Translate this page into:
Bilateral optic nerve infarction in rhino-cerebral mucormycosis: A rare magnetic resonance imaging finding
Address for correspondence: Dr. Mandeep Singh Ghuman, Dayanand Medical College and Hospital, Ludhiana - 141 001, Punjab, India. E-mail: dr.msghuman@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Mucormycosis is an emerging disease in diabetes and immunocompromised patients. Rhino-orbito-cerebral mucormycosis is one of the common forms of the disease. Mucormycosis leading to ischemic optic neuropathy is a rare complication. The role of magnetic resonance imaging (MRI) in the diagnosis of ischemic optic neuropathy is limited and uncommonly reported. We report an unusual case of mucormycosis in which MRI revealed bilateral optic nerve infarction, in addition to perineural extension of the fungus along the trigeminal nerve, another uncommon imaging finding.
Keywords
Ischemic optic neuropathy
MRI
optic nerve infarction
perineural spread
rhino-cerebral mucormycosis
Introduction
Mucormycosis is a devastating opportunistic infection associated with high mortality.[1] In developing countries such as India, it is on an emerging trend due to the vast number of diabetes mellitus cases. Most of the cases occur in patients with uncontrolled diabetes mellitus and compromised immune status, and rhino-cerebral mucormycosis is the most common form of the disease.[2] The fungus rapidly spreads from paranasal sinuses to orbits and cavernous sinuses with extension to intracranial vasculature and brain. Common pathological hallmark is vascular invasion and neurotropism.[23] An extremely rarely reported complication of rhino-cerebral mucormycosis is optic nerve infarction. Another unusually seen phenomenon is perineural spread. We describe MRI findings in a case in which both of these complications occurred concurrently and were clearly evident on imaging.
Case Report
A 33-year-old female, known type-1 diabetes mellitus with ketoacidosis, presented with nasal bleeding with blackish nasal crusts, periorbital swelling, proptosis and left hemifacial pain. She further developed decreased vision in both eyes and altered sensorium. Examination showed bilateral ophthalmoplegia, left corneal and left hemifacial sensory loss. Visual acuity was limited to detecting hand movements at one foot bilaterally. Magnetic resonance imaging (MRI) revealed intensely hypointense signal, involving medial orbits bilaterally, orbital apices, and left cavernous sinus suggesting a fungal pathology. Diffusion-weighted (DW) MRI and corresponding ADC maps [Figure 1b and c] demonstrated bilateral optic nerve infarction. Abnormal signal intensity was also noted along the left trigeminal nerve in left side of the ambient cistern extending into the left side of pons [Figures 1a and 2a and b]. Smear of sinonasal aspirate and histopathology of nasal crusts confirmed mucormycosis.
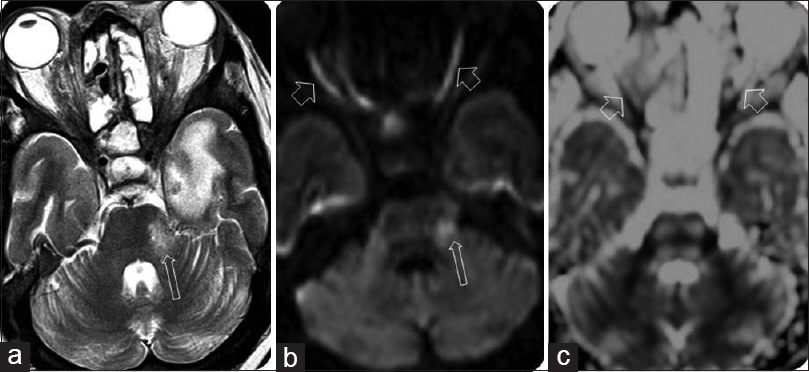
- Axial T2-weighted image (a) reveals pansinusitis, soft tissue consistent with cellulitis in the medial -orbits, with hypointense signal extending posteriorly to the orbital apices, and contiguous involvement of left medial temporal lobe. Abnormal high signal is seen in the left side of pons (arrow) corresponding to the location of 5th nerve nuclei. Axial diffusion-weighted image (b) clearly demonstrates high signal in the bilateral optic nerves (short arrows) with corresponding hypointensity on ADC image (c, short arrows) consistent with infarction. Restricted diffusion is seen in the pons (b, long arrows)

- Axial diffusion-weighted image (a) and fluid-attenuated inversion recovery image (b) showing abnormal high signal and thickening of the cisternal segment of the left trigeminal nerve (thin arrows) extending to involve the left side of the pons (chevron)
Discussion
Mucor, a saprophytic fungus, occasionally causes a potentially fatal opportunistic infection of the paranasal sinuses and nasal airway with progressive involvement of orbit and brain.[12] Rhino-orbitocerebral mucormycosis usually affects persons with diabetes and immunocompromised state.[24] From the paranasal sinuses, fungus can invade the orbit and infiltrate posteriorly into the cavernous sinuses and can lead to thrombosis of the cavernous sinus and cavernous internal carotid artery (ICA). Because of its predilection for spread along vessel walls, mucor is sometimes called “angiotropic” Intracranial extension may occur due to this angiotropic spread or due to distal mycotic emboli or contiguous meningeal inflammation.[4]
Thorough search of the literature revealed very few cases of diffusion-weighted MRI demonstration of optic ischemic neuropathy.[5] Out of these, MRI demonstrated ischemic optic nerve involvement due rhino-orbito-cerebral mucormycosis in only three case reports.[678] MRI findings confirming the infarction of the optic nerve are high signal intensity along the optic nerves on diffusion-weighted imaging, with corresponding low signal on apparent diffusion coefficient map with normal fluid-attenuated inversion recovery (FLAIR) and gadolinium-enhanced images.[67] These imaging findings and ensuing blindness may result from the invasion of the blood vessel walls by the organisms leading to occlusion or thrombosis of the central retinal artery or ophthalmic artery or direct optic nerve infiltration by mucormycosis.[69] Diffusion-weighted imaging is vital for early diagnosis of ischemic optic neuropathy and it shows the abnormality when other MR sequences are normal.[68]
Various head and neck malignancies, such as adenoid cystic carcinoma, squamous cell carcinoma and lymphoma, are well known to spread in perineural fashion, the trigeminal nerve and its branches being the common site.[10] Perineural extension has been uncommonly reported in invasive mucormycosis. From the cavernous sinus, extension along the trigeminal nerve to the pons has been described in few case reports.[41011]
Conclusion
In conclusion, rhinocerebral mycosis is an increasingly common infection especially in developing countries, and is a major threat to patients with poorly controlled diabetes mellitus. Ischemic involvement of the optic nerves, although a rare complication, should be considered in cases presenting with visual symptoms. Urgent MRI with diffusion-weighted imaging has a definite role in early diagnosis and management. As commonly demonstrated in histopathological specimens, imaging can reveal perineural extension along the cranial nerves with resultant involvement of the brainstem.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis. 2012;54(Suppl 1):S23-34.
- [Google Scholar]
- The rising trend of invasive zygomycosis in patients with uncontrolled diabetes mellitus. Med Mycol. 2006;44:335-42.
- [Google Scholar]
- Invasive mold infections: Virulence and pathogenesis of mucorales. Int J Microbiol 2012 2012 349278
- [Google Scholar]
- Perineural spread of rhinocerebral mucormycosis. AJNR Am J Neuroradiol. 1996;17:114-6.
- [Google Scholar]
- Diffusion-weighted MRI in acute posterior ischemic optic neuropathy. Indian J Radiol Imaging. 2012;22:106-7.
- [Google Scholar]
- Acute optic nerve infarction demonstrated by diffusion-weighted imaging in a case of rhinocerebral mucormycosis. AJNR Am J Neuroradiol. 2007;28:489-90.
- [Google Scholar]
- Diffusion MR imaging in a case of acute ischemic optic neuropathy. AJNR Am J Neuroradiol. 2006;27:255-7.
- [Google Scholar]
- Optic nerve thickening and infarction as the first evidence of orbital involvement with mucormycosis. Middle East Afr J Ophthalmol. 2012;19:340-2.
- [Google Scholar]
- Sudden blindness and total ophthalmoplegia in mucormycosis: A clinicopathologic correlation. J Clin Neuroophthalmol. 1993;13:27-34.
- [Google Scholar]
- Clinical-radiologic issues in perineural tumour spread of malignant diseases of the extracranial head and neck. Radiographics. 1991;11:383-99.
- [Google Scholar]
- Rhinocerbral mucormycosis: Perineural spread via the trigeminal nerve. J Clin Neurosci. 2005;12:484-6.
- [Google Scholar]






