Translate this page into:
Bladder distension: An unusual cause of reflux of blood and hemodynamic changes (autonomic dysreflexia) during endovascular coiling
Address for correspondence: Dr. Daljit Singh, Department of Neurosurgery, 529, Academic Block, GB Pant Hospital, New Delhi – 110 002, India. E-mail: drdaljit@hotmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Autonomic dysreflexia due to distended bladder is well known. Reflux of blood during endovascular procedure is also a common observation. It happens due to difference in pressure gradient between arterial pressure and that of infusing solution. Generally it happens when the infusion bottle is empty or the pressure in infusion bottles fall. We present an uncommon situation where distended bladder mechanically resulted in reflux of blood into endovascular catheters as well as alteration in hemodynamic parameters. Both settled once the bladder was empty.
Keywords
Aneurysm
coiling
dysautonomia
reflux
Introduction
Hemodynamic changes due to distended bladder are well known. Such changes are referred as part of autonomic dysreflexia (AD) or hyper reflexia. It can even occur during surgery; however, we present an interesting case where AD happened with non-flow of infusion saline in arterial circulation despite high infusion pressure.
Case Report
A 45-year-old male presented with sudden onset headache and altered sensorium. On arrival, his Glasgow coma score was E4M5V4. His pulse was 65/minute. Blood pressure (BP) was 126/76 mmHg. Plain computed tomography of the head revealed blood in left Sylvain cisterns suggestive of subarachnoid hemorrhage. Four-vessel angiogram revealed 6-mm aneurysm in left middle cerebral artery bifurcation.
Patient was taken up for endovascular coiling on first available operation theatre, i.e., 3 days after admission under general anesthesia. His groin was cleaned and draped. The entire body was covered with sterile gown. His BP at induction was 120/76 mmHg and pulse 76/minute. General anesthesia was maintained as per standard protocols. The femoral artery was punctured with 6-French (F) check flow. The angiogram was performed with standard techniques using 6-F angiocatheter. Pressure cuff was applied on the infusion vac and a pressure of 250 mmHg was maintained on the pressure bag to allow easy flow of heparinised saline. A microcatheter (prowler 14) was put for selective catheterization of middle cerebral artery. While negotiating microcatheter, the BP shot up to 200/110 mmHg and pulse was 100/minute. Patient was, however, in deep anesthesia. At this stage of the procedure, the flow of saline solution stopped despite a pressure of 250 mmHg in infusion chamber. There was reflux of blood via the 6-F catheter back into the irrigating arterial tubing despite a constant pressure of 250 mmHg on the fluid bags. There was no evidence of intraoperative rupture of aneurysm during procedure. For about 20 minutes the attempts to control the BP with Diltizam (5 mg) and propofol failed and BP remained on higher side (200/110 mmHg). His arterial blood gases were within normal limits.
The reflux of blood back from femoral artery into the intra-arterial lines resulted in halting of the procedure.
At this stage surgeon noticed grossly distended abdomen and suspected a full bladder. The urine bag was empty. The tubing of Foleys catheter was found to be kinked. The tubing was repositioned, which resulted in bladder empting and settling of BP and pulse.
The reflux of blood also settled and coiling of the aneurysm was successfully completed. Patient was discharged on fourth postop day in satisfactory condition.
Discussion
Rupture of aneurysm results in subarachnoid hemorrhage with high degree of morbidity and mortality. The surgical treatment of aneurysm is either clipping or coiling. Coiling of aneurysm is becoming the more popular method of treatment of rupture aneurysm.[1] Most of the endovascular coiling are done under general anesthesia so that the patient does not move the head. Any shake in the body can impair the road map picture which forms the basic guide for the proper procedure.
The coiling also requires a meticulous control of pulse and BP in right plane of anesthesia.[2] The autonomic responses, e.g., increase in BP and changes in pulse rate can be due to lighter plane of anesthesia, intraoperative rupture of aneurysm, some drug reaction, or thromboembolic episodes during surgery.
In neurosurgical practice, AD is mostly noticed in spinal fracture. Hypertension responses are elicited with somatic stimulation above the lesion, and the response may require aggressive pharmacologic management.[3] Beside full bladder, the other causes of AD are bladder infection, severe constipation, loaded colon, or pressure sores.[4]
Nociceptive stimulations from the bladder add to hypertension.[5] Experimental results using the rat urinary bladder distension model demonstrated the role of the analgesics (morphine, U50,488, and mexiletine) in the inhibition of visceral nociceptive transmission.[6]
Higher incidence of symptomatic AD is reported in subjects using reflex voiding and in those using manual removal of stool. By contrast, the lowest incidence of symptomatic AD was in those on continent spontaneous voiding and continent spontaneous defecation.[7]
The symptoms that occur with AD are directly related to the types of responses that happen in the sympathetic and parasympathetic nervous systems.[89]
Serotonergic and noradrenergic facilitation are also believed as mechanism of AD.[10] During an episode of AD, a significant increase in visceral sympathetic activity with coronary artery constriction can result in myocardial ischemia, even in the absence of coronary artery disease.[11]
The other suggests that glutamate transferase (GLT-1) overexpression attenuates the visceromotor response to bladder distension and both local irritant-induced and cross organ-sensitized visceromotor response to bladder distension due to overexpression of the astrocytic glutamate transporter (GLT-1).[12]
Other observations support the concept that ganglionic acertyl choline resistant (AChR) antibodies are diagnostically and pathophysiologically important. Patients with orthostatic hypotension and prominent cholinergic dysautonomia are most likely to be seropositive for ganglionic AChR antibody.[13]
The salient feature of autonomic changes in our case was its association with reflux of blood into the arterial lines. Both these findings were refractory to medical management. The BP was not settling and tachycardia was persistent.
Association of reflux of blood back into arterial line under infusion pressure of 250 mmHg and autonomic changes were rather peculiar. It is well known that the filled bladder can result in reflex increased in intra-aortic pressure. However, in our case the intra-arterial pressure was 200/110 mmHg which was about 50 mm less than the pressure in the infusion vac. The pressure gradient across the infusion saline and BP was enough to allow the flow of the saline into the arterial line. The reflux of blood therefore cannot be explained due to distended bladder alone. The hemodynamic changes, e.g., increase in BP and tachycardia was due to AD. The mechanism that led to reflux could be due to the direct pressure of distended bladder on the aorta or at femoro-aortic junction resulting in direct compression and king in angiocatheters [Figures 1 and 2] against bony vertebral body. Both hemodynamic changes and reflux settled immediately once the bladder was empty.
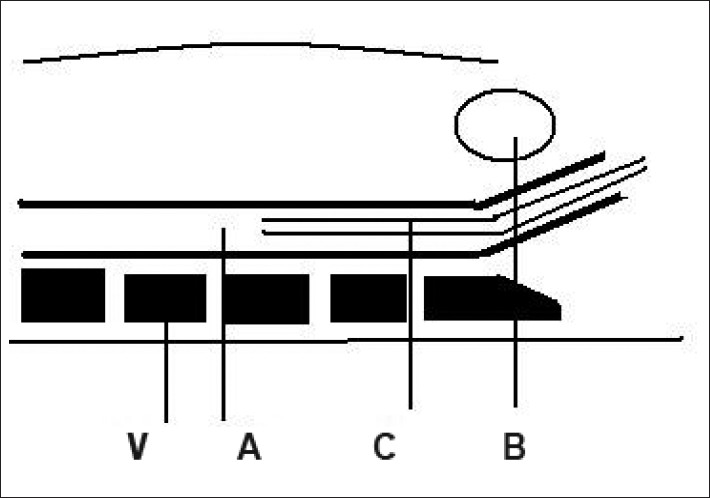
- Schematic representation of the procedure. Note the relationship of aorta and catheter within it and empty bladder
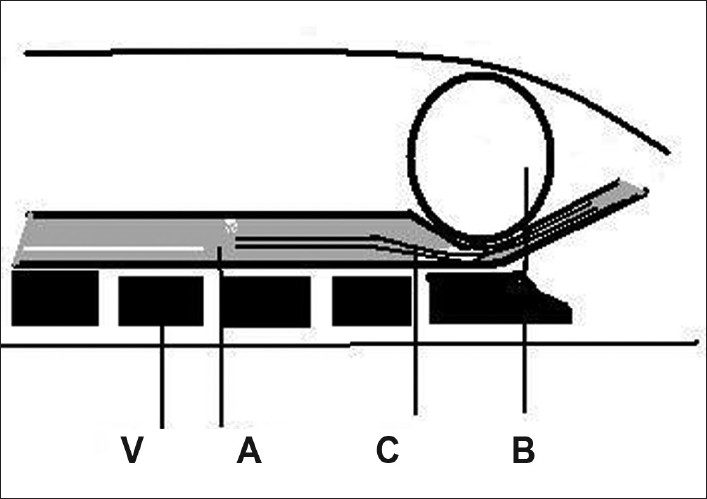
- Schematic representation of filled, distended bladder causing mechanical compression on aorta and catheter against bony vertebral columns resulting in kink, V, vertebral body; A, aorta; C, angiocatheter; B, urinary bladder
Conclusions
The autonomic changes due to filled bladder can result in increase in BP and tachycardia. To settle these changes, it may lead to use of drugs during surgery. However, a careful clinical inspection of the status of urine bag can avoid the use of unnecessary medication, compressions on arterial system, and angiocatheter resulting in backflow of arterial blood into arterial lines.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Impact of International Subarachnoid Aneurysm Trial results on treatment of ruptured intracranial aneurysms in the United States. J Neurosurg. 2011;114:834-41.
- [Google Scholar]
- Aneurysmal subarachnoid haemorrhage and the anaesthetist. Br J Anaesth. 2007;99:102-18.
- [Google Scholar]
- Autonomic dysreflexia-like syndrome in a T12 paraplegic during thoracic spine surgery. Anesth Analg. 2010;111:1290-2.
- [Google Scholar]
- Autonomic dysreflexia as a complication of a faecal management system in a man with tetraplegia. J Spinal Cord Med. 2010;33:266-7.
- [Google Scholar]
- Characterization of pressor and visceromotor reflex responses to bladder distension in rats: Sources of variability and effect of analgesics. J Urol. 2001;165:968-74.
- [Google Scholar]
- Pharmacologic evaluation of pressor and visceromotor reflex responses to bladder distension. J Neurourol Urodyn. 2008;27:249-53.
- [Google Scholar]
- Incidence of symptomatic autonomic dysreflexia varies according to the bowel and bladder management techniques in patients with spinal cord injury. Spinal Cord. 2011;49:49-54.
- [Google Scholar]
- Effects of distension of the urinary bladder on the cardiovascular reflexes from the carotid baroreceptors in the dog. J Physiol. 1993;463:545-64.
- [Google Scholar]
- Cardiovascular sensory receptors and their regulatory mechanisms. Indian J Physiol Pharmacol. 2003;47:124-46.
- [Google Scholar]
- Serotonergic and noradrenergic facilitation of the visceromotor reflex evoked by urinary bladder distension in rats with inflamed bladders. Neurosci Lett. 2008;442:253-6.
- [Google Scholar]
- GLT-1 over-expression attenuates bladder nociception, and local/cross-organ sensitization of bladder nociception. Am J Physiol Renal Physiol. 2011;300:F1353-9.
- [Google Scholar]
- Idiopathic autonomic neuropathy: Comparison of cases seropositive and seronegative for ganglionic acetylcholine receptor antibody. Arch Neurol. 2004;61:44-8.
- [Google Scholar]






