Translate this page into:
Blind after first chemotherapy
*Corresponding author: Josef Finsterer, Department of Neurology, NNC, Vienna, Austria. fifigs1@yahoo.de
-
Received: ,
Accepted: ,
How to cite this article: Finsterer J. Blind after first chemotherapy. J Neurosci Rural Pract. 2024;15:393-5. doi: 10.25259/JNRP_568_2023
Dear Sir,
Chemotherapy is not without side effects. The most common side effects are fatigue, hair loss, mouth and throat sores, diarrhea, constipation, nausea and vomiting, and low blood counts.[1] These side effects usually improve with a lower dose of chemotherapy or after chemotherapy is stopped. Less commonly, chemotherapy can cause serious central nervous system (CNS) side effects including seizures, syndrome of inappropriate antidiuretic hormone (SIADH) secretion, vision loss, taste loss, hearing loss, and memory impairment.[2] There is controversy about whether chemotherapy also increases the risk of stroke. Some studies found that chemotherapy did not increase the risk of stroke,[3] whereas other studies found a clear significantly increased risk of stroke with chemotherapy.[4,5] There have been no reports of ischemic stroke resulting in temporary complete loss of vision within 24 h of chemotherapy.
The patient is a 77-year-old male, who noticed bilateral vision loss when he woke up the next morning after his first round of chemotherapy for a recently detected cardia carcinoma. After a few hours, vision steadily returned, and after two days, he had regained his previous visual acuity. Chemotherapy included oxaliplatin (150 mg intravenously), docetaxel (86 mg intravenously), and fluorouracil (4.5 mg intravenously) and was well tolerated during infusion.
His past medical history was positive for surgery for a left inguinal hernia and a right clavicle fracture. He never smoked, was not an alcoholic, and did not take medications regularly. He had been suffering from progressive dysphagia for two months before chemotherapy. During the workup, a stenosing cardia carcinoma was discovered. After dysphagia culminated in complete inability to swallow liquids or solid foods, a percutaneous endoscopic gastrostomy (PEG) was implanted.
Examination for visual loss revealed multilocular, small, cortical and subcortical, subacute ischemic lesions of both occipital lobes and a subacute left cerebellar infarction [Figure 1]. The clinical neurological examination two days after the onset of temporary blindness was completely normal as were the ophthalmological and cardiological examinations including telemetry, echocardiography, and 24 h blood pressure monitoring. Blood tests revealed elevated CRP levels and slightly elevated liver transaminases, which were due to tumor or hepatotoxicity of the chemotherapeutic drugs used. The clotting was normal. Acetylsalicylic acid and a change in chemotherapy were recommended.
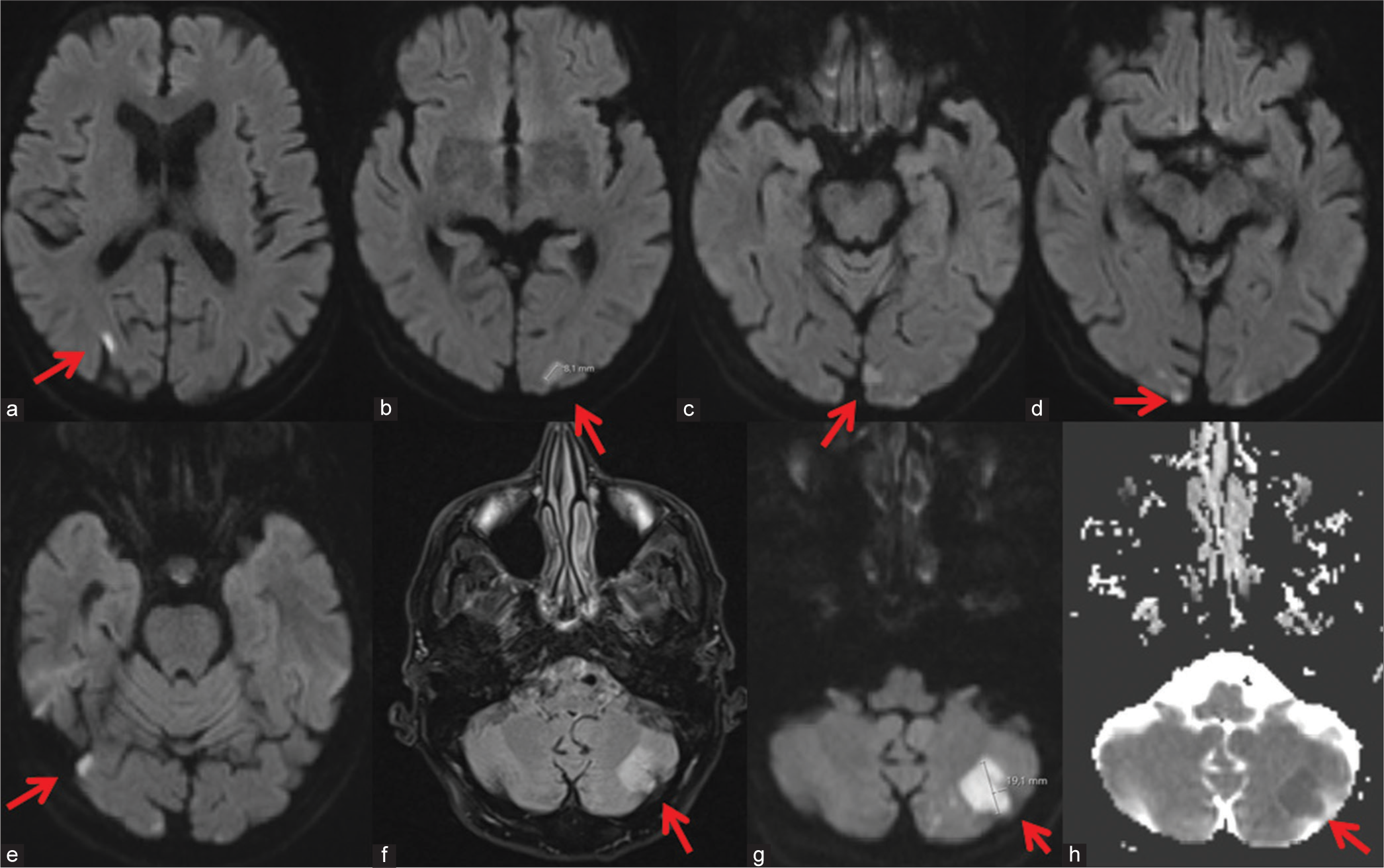
- Cerebral magnetic resonance imaging diffusion-weighted images (DWIs), showing patchy, multilocular hyperintensities in the occipital cortex bilaterally (red arrows). There was also a DWI hyperintense and apparent diffusion coefficient hypointense lesion in the left cerebellum, which was already hyperintense on fluid-attenuated inversion recovery (red arrows).
The study is of interest because oxaliplatin, docetaxel, and fluorouracil in combination have not previously been reported as a cause of ischemic stroke and the index patient did not have classic cardiovascular risk factors but still suffered an ischemic stroke. This suggests that either transient illnesses predisposing to ischemic stroke occurred or chemotherapy toxicity was the cause. Although transient factors such as heart failure, atrial fibrillation, malignant ventricular arrhythmias, pulmonary embolism, thrombophilia or desiccosis could have been causative factors, these conditions were considered unlikely, as follow-up examinations for cardiovascular and other risk factors for ischemic stroke were completely negative.
The first argument for chemotherapy-associated neurotoxicity is the close temporal connection between the first chemotherapy and the occurrence of an ischemic stroke. A second argument for chemotherapy-related toxicity is that chemotherapy-related strokes have been previously reported. Several cases of fluorouracil-associated ischemic stroke have been published.[4] Oxaliplatin is also known to be able to trigger at least stroke-like events.[5] Ischemic stroke has also been reported in a single patient receiving docetaxel for oral squamous cell carcinoma. The stroke in the index patient could also have been a paraneoplastic phenomenon due to increased thrombogenicity. However, all coagulation parameters tested were within the normal range.
In summary, this case shows that chemotherapy with oxaliplatin, docetaxel, and fluorouracil can be complicated by acute ischemic stroke with bilateral vision loss. Although the cardiovascular profile of the index patient was negative, it cannot be ruled out that a transient onset of cardiovascular disease or a paraneoplastic phenomenon was a causative factor.
Author’s contributions
JF: Design, literature search, discussion, first draft, critical comments, final approval.
Data availability statement
Data that support the findings of the study are available from the corresponding author.
Compliance with ethics guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Ethical approval
The research/study approved by the Institutional Review Board at NNC, dated 25.9.2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The most common side effects experienced by patients were receiving first cycle of chemotherapy. Iran J Public Health. 2018;47:1218-9.
- [Google Scholar]
- Mechanisms of chemotherapy-induced neurotoxicity. Front Pharmacol. 2022;13:750507.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of chemotherapy on stroke risk in cancer patients. Thromb Haemost. 2020;120:714-23.
- [CrossRef] [PubMed] [Google Scholar]
- 5-Fluorouracil associated neurovascular toxicities. Curr Probl Cancer. 2021;45:100746.
- [CrossRef] [PubMed] [Google Scholar]
- Unusual stroke-like symptoms with oxaliplatin use. J Oncol Pharm Pract. 2023;29:1766-9.
- [CrossRef] [PubMed] [Google Scholar]





