Translate this page into:
Belly Dancer's Dyskinesia Responsive to Oral Medication Treatment
Stella Natadidjaja, MD Department of Neurology, Faculty of Medicine, Universitas Sam Ratulangi/R.D. Kandou Hospital Jl W. Mongisidi No. 56, Malalayang, Manado 95162, Sulawesi Utara Indonesia stella.natadidjaja@yahoo.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Belly dancer's dyskinesia is a rare disease characterized mostly by the uncontrolled and rhythmic movements of the abdominal wall. No exact etiology has been identified yet and the treatment is mostly symptomatic. From most available case reports, oral medication therapy often provides disappointing result in term of reducing the symptom. Here, we report a patient who has satisfactory improvement after treated with oral medication only.
Keywords
belly dancer's dyskinesia
haloperidol
clobazam
Introduction
Iliceto et al first reported a serial case of belly dancer's dyskinesia/dystonia (BDD) in 1990.1 BDD is still considered as a rare type of movement disorder characterized by uncontrolled and rhythmic movements of the abdominal wall.2 The pathomechanism is not well understood and the case is mostly idiopathic in nature.3 4 Some are related to disorders of the basal ganglia, the complication of abdominal diseases or surgery, prior infection, thyroid dysfunction, or the use of dyskinesia-inducing drugs such as domperidone.2 4 5 Genetic influence is unclear. The conservative management is often not satisfactory and invasive/surgical procedures might be needed.2 6
Case Report
A 47-year-old Indonesian man with uncontrolled movement on his belly for 1 year visited our clinic. He described the movement as a sudden, undulating movement, from the right to the left side of his belly or vice versa. The frequency and duration were increasing until now. Recently, the movement sometimes extended to his shoulders, especially on the right. He cannot control the movement when awake, but it disappeared during sleep. No exacerbating nor relieving factors were noted. The movement was not influenced by changing his position or taking a deep breath. After each episode, he experienced pain over his belly and difficulty to breath. He also has a history of eyes winking and nose sniffing habit since childhood. He can suppress the urge to do it for a short time but feel uncomfortable. No remarkable history of illness, specific medication, or similar disease in his family.
The patient was kyphoscoliotic and the rest of the general examination was within normal limit. On neurological examination, he was fully awake and no meningeal signs were noted. Cranial nerves examinations were normal. On inspection, we found a rhythmic undulating movement of the abdomen (Video 1). This movement was not influenced by activity, body position, or respiration, and no shoulder involvement was noted. He was unable to control the movement and complaining about pain over the abdomen after each contraction. On a 5-minute observation, the movement continuously appeared with no change in pattern and intensity. The patient can suppress the urge for a short time. We also found brief, repeated, and nonrhythmic contractions of the muscles around the eyes and nose. Muscle strength, tone, and physiological reflexes were normal. Pathological reflexes were absent. No sensory abnormality was found. Gait and stance were normal. The routine neurobehavior examination was also normal.
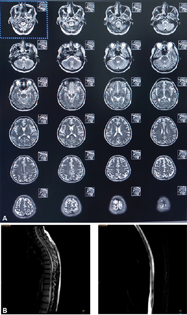
Routine hematology and blood chemistry test were unremarkable. Chest X-ray, brain magnetic resonance imaging (MRI) (Fig. 1A), and whole spine MRI (Fig. 1B) showed no abnormality. The electroencephalogram (EEG) and routine electromyogram (EMG) were within normal limit. Abdominal fluoroscopy and ultrasound were not done.
-
Fig. 1 Brain and spine MRI of the patient. The T2WI axial brain MRI (A), T2WI sagittal spine MRI (left, B), and myelography (right, B) sequences showed no abnormality. MRI, magnetic resonance imaging; T2WI, T2-weighted imaging.
Fig. 1 Brain and spine MRI of the patient. The T2WI axial brain MRI (A), T2WI sagittal spine MRI (left, B), and myelography (right, B) sequences showed no abnormality. MRI, magnetic resonance imaging; T2WI, T2-weighted imaging.
He was diagnosed as BDD and facial tic and treated with oral haloperidol 0.5 mg three times a day and clobazam 10 mg three times a day for 10 days. On day 10, the movement was diminished but the patient complained about oversleeping. The haloperidol was then reduced to 0.5 mg twice a day. One week after, the movement was diminished. He felt no oversleeping and abdominal pain. He can accept the reduced level of symptom. One year after the initial examination, he was still on the same regiment and functioned well in his daily activities. The belly movement was still diminished (Video 2).
Discussion
The clinical manifestation of BDD is the fluttering of the anterior abdominal wall. The movements are involuntary, repetitive, semicontinuous, sometimes painful, often rhythmic, and slow writhing.2 This description is consistent with our patient. A focal seizure was unlikely since the abdominal wall movement persisted for a long period and the EEG result was normal. The movement pattern was also difficult to be trained.
The BDD has been reported to be originated from basal ganglia, spinal cord, and peripheral nerve.4 5 We believe the BDD in this patient originated from basal ganglia. In general, if the dyskinesia is caused by basal ganglia pathology, it will disappear during sleep but will persist if caused by spinal cord or peripheral nerve lesion.5 Furthermore, a central origin is more likely if the movement is bilateral in fashion.4
Idiopathic etiology was most likely to be the cause here. No history of medication/illness that can induce dyskinesia was found. Brain and spinal cord MRI and EEG were also normal. In BDD caused by the phrenic nerve irritation, the heart is the most common source. In such cases, the flutter should be synchronous with the systole which was not observed in this patient.2
Generally, the facial tic, as found in this patient, was hypothesized to be caused by the disruption of gamma-aminobutyric acid (GABA) transmission resulting in disinhibition of the corticobasal ganglia-thalamocortical circuitry.7 Other literatures emphasize the role of dopaminergic and serotonergic neurotransmission.8 Derived from those hypotheses, we can assume that there is a relationship between the facial tic and BDD found in this patient. However, only a few literatures reported a facial tic found with BDD.4 None of them provided sufficient explanation.
Current treatments for BDD were based on expert opinion and case reports due to the rarity of the disease. Many reports described BDD as difficult to treat.2 Diphenylhydantoin is the oral medication frequently used to treat this disorder. However, the reported results vary. Diazepam, clonazepam, and haloperidol have also been shown to be beneficial.2 4
We chose to start the treatment with haloperidol and clobazam. The use of haloperidol has been reported previously in some case reports with variable results.2 4 However, to the best of our knowledge, the use of clobazam for BDD has not been reported in medical literature yet. Clobazam is a long-acting benzodiazepine that was used to treat some type of epilepsy and also has anxiolytic property.9 There are some reasons for us to use clobazam. First, clobazam was known to potentiate the GABA-ergic neurotransmission by binding at the benzodiazepine site at the α2 subunit of GABA(A) receptor.9 Second, this drug is widely available in our region.
The limitation of this case report is that no surface EMG performed on this patient due to device problem. EMG can provide assistance in excluding the possibility of a rare type of spinal myoclonus, the propriospinal myoclonus. In propriospinal myoclonus, EMG activity has a specific temporospatial distribution that is not found in BDD.5
Conclusion
For functional and central BDD, haloperidol and clobazam may provide satisfactory control of the movement disorder like in our case.
Conflict of Interest
None declared.
Funding None.
References
- Diaphragmatic flutter, the moving umbilicus syndrome, and “belly dancer's” dyskinesia. Mov Disord. 1990;5(1):15-22.
- [Google Scholar]
- Belly dancer's dyskinesia: a glimpse of a rare phenomenon. Cureus. 2017;9(7):e1457.
- [Google Scholar]
- Belly dancer's syndrome following central pontine and extrapontine myelinolysis. Mov Disord. 2007;22(6):892-894.
- [Google Scholar]
- Belly dancer's syndrome: causes, clinical presentations, and treatment options. . Accessed June 3, 2021 at:
- [Publisher] [Google Scholar]
- A case of functional belly dancer's dyskinesia. Mov Disord Clin Pract (Hoboken). 2015;3(3):306-308.
- [Google Scholar]
- Ultrasound-guided botulinum toxin A injection in the treatment of belly dancer's dyskinesia. BMC Neurol. 2016;16(1):226.
- [Google Scholar]
- Tics and Tourette: a clinical, pathophysiological and etiological review. Curr Opin Pediatr. 2017;29(6):665-673.
- [Google Scholar]
- Mechanisms of dopaminergic and serotonergic neurotransmission in Tourette syndrome: clues from an in vivo neurochemistry study with PET. Neuropsychopharmacology. 2008;33(6):1239-1251.
- [Google Scholar]
- Clobazam: a safe, efficacious, and newly rediscovered therapeutic for epilepsy. CNS Neurosci Ther. 2015;21(7):543-548.
- [Google Scholar]








