Translate this page into:
Bilateral ptosis without upward gaze palsy: Unusual presentation of midbrain tuberculoma
Address for correspondence: Dr. Chaitali Patra, 40/8, Nabanari Tala 1st Bye Lane, Buxarah, Howrah - 711 110, West Bengal, India. E-mail: chaitalipatra2009@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Central nervous system tuberculoma can have variable presentations depending on the site and number of tuberculomas. We are reporting a rare case of an 11-year-old male child presenting with ptosis and ataxia. Clinical examination revealed bilateral partial 3rd cranial nerve palsy (ptosis without any upward gaze palsy) associated with dysdiadochokinesia and ataxia on the right side. Magnetic resonance imaging of the brain revealed a single ring-enhancing lesion in the dorsal midbrain with perifocal edema. Magnetic resonance spectroscopy provided the etiological information as tuberculoma.
Keywords
Ataxia
magnetic resonance spectroscopy
midbrain
ptosis
tuberculoma
Introduction
Tuberculosis (TB) is still an important public health problem in the developing countries with constant endemicity. It accounts for about 40% of all the intracranial space-occupying lesions (SOLs). Isolated brainstem tuberculoma is a comparatively rare entity with only 5-10% incidence among them.[12] Here, we report a case of an 11-year-old male child presenting with bilateral ptosis and right-sided ataxia, ultimately diagnosed to have midbrain tuberculoma by magnetic resonance spectroscopy (MRS).
Case Report
An 11-year-old male child presented with a history of drooping of both the eyelids for 5 days with associated headache and ataxia for 2 days. He had no history of fever, convulsion, or loss of vision. There was a history of contact with a case of TB in the neighborhood. Clinical examination revealed bilateral symmetrical ptosis [Figure 1], but the movement of both the eyeballs was normal in all the directions with normal pupillary size and reaction bilaterally. Other cranial nerves were essentially normal. Dysdiadochokinesia and ataxia were noted on the right side. No weakness was found in any of the limbs. Deep tendon jerks were bilaterally normal with a normal plantar response.

- An 11-year-old male child with bilateral symmetrical ptosis
Investigations revealed normal blood counts and raised erythrocyte sedimentation rate. Mantoux test was negative and chest radiograph was normal. Magnetic resonance imaging (MRI) of the brain revealed single ring-like enhancing lesion in the dorsal part of the midbrain with significant perifocal edema in adjacent parts of the brainstem, right cerebellar peduncle, adjacent thalamocortical tract, and periventricular region [Figure 2]. MRS at the site of the lesion showed increased lipid peak, decreased N-acetylaspartate (NAA) peak with increased choline/creatinine ratio, suggestive of tuberculoma [Figure 3].
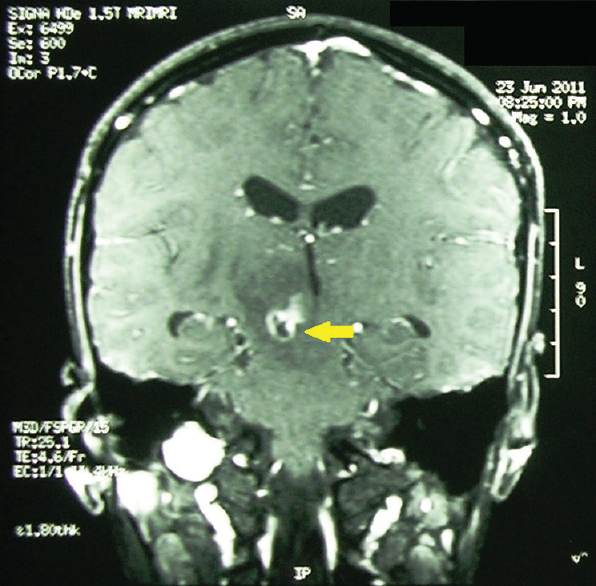
- Magnetic resonance imaging of brain (T1-weighted image; contrast-enhanced) showing single ring-enhancing lesion (yellow arrow) in the dorsal part of the midbrain with significant perifocal edema in adjacent part of brainstem, right cerebellar peduncle, adjacent thalamocortical tract, and periventricular region
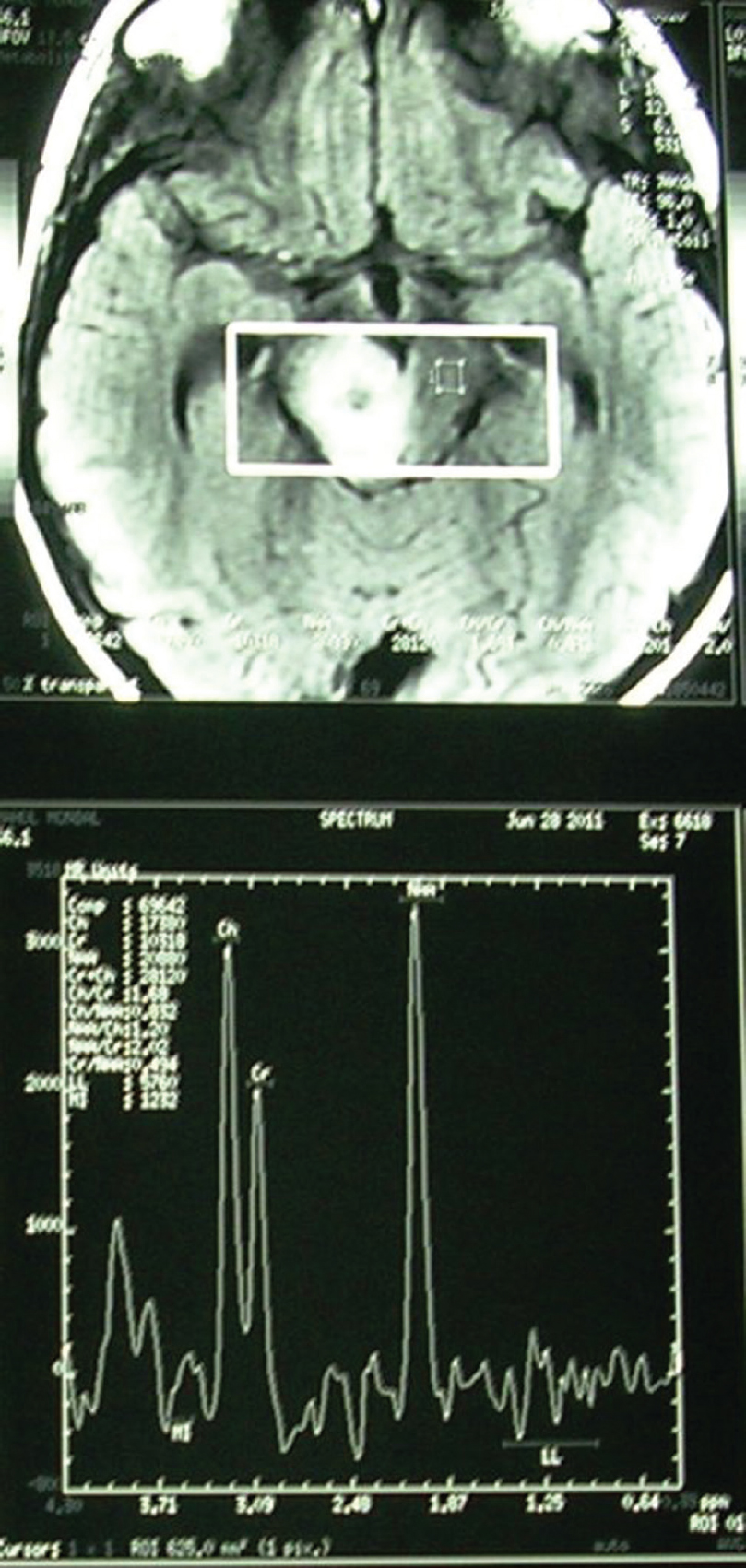
- Magnetic resonance spectroscopy showing increased lipid peak, decreased N-acetylaspartate peak with increased Ch/Cr ratio, suggestive of tuberculoma
He was started on four drugs antitubercular treatment (ATT) (isoniazid [10 mg/kg/day], rifampicin [10 mg/kg/day], ethambutol [25 mg/kg/day], and pyrazinamide [35 mg/kg/day] – all thrice a week) along with intravenous dexamethasone (0.6 mg/kg/day in 4 divided doses). Later, dexamethasone was switched over to oral prednisolone at 1 mg/kg/day which was tapered after 6 weeks. Ataxia and headache responded within 2 days of starting the treatment, whereas drooping of eyelids improved gradually after 4 weeks of treatment. No worsening of symptoms was noted. ATT was continued for 12 months (2 months intensive phase with four drugs, followed by 10 months continuation phase with isoniazid and rifampicin) and the child is doing well without any symptom at 12 and 18 months follow-up.
Discussion
Neurotuberculosis comprises 5–15% cases of extrapulmonary TB. Common locations of intracranial tuberculoma are cerebral and cerebellar hemispheres due to their rich blood supply. Other rare locations include quadrigeminal cistern, cerebellopontine angle, and suprasellar region.[3] Isolated brainstem tuberculomas are also rare with varied clinical presentations depending on the number and site of lesion and associated edema. Kumar et al. reported a patient presenting as isolated bilateral ptosis due to midbrain tuberculoma.[4] The other presentations of brainstem tuberculoma mentioned in literature were pontine tuberculoma with horizontal gaze palsy,[5] bilateral internuclear ophthalmoplegia,[6] one-and-a-half syndrome,[7] and eight-and-a-half syndrome.[8]
The nucleus of the oculomotor nerve does not consist of a continuous column of cells, but is broken up into a number of smaller nuclei, which are arranged in two groups, anterior and posterior. Those of the posterior group are six in number, five of which are symmetrical on two sides of the midline, while the sixth is centrally placed and is common to the nerves of both sides. The anterior group consists of two nuclei, an anteromedial and an anterolateral. The central caudate subnucleus is single and controls both levators. The autonomic nucleus (Edinger-Westphal) is single at one end and divided into two horns at its anterior end. A few scattered large multipolar cells are seen on the midline raphe between the right and left oculomotor masses. They innervate the superior recti muscles, rather than the medial recti. It should be noted, however, that it is more common to find ptosis in association with upgaze paresis as the unpaired superior rectus subnuclei are located medially in close relation to the caudal central subnucleus (i.e., levator palpebrae subnucleus).
The critical location of the lesion in the right dorsal midbrain with perilesional edema in our patient explains the clinical manifestations of 3rd cranial nerve palsy and cerebellar involvement. However, the occurrence of partial 3rd cranial nerve palsy (i.e., ptosis without affection of the upward gaze) could have been due to the isolated involvement of caudal central subnucleus without affecting the fibers innervating superior recti muscle.
According to the clinical picture, which suggests the topography to be midbrain and cerebellum, differential diagnoses should be the causes of childhood stroke (such as hemorrhage or infarction, notably lacunar infarcts) or any other SOL, such as brain tumor, abscess, tuberculoma, and neurocysticercosis (NCC). Lacunar infarcts presenting with atypical lacunar syndromes include bilateral paramedian thalamic lacunar infarct,[9] which can have a similar presentation clinically and, thus, should be considered as a differential diagnosis. However, the presentation here is more subacute compared to the acute stroke syndrome and MRI brain excludes the possibility by clearly showing a ring-enhancing lesion.
Now, differentiation among the ring-enhancing SOLs necessitates the use of MRS. Gliomas, metastases, abscesses, NCC, and demyelinating diseases were the differential diagnoses that were considered in our patient and MRS is considered diagnostic to exclude the differentials. MRS may increase the specificity of diagnosis by identifying lipids within the lesions that are considered characteristic for TB. In vivo and in vitro MRS has shown elevated lipid peaks within the TB lesions.[10] The other findings are decreased NAA peak and increased choline/creatinine ratio. Whereas choline/creatinine ratio is comparatively lower in NCC, demyelinating lesions may show glutamine/glutamate peak along with raised choline and low NAA, abscesses show absent NAA inside the lesion, and brain tumors have high lactate along with other routine findings. Hence, characteristic MRS findings and, finally, response to ATT supported the diagnosis of tuberculoma in our case.
This case highlights the rarity of midbrain tuberculoma and its unique presentation as isolated nuclear oculomotor nerve palsy with cerebellar involvement. It also justifies the importance of realizing the architectural organization of oculomotor nerve fibers responsible for its varying clinical presentations. To the best of our knowledge, ataxia with bilateral ptosis without any gaze palsy due to midbrain tuberculoma has not been previously reported.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Neurological tuberculosis. In: Sharma SK, ed. Tuberculosis (1st ed). India: Jaypee Publications; 2001. p. :209-28.
- [Google Scholar]
- Isolated bilateral ptosis as the presentation of midbrain tuberculoma. Neurol India. 2008;56:212-3.
- [Google Scholar]
- Pontine tuberculoma presenting with horizontal gaze palsy. J Neuroophthalmol. 2006;26:276-8.
- [Google Scholar]
- Tuberculomas presenting as isolated intrinsic brain stem masses. Br J Neurosurg. 1997;11:127-33.
- [Google Scholar]
- Isolated “one and a half syndrome” with brainstem tuberculoma. Indian J Pediatr. 2004;71:469-71.
- [Google Scholar]
- Brainstem tuberculoma presenting as eight-and-a-half syndrome. Eur J Paediatr Neurol. 2006;10:41-4.
- [Google Scholar]
- Clinical study of 39 patients with atypical lacunar syndrome. J Neurol Neurosurg Psychiatry. 2006;77:381-4.
- [Google Scholar]
- The diagnosis of brain tuberculoma by (1)H-magnetic resonance spectroscopy. Eur J Pediatr. 2011;170:379-87.
- [Google Scholar]






