Translate this page into:
Back bugged: A case of sacral hydatid cyst
Address for correspondence: Dr. Dhaval Shukla, Department of Neurosurgery, National Institute of Mental Health and Neurosciences (NIMHANS), Hosur Road, Bangalore-560 029, India. E-mail: neurodhaval@rediffmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Hydatid cyst of bone constitutes only 0.5 - 2% of all hydatidoses. The thoracic spine is the most common site of spinal hydatidoses. Primary hydatid cyst of the sacral spinal canal is rare. A 23-year-old gentleman had back pain five years ago. At that time he was evaluated and found to have a small cyst in S1 spinal canal, which was presumed to be a benign Tarlov's cyst; and no treatment was offered. He continued to have back pain and also developed sciatica on the right side. Neurological examination presently revealed right S1 radiculopathy. Magnetic resonance imaging (MRI) showed a large multiloculated cystic lesion extending from L5 to S2 spinal canal with bone erosion, both anteriorly and posteriorly. He underwent L5 to S2 laminectomy and excision of multiple cysts. The whole cyst was excised and cavity irrigated with sterilized formalin. A laparoscope was introduced in the cavity to look for extension into the pelvis and to confirm complete excision. Postoperatively, the patient received albendazole for two months. At 16 months follow-up the patient was asymptomatic. Hydatid cyst of sacrum is rare and can be missed at initial presentation. If the patient with a cystic lesion of sacral continues to have symptoms the diagnosis should be revaluated and prompt treatment should be offered.
Keywords
Cestode
echinococcus
hydatid
sacrum
spine
Introduction
The commonest site of hydatid cyst is liver and lungs. Skeletal hydatidosis occurs in 0.5 to 2% cases, half of which infest the spine.[1–3] The commonest site is thoracic and sacral involvement is rare.[2] We report a case of sacral hydatid cyst.
Case Report
A gentleman aged 27 years presented with back pain, right sciatica and voiding difficulty for last one year. In 2003 he was evaluated elsewhere for back pain when he did not have neurological deficits. Magnetic resonance imaging (MRI) at that time showed small cystic lesion in sacrum and no active treatment was offered [Figure 1]. He is a vegan, has no pets at home and never had back injury.
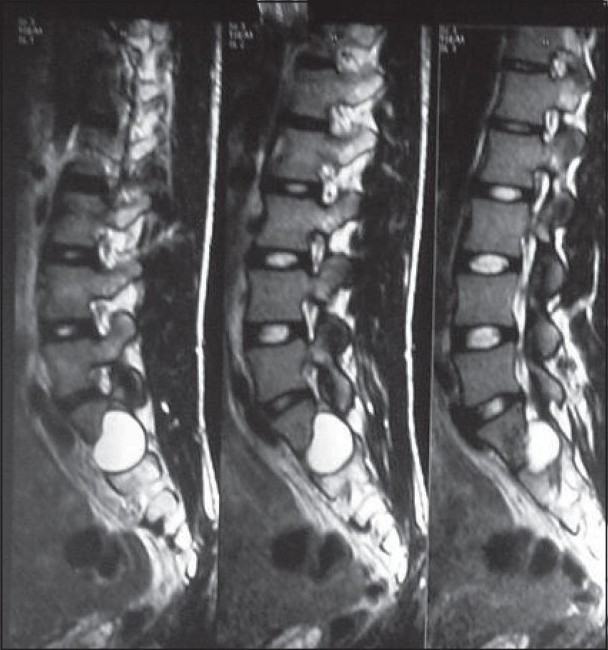
- MRI T2W, done in 2003 shows a small cystic lesion of sacrum, which was presumed to be Tarlov's cyst
On presentation to our clinic his neurological examination revealed weakness of right foot and hypoesthesia of dermatomes below L5. There was no significant restriction of straight leg raise (SLR). A repeat MRI done in 2007 showed significant increase in size of cyst with inhomogeneous contents [Figure 2]. Our working diagnosis was a cystic bone tumor.
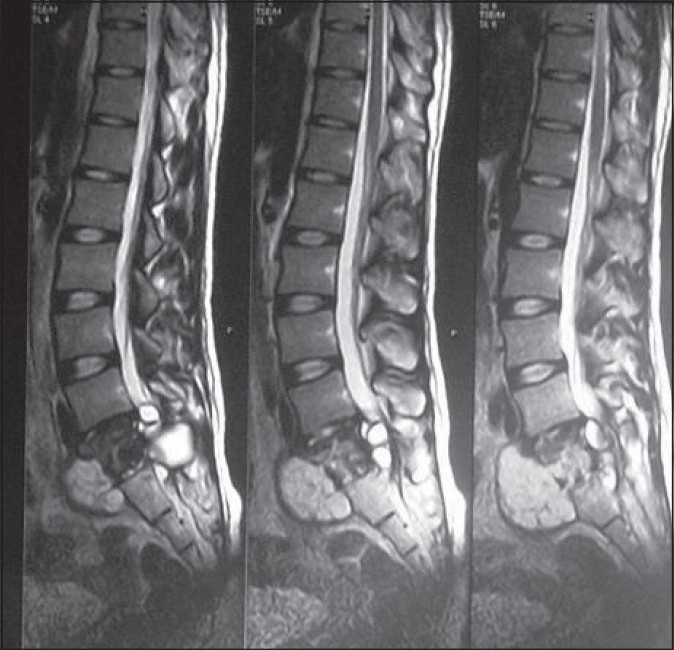
- MRI T2W, done in 2007 shows enlargement of previous sacral cystic lesion with heterogeneous intensity and extension into presacral space and spinal canal
He underwent L5 to S2 laminectomy and excision of cyst. Cyst was lined by thin fibrous wall and had eroded laminae of S2. Inner lining of cyst was white with multiple daughter cysts within [Figure 3]. The fluid was clear. A few types of sediments were also present. The cyst cavity was irrigated by formalin 1%. No adverse reaction occurred during surgery. Cyst was totally excised and laparoscopic inspection was done to look for intrapelvic extension and confirm completion of excision. A negative suction drain was placed in the space left behind after excision of cyst.

- Chitinous cyst wall with multiple daughter cysts
Postoperatively, he had persistent watery discharge. A myelo computerized tomography (CT) scan of spine did not reveal any cerebrospinal fluid (CSF) leak. The drain was retained for 12 days and leak subsided. X-ray chest and ultrasound examination of abdomen did not reveal any other cysts. He received albendazole 800 mg / day for two months. An MRI was done seven months after surgery showed collapsed cyst [Figure 4]. At the last follow-up after 16 months of surgery he was asymptomatic.

- MRI T2W done after seven months of surgery shows collapsed cyst. There are no intracystic contents. There is no epidural compression
Discussion
Epidemiology
Hydatid cysts predominantly occur in liver and lungs. Involvement of other organs is uncommon. Skeletal involvement occurs in 0.5 to 2% of all cases, half of which are in the spine.[14] A neurosurgeon encounters hydatid cyst in brain and spine. Hydatid cyst of brain is more common than spine. In a series of 29 cases of intracranial and spinal hydatid cysts, no sacral lesion was seen.[5] In a series of 25 cases of vertebral hydatidosis the cyst was located in the cervical vertebrae in three, the thoracic vertebrae in 11, the lumbar vertebrae in five, and the sacrum in six cases.[6] In another series of 13 cases of vertebral hydatidosis, sacrum was involved in only one case.[7] Approximately 90% of spinal hydatidosis cases are located extradurally, most commonly in the vertebral body. Intradural location is very rare and appears like an arachnoid cyst.[8]
Clinical features
As there is no host reaction the cyst can grow to enormous size and remain asymptomatic. The initial symptom is back pain when cyst invades spinal canal after erosion of bony cortex. As whole vertebral body is destroyed, gibbus deformity does not result. The neurological symptoms are those of extradural tumor or disc disease.[1]
Hydatid disease of sacrum is not easily detected. In one case report, sacral hydatid cyst was not suspected and the symptoms were considered due to lumbar disc disease. The diagnosis was delayed up to 12 years as pelvis was not imagined, which could have shown a cystic lesion in presacral space.[9] Even in our case diagnosis was missed as the small cystic lesion was presumed as Tarlov's cyst. The other differential diagnosis of cystic lesion of sacrum includes developmental cysts (epidermoid, dermoid, teratoma, neurenteric and retrorectal cystic hamartoma (tail gut cyst)), anterior sacral meningocele, necrotic sacral chordoma, schwannoma, arachnoid cyst, and aneurysmal bone cyst.[6]
Imaging
Though no specific imaging features point to hydatid cyst, the presence of the following appearances should consider hydatid cyst at top of suspicion, particularly in an endemic country.[6]
-
Lytic lesion with dense calcified rim
-
No disc space involvement
-
Multiloculated cyst with signal of parent cyst similar to muscle on T1W
-
Signal of daughter cyst similar to water
-
Daughter cyst in, overflowing or adjacent to parent cyst
-
Both parent and daughter cysts with higher signal on T2W with rose or wheel shape formation
-
Decrease in hyper intensity and increase in hypo intensity with time as cyst succumbs
Treatment
Neither surgery nor medical therapy is generally effective for bone, especially spinal hydatidosis. The initial treatment of choice is surgical excision for neural decompression and establishing diagnosis. The operative finding of a large cyst with multiple chitinous small cysts is virtually diagnostic. After excision local scolicidal agents like hypertonic saline or cetrimide should be used for irrigation instead of formalin. Inadvertent opening of dura can lead to intradural recurrence and spillage of local scolicidal agent. In one case, death occurred due to toxic myelitis and respiratory arrest from intradural spillage of formalin.[7] We were not aware of this complication and have used formalin. Fortunately no untoward event occurred during or after surgery. Patients may require stabilization after extensive resection. Subcutaneous drainage for prolonged period after surgery is advised due to persistent discharge.
Albendazole is the drug of choice against this disease. When suspected, presurgical use of albendazole in echinococcus infestations reduces risk of recurrence and/or facilitates surgery by reducing intracystic pressure. A dose of 400 mg twice daily for 28 days, for otherwise healthy adults, and for children a dose of 15 mg / kg of body weight daily in two divided doses (not to exceed total daily dose of 800 mg) should be given. The 28-day course may be repeated after 14 days without treatment to a total of three treatment cycles. Treatment with albendazole in E. granulosus infection can result in an apparent cure in as many as 30% of patients, with a further 40-50% of patients showing objective evidence of response when observed short term. Patients who do not show obvious initial evidence of response may be found to be cured when observed over several years. Though it is a benign disease, due to frequent recurrences and dissemination, the behavior is of malignancy. The overall recurrence rate is 30 to 40%.[10] When recurrence occurs, repeat excision should be attempted if feasible.
Conclusion
A missed diagnosis of hydatid cyst could be devastating. Hence, hydatid cyst should be kept as a differential diagnosis when encountered with a cystic lesion of sacrum. In addition, long-term follow-up is mandatory as recurrence is high despite use of scolicidal agents.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Diagnosis and management of hydatid cyst of the central nervous system: Part 2: Hydatid cysts of the skull, orbit, and spine. Neuro Quart. 2001;11:10-6.
- [Google Scholar]
- Combined medical and surgical treatment of spinal hydatid disease: A case report. J Neurol Neurosurg Psychiatry. 1982;45:927-31.
- [Google Scholar]
- Spinal hydatid disease, a rare but existent pathological entity: Case report and review of the literature. South Med J. 2006;99:178-83.
- [Google Scholar]
- Cestode parasitic infestation: intracranial and spinal hydatid disease: A clinicopathological study of 29 cases from South India. Clin Neuropathol. 2006;25:98-104.
- [Google Scholar]
- Primary spinal intradural hydatid cyst: A short report. Neurol India. 2001;40:203-4.
- [Google Scholar]






