complained about low-grade continuous, non-radiating low back pain. He denied fever or malaise. Upon physical examination, he had tenderness over the T8-9 level with an apparent kyphotic deformity, but his neurological exam was normal. Laboratory tests were normal except elevated ESR and showed no immunosuppression. Thoracic spine radiographs revealed acute compression fractures of vertebral bodies at T8, T9 levels. CT-scan and later, MRI confirmed spondylodiscitis [Figures 1 and 2]. The CT-guided biopsy revealed Candida albicans infection. He was started on caspofungin for 7 days followed by fluconazole treatment for 6 months until he had clinical resolution with normalization of ESR.
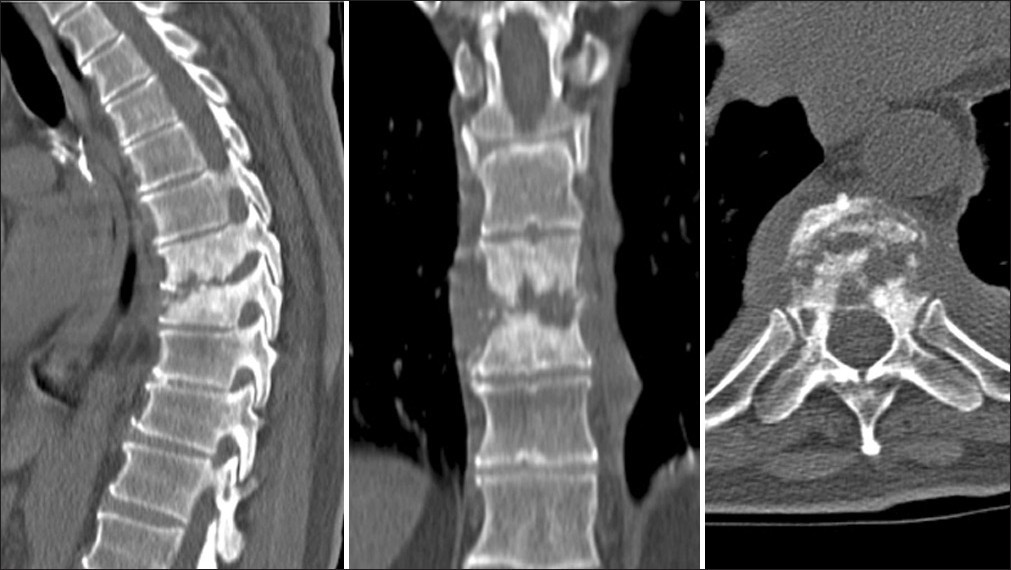
- Sagittal, coronal, and transverse views of the CT scan show the extent of bone fragmentation and sclerosis
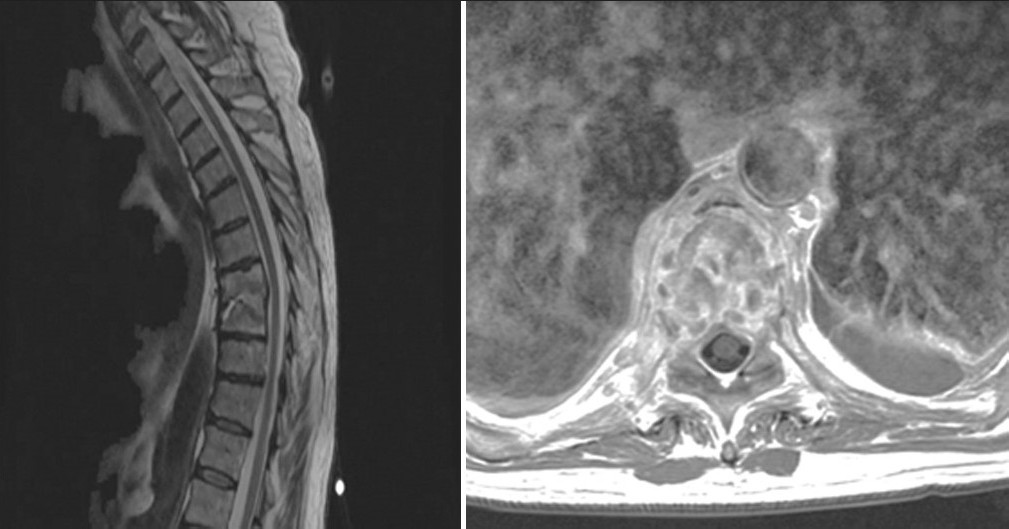
- Magnetic resonance imaging of thoracic spine with contrast shows involvement of T8, T9 vertebral bodies with associated pre-vertebral soft tissue inflammation
CSD is possible in immunocompetent subjects with well-defined risk factors. The risk factors include illicit intravenous drug abuse, alcoholism, diabetes, central venous catheters, parenteral feeding, prolong antibiotic use, and post-spinal surgery.[23] In the present case, our patient had two risk factors, i.e. chronic alcoholism and central venous catheterization. The low virulence of the pathogen and poor vascularization of the disc space make CSD, a sub-acute condition with vague symptoms. It may take a few weeks to months to cause extradural involvement.[1] It usually involves lower thoracolumbar spine like in our case. Common symptoms are back pain, anorexia, fever (32%-48%), and neurological deficit (~20%).[24] A patient may not have a history of candidemia and laboratory data can be non-specific.[2] Insidious progression of infection with non-specific symptoms and laboratory data constitute a diagnostic problem for a clinician especially in non-immunocompromised subjects. Therefore, knowledge of risk factors is imperative which leads to early diagnosis of CSD. MRI is a sensitive and specific modality for early detection.[1] It may show vertebral bodies involvement with endplate destruction, loss of disc space as well as associated pre-vertebral soft tissue inflammation without spinal cord compression. As compared to pyogenic infection, in CSD mostly one level is affected and incidence of paraspinal inflammation is less common than tuberculosis though above described findings may be absent.[5] Therefore, a biopsy is necessary to confirm the diagnosis.[1] The treatment guidelines for CSD are based on treatment protocols for candidemia using isolated or combination of antifungal medications. A reasonable strategy is to treat with intravenous therapy followed by oral medication. Treatment should be continued until resolution of clinical symptoms and inflammatory changes on imaging studies as well as normalization of laboratory data.[2] Successful outcomes have been achieved with amphotericin B or fluconazole. Indications for surgical intervention are neurological compromise, spinal instability, and medically refractory infection.[1–3]
CSD in immunocompetent patients has a good outcome if early diagnosis is made.[2] A high index of suspicion and knowledge of risk factors are helpful for early diagnosis.
Acknowledgment
This case was moderated at ‘The 2010 Annual Meeting of the Academy of Spinal Cord Injury Professionals’ at Las Vegas, Nevada, U.S.A. September 22-24, 2010.
References
- Vertebral osteomyelitis due to Candida species: Case report and literature review. Clin Infect Dis. 2001;33:523-30.
- [Google Scholar]
- Fungal spinal osteomyelitis in the immunocompromised patient: MR findings in three cases. Am J Neuroradiol. 1999;20:381-5.
- [Google Scholar]





