Translate this page into:
Attitudes toward psychotropic medications among patients with chronic psychiatric disorders and their family caregivers
Address for correspondence: Dr. Sandeep Grover, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh - 160 012, India. E-mail: drsandeepg2002@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
To examine attitudes towards psychotropic medications among patients with chronic psychiatric disorders as well as their family caregivers by using factor analysis.
Materials and Methods:
The study included 200 patients and their family caregivers with chronic psychiatric disorders who are attending the psychiatry outpatient services. A self-designed 18-item self-rated questionnaire was used to evaluate the attitude toward psychotropics and factor analysis was done to study the different models of attitudes.
Results:
In general both patients and caregivers had positive attitude toward the psychotropic medications and there was no significant difference between the patients and caregivers on the various items of the questionnaire assessing the attitude. Factor analysis of the questionnaire indicated that either two-factor or four-factor models explained the attitude of the patients and caregivers. In the two-factor model there was one positive and one negative attitude factor, whereas the four-factor model comprised of two positive and two negative attitude factors. The four-factor model of attitudes provided a more comprehensive solution to how attitudes might be formed among patients and their family caregivers. Factors one and four in the four-factor solution still reflected positive attitudes, but appeared to portray a risk-benefit approach, in which benefits such as the efficacy of psychotropic medications in treating mental illnesses and preventing relapse, and medications being better than other options were being contrasted with the risks of side effects and permanent damage or harm.
Conclusion:
Attitudes of patients with chronic psychiatric disorders and their caregivers toward psychotropic medications appear to be shaped by factors such as perceived efficacy or benefit from medicines, the necessity for taking treatment and concerns such as side effects, harm or expense.
Keywords
Attitude toward medications
family caregivers
patients
psychotropics
Introduction
Medication non-adherence is a common and complex barrier to effective long-term treatment of chronic psychiatric disorders. Reported rates of non-adherence vary greatly across different studies of psychotic, mood and anxiety disorders, but fall somewhere within the range of 24% to 90%; on the average about half or more of the patients with these disorders are non-adherent at any given point of time.[123] Non-adherence has several adverse consequences. It worsens the course of the illness and leads to impaired functioning, which in turn increase the burden on the caregivers and on the society, by increasing the costs of care of chronic psychiatric disorders.
A multitude of factors can potentially influence adherence to a prescribed psychotropic medication regimen. Traditionally, studies have focused more on demographic, clinical and treatment-related factors. However, research over the past two decades or so has highlighted the contribution of patients’ perspectives toward adherence. According to social, cognitive and behavioral perspectives, adherence or non-adherence is often a considered decision by people making their own choices about the benefits and disadvantages of treatment, based on their own attitudes and beliefs, their personal circumstances, and the information available to them.[45] The construct of attitudes to medications represents a convenient proxy measure for this decision-making process on part of the patients.[6] Therefore, it comes as no surprise that patients’ attitudes toward medications have been consistently linked to their likelihood of adhering to the prescribed medication regimen.[78] Moreover, unlike many other factors influencing medication adherence, attitudes toward medications can be modified by appropriate patient-centered interventions. Hence, it is profitable to explore attitudes of patients toward psychotropic medications.
A patient's attitudes to treatment can be influenced by a variety of factors including psychopathology, insight, side effects of medications, health beliefs, and the clinician-patient relationship. Additionally, certain studies have also found that attitudes of family members and their knowledge of the patient's illness contribute to adherence,[9101112] and that attitudes of the family toward psychotropic medications can influence the attitudes of patients toward these medications.[13141516] Attitudes held by family members are of particular importance in the Indian context, where there is a greater involvement of the family in all aspects of the patient's care, including the decision to take prescribed medicines.[17] However, the number of studies, which have examined the attitudes among family caregivers, including those from India, is still quite small.
These considerations provided the impetus for the current study, which attempted to examine attitudes to psychotropic medications among patients with chronic psychiatric disorders as well as their family caregivers. A relatively large and diverse group of patients with chronic psychiatric disorders was chosen to make the study more relevant and representative of such patients.
Materials and Methods
The study was approved by the Ethics Committee of the Institute where it was conducted. The study was partly funded by the institute. All the patients and their caregivers were recruited after obtaining proper written informed consent. Other ethical safeguards were maintained during the conduct of the study.
Participants
The sample for the study comprised of 200 patients and their family caregivers with chronic psychiatric disorders who are attending the psychiatry outpatient services.
Patients were included if they were more than 18 years of age, were suffering from any chronic psychiatric disorder of more than a year's duration, were receiving psychotropic medications for at least 1 year, were able to read Hindi or English, and consented to participate in the study. All patients were “clinically stable”, i.e. there had been no major change in their clinical condition in the 3 months prior to inclusion, and not more than a 50% hike or reduction of dosages of psychotropics during this period. Patients who were acutely ill, uncooperative, aggressive or actively suicidal, or cognitively impaired were excluded.
Family caregivers of these patients were included if they were more than 18 years of age, were living with and involved in patient's care for the past 1 year or more prior to inclusion, were able to read Hindi or English, and consented to participate in the study. Family caregivers who were themselves suffering from any mental illness or mental retardation were excluded.
Assessments
Apart from recording demographic, clinical and treatment data, the principal task of this study was to assess attitudes toward psychotropic medications among patients and their family caregivers. There are several well-validated scales for assessment of attitudes among patients including the Drug Attitude Inventory (DAI),[18] the Rating of Medication Influences scale (ROMI).[19] the Attitudes toward Neuroleptic Treatment (ANT)[20] questionnaire, and the Antidepressant Compliance Questionnaire (ADCQ).[21] However, for several reasons these scales did not suit the purpose of this study. Firstly, all these scales were meant for assessing attitudes among patients, and not meant to be used for assessing attitudes of caregivers. Studies assessing caregivers’ attitudes have devised their own questionnaires, but these have not been properly validated.[1416] Secondly the DAI, the ROMI and the ANT questionnaire are meant to assess attitudes toward antipsychotics. They have thus been mainly used among patients with psychosis or schizophrenia, and only occasionally among patients with depressive or bipolar disorders.[2223] Finally, in our experience some of the items of these scales such as the DAI are not well understood by Indian patients,[242526] while other common culturally derived beliefs and attitudes are, understandably, not incorporated in these scales.
Accordingly, a questionnaire, named Self Report Attitude Toward Psychotropic Medications Questionnaire, was devised to assess attitudes toward psychotropic medications among patients with a wide range of chronic psychiatric disorders including psychotic disorders, mood disorders (both major depressive and bipolar disorders), and other chronic psychiatric disorders. Moreover, the questionnaire was devised in such a way that it could also be used to elicit attitudes of family caregivers toward psychotropic medications. For this purpose, a 7-item questionnaire for measuring attitudes toward psychotropic medications or antipsychotics among laypersons, as well as professional and non-professional caregivers was adapted for use in this study.[2728] Firstly, the wording of the items was modified to elicit attitudes toward psychotropic medications in general and not just antipsychotics. Secondly, the scoring pattern of the scale was simplified. In the original version of this instrument, each statement is rated on a five-point scale from: 1- ‘completely agree’ to 5- ‘completely disagree’.[28] While the original Likert format of the scale was maintained, items were scored on a three-point scale with three options for the items eliciting positive attitudes including: 1 - “strongly disagree”. 2- “agree to an extent”, and 3- “strongly agree”. For the items assessing negative attitudes, the pattern of scoring was reversed, which ensured that a higher score always reflected more positive attitudes on each item (1-3) and for the total score of the scale (range 18-54). Finally, additional items which reflected common culturally derived attitudes toward medications were incorporated after discussions with other mental health professionals, patients and their caregivers. The outcome of this process resulted in an 18-item questionnaire in English, which was translated to Hindi (the local language) using standardized methodology proposed by the World Health Organization.[29] All efforts were made to keep the questionnaire as short and simple as possible to enhance its ease of use. The Hindi version of the questionnaire was again reviewed by a panel of experts and was administered to the patients and their caregivers to assess the language and wording of the questions. All the suggestions made during this phase were incorporated by arriving at a consensus. Of the 18 items of the questionnaire, 10 items assessed negative attitudes and 8 items assessed the positive attitudes toward psychotropic medications. The questionnaire was designed to be used as a self-report measure. Before asking the participants to complete the questionnaire, clear instructions were given about the purpose of the questionnaire and the response categories. Once these instructions were understood, most participants had no difficulty in completing the questionnaire and took about 4-6 minutes to complete the questionnaire.
Data analysis
Data were analyzed using the Statistical Package for Social Scientists, version fourteen (SPSS-14).[30] Frequency, percentage, mean, and standard deviation were calculated for the descriptive data. Comparisons were done using the Chi-square and Fishers’ exact test for the nominal and ordinal variables, and t-tests for the continuous variables. Exploratory factor analysis was carried out using a principal components analysis. Principal components analysis was chosen as the primary aim was to determine the minimum number of factors that would account for the maximum variance in the data. Initially a correlation matrix was prepared. The Kaiser Meyer Olkin measure of sampling adequacy and the Bartlett's Test of Sphericity were assessed. Once it was confirmed that the data lent itself to factor analysis, the number of factors derived on the basis of un-rotated matrix were evaluated. Next the data were subjected to orthogonal rotation using the varimax technique to increase interpretability and interpretation of the results. Loadings of ≥0.4 of an item on a particular factor were considered to be significant loadings, and the item was included in that factor. When the variable loaded at 0.40 or above on more than one factor, it was assigned to the factor on which it had the higher loading. For determining the optimum number of the factors, the Kaiser-Guttman Rule[31] was used. Only factors with Eigen value of more than 1 and loadings that were ≥0.4 were retained to render the extracted factors meaningful and interpretable. A scree plot was also generated, and previous literature was referred to determine the factor solutions that would provide best fit for the data.
Results
The study included 200 patients with chronic psychiatric disorders and 200 family caregivers of these patients. The mean age of the patients was 36.47 (SD-12.83; range 18-82) years and that of caregivers was 45.27 (SD-12.54; range 18-85). More than half of the patients (55%) were females, whereas more than half of the caregivers (54.5%) were males. Two-third (65%) of the patients and majority of the caregivers (87.5%) were married. Most of the patients (79.5%) and caregivers (73.5%) had received at least 10 years of formal education. More than half (53.5%) of the patients were housewives or unemployed, whereas two third (63.5%) of the caregivers were employed. Three fourth (76.5%) of the study sample came from an urban background. About half (48%) of the caregivers were spouse of the patients and one-third (35%) were parents. Minority (17%) of the caregivers had relationship other than the spouse or parent with the patient. The diagnostic distribution of the patient included in the study was psychotic disorders (37%), affective disorders (39.5%) and anxiety, stress and neurotic disorders (23.5%).
All patients were outpatients at the time of assessment. Average duration of illnesses was more than 2 years. All patients were on psychotropic medications including antipsychotics, antidepressants, mood stabilizers, anticholinergics and sedative hypnotics.
Attitude toward psychotropic medications patients and family caregivers
The responses on different attitude items, the total scores and scores on positive and negative attitude items among patients and family caregivers are depicted in Table 1.
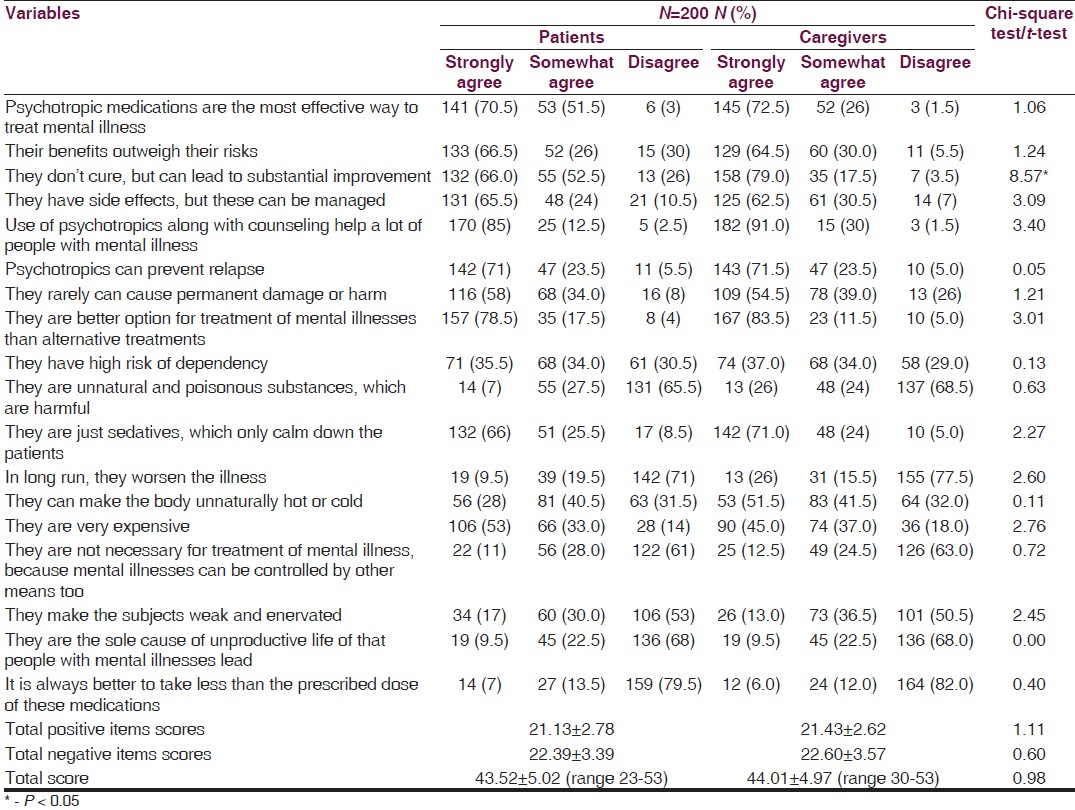
As shown in Table 1, on the 8 items assessing positive attitude toward psychotropics, responses of 58-78.5% of patients and 54.5-83.5% of caregivers reflected favorable attitude toward psychotropics. With regards to the 10 items assessing the negative attitude toward psychotropics, responses of 8.5-79.5% of patients and 5-82% of caregivers reflected that they had favorable attitude toward psychotropics.
The mean total score of patients was 43.52 ± 5.02 (range 23-53) and that of caregivers was 44.01 ± 4.97 (range 30-53), out of the maximum obtainable score of 54.
Mean weighted positive attitudes scores (obtained by dividing the total raw score by total number of items assessing the positive attitude, i.e. 8) for patients was 2.64 ± 0.34 (range 1.38-3), while mean weighted negative attitudes scores (obtained by dividing the total raw score by total number of items assessing the negative attitude, i.e. 10) was 2.23 ± 0.33 (range 1-3). This indicated that positive and negative attitudes toward psychotropic medications were equally prevalent among patients. Similarly, for caregivers mean weighted positive attitudes scores was 2.67 ± 0.32 (range 1.62-3), while mean weighted negative attitudes scores was 2.25 ± 0.353 (range 1-2.9), which also indicated that caregivers had an equal share of both positive and negative attitudes toward psychotropic medications.
Comparisons of attitudes between patients and caregivers revealed differences only on one item, i.e. psychotropics “Don’t cure, but lead to substantial improvement”. Thus, attitudes toward medications were similar among patients and their family caregivers.
Factor analysis of attitudes toward psychotropic medications among patients and family caregivers
Separate factor analyses were run for the data generated from the patients and the caregivers. Additionally, the final factor analysis included data of both patients and the caregivers. The details of the various factor analyses are given in [Tables 2 and 3]. In all the factor analyses, the initial unrotated factor analysis yielded a five-factor structure, which explained 53.59% to 54.73% of variance. The scree plot for the factor analysis of the scale based on responses of patients is depicted in the accompanying figure.


Factor solutions
Factor loadings, the total variance explained by the different numbers of factors, the Scree plot [Figure 1] and previous literature were all used to determine the factor solutions that provided best fit for the data. The two-factor solution (positive and negative attitude factors) was in keeping with many of the earlier studies on attitudes with the DAI.[63233] However, the variance explained by the two-factor solution was the least.
There was very little difference between the loadings on different factors in the three-, four-, and five factor solutions. The scree plots appeared to tail off at the four or five factors. Studies of the DAI have also yielded between three to seven factors,[183334] while a three to five factor structure has also been proposed for the ROMI scale,[19] and a three factor solution has been proposed for the ANT questionnaire.[20] Therefore, a four-factor solution was also considered as ideal fit for the data.

- Scree plot showing the factor analysis solution for the data on attitude toward psychotropics
Details of factor loadings for the two-factor solution have been included in Table 3, and those for the four-factor solution have been depicted in Table 4.
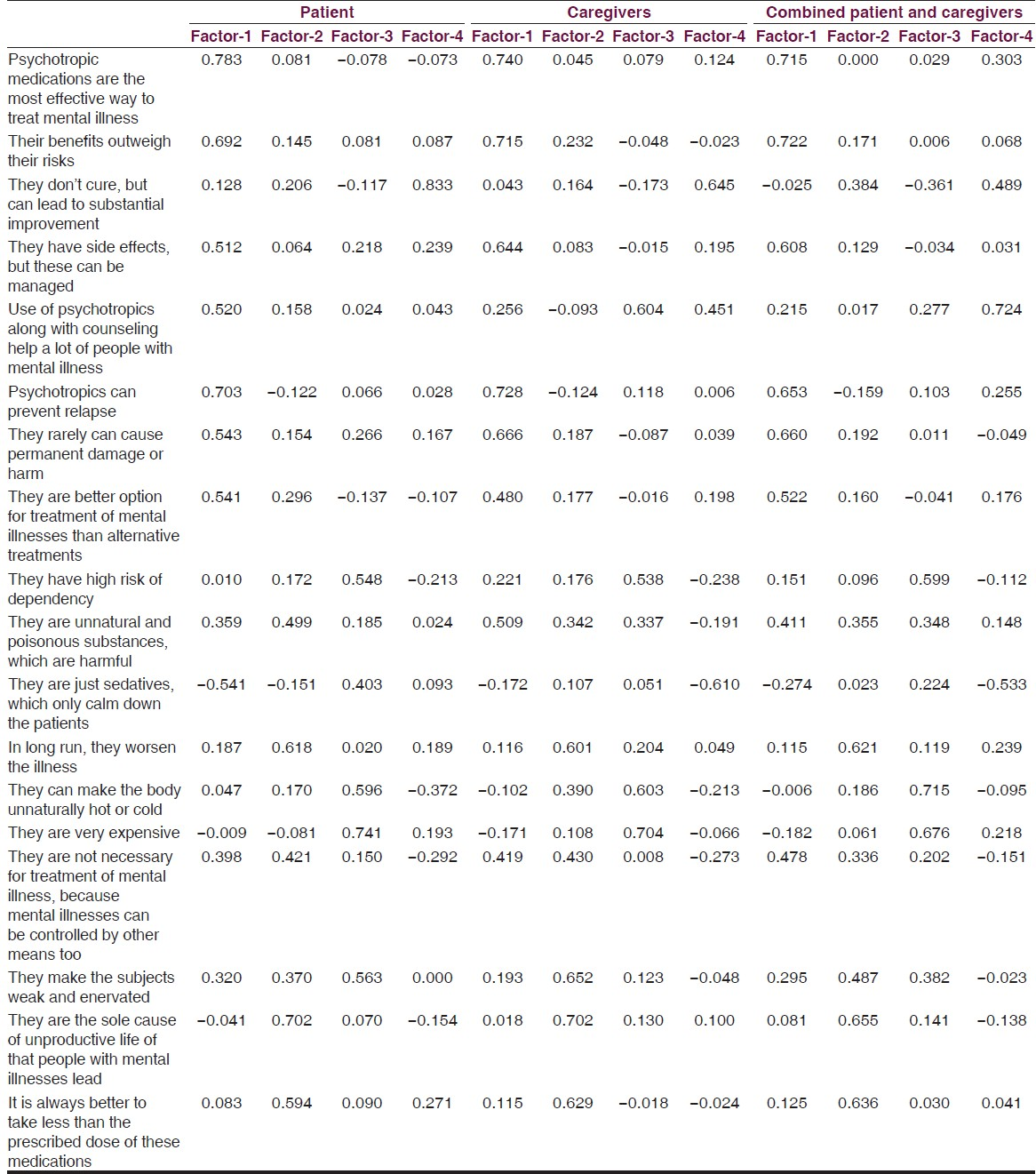
The two-factor solution
In the two-factor structure for patients, factor one comprised of items 1 to 8, except item 3, which though loaded on to factor one, just fell short of the cut-off of 0.40. In addition, item 11 demonstrated an inverse loading on this factor. Thus, factor one appeared to be a “positive attitudes” factor. However, there were two important discrepancies. Item 10 (“Psychotropic medications are unnatural and poisonous substances, which are harmful”), which reflected negative attitudes also loaded on to factor one. Item 15 (“Psychotropic medications are not necessary for treatment of mental illness, because mental illnesses can be controlled by other means too”), which also reflected negative attitudes loaded on to both factors, though its loading on factor one was somewhat greater. It was not clear why these two items should load on to factor one, which essentially comprised of positive attitudes. It is possible that there was some ambiguity in the wording of these items, which led to these discrepant loadings. Factor two comprised of four items (items 9, 10, 16 and 17), which all reflected negative attitudes. Thus, factor two was the “negative attitudes” factor.
This positive (factor one) and negative (factor two) attitudes distinction was more apparent in the case of caregivers with all positive attitude items (except item 3 and 5), and all negative attitude items (except item 11) loading on to factor one and two respectively.
However, this positive-negative attitudes distinction was best illustrated by the results of the factor analysis of the combined sample of 200 patients and 200 caregivers. In this analysis, factor one comprised of all the positive attitude items (from item 1 to item 8) and the inverse of a negative attitude item (item 11), while factor two comprised of all negative attitude items, except item 11.
The four-factor solution
In the four-factor solution for patients, factor one comprised of all items reflecting positive attitudes from item 1 to item 8, except item 3, which loaded separately on to factor four. Analysis of individual items in factors one and four appeared to indicate that a risk-benefit approach was being followed by patients, in which the benefits of medication was contrasted with the risks to arrive at a positive attitude regarding medication. Factors two and three both reflected negative attitudes. Factor two was comprised of items that focused on harm caused by medications (items 10, 12, 17 and 18), and one item reflecting the lack of necessity for these medications (item 15 - “Psychotropic medications are not necessary for treatment of mental illness, because mental illnesses can be controlled by other means too”). Factor three was exclusively comprised of items that reflected the harm caused by these medications. Moreover, the items comprising this factor also possibly reflected common culturally derived attitudes toward allopathic medications, since the items focused on the risk of dependency (item 9), medications making the body unnaturally hot or cold (tem 13), or draining energy and causing weakness (item 16), and on medications being very expensive (item 14).
Among caregivers these four factors were again replicated with some minor differences. For example item 10, which reflected negative attitudes loaded on to factor one, and factor 5, which reflected positive attitudes loaded both on to factor three and factor four. Apart from these discrepancies the factor structure was essentially similar to that obtained among patients with factors one and four as positive attitude factors, derived from a risk-benefit approach that favored medications, and factors two and three being negative attitude factors, which focused on concerns regarding medications such as potential harm, expense and lack of necessity.
The results also indicated that the four-factor structure was the best fit for the data obtained from the combined sample of 200 patients and 200 caregivers.
Discussion
The construct of attitudes to psychotropic medication seems to represent a final, common pathway toward medication adherence. It encapsulates the patient's weighing of many factors that lead him/her to agree to take medications.[635] Different social-cognitive and psychological models have been used to explain the phenomenon of adherence.[45] These models provide a framework for understanding the factors that determine adherence behavior. The model most commonly employed to explain treatment adherence is the Health Belief Model.[36] The model consists of four principal beliefs, which determine attitudes to medication taking including perceived benefits of treatment (symptom reduction), perceived barriers to treatment (e.g. stigma, side-effects), perceived susceptibility to illness or relapse in the absence of treatment, and perceived severity of the outcome (negative consequences of relapse). Additional factors include self-efficacy, and either internal (e.g. prodromal symptoms) or external cues (e.g. family support), which prompt the patient to adhere to medications. The decision to take medication is a result of weighing perceived benefits against the perceived risks of illness and costs of treatment. Adherence is thought to be most likely if the threat of illness (i.e. susceptibility and severity) is believed to be high, and the perceived benefits exceed the barriers of medication adherence.[6373839] Another model, which attempts to explain patients’ attitudes and medication taking behavior is the Necessity-Concerns Framework.[540] This suggests that the patient's decision to begin and continue treatment is influenced by their beliefs about their personal need for treatment (necessity beliefs) relative to their concerns about a range of potential adverse effects of the treatment (concern beliefs).
The results of the factor analysis of attitudes in the current study can be viewed in the context of these models. Firstly, in the simpler two-factor structure of attitudes, they could be conveniently grouped into positive and negative attitudes. Studies with the DAI have also yielded a similar two-factor structure consisting of a positive and a negative attitudes factor, both with the 10-item,[6] and the 30-item versions.[32] Even when more than two factors have been elicited with the 30-item version, the positive and negative factors appear to be the most robust ones, and explain a major part of the variance.[1833] However, the four-factor structure of attitudes appeared to provide a more comprehensive solution to how attitudes might be formed among patients and their family caregivers. Factors one and four in the four-factor solution still reflected positive attitudes, but appeared to portray a risk-benefit approach on the part of the patients, in which benefits such as the efficacy of psychotropic medications in treating mental illnesses and preventing relapse, and medications being better than other options were being contrasted with the risks of side effects and permanent damage or harm. This was thus in keeping with the constructs of the Health Belief model and the Necessity-Concerns Framework.[637383940] Factors two and three both represented negative attitudes toward psychotropic medications, and were mainly focused on the harm or damage caused by such medications, or other barriers such as cost. One item in factor three ("Medications are not necessary for treatment of mental illness, because these can be controlled by other means too") also appeared to reflect the lack of necessity for taking psychotropic medications. Of note was the fact that both these negative attitude factors were comprised of attitudes, which appeared to be culturally determined. For example, the belief that psychotropics are unnatural and poisonous substances or that they make the body unnaturally hot or cold, and weaken or enervate patients, are all commonly held cultural beliefs. According to all social-cognitive and psychological models of adherence, the environment, including culture plays a significant role in influencing attitudes toward medication.[41] Cultural influences consist of explanatory models of illness causation, and beliefs regarding treatment, such as the preference for indigenous treatments over psychotropic medications.[4142] However, cultural aspects of attitudes toward psychotropic medications have perhaps not been explored as comprehensively as some of the other factors influencing attitudes.[42]
Two more findings of this study are of some relevance. Firstly, positive and negative attitudes toward psychotropic medications were equally prevalent among patients of this study and their caregivers. Results of earlier studies in this regard have been mixed. For example, some studies which have examined patients’ attitudes toward antipsychotics have reported predominantly positive attitudes toward medications among them,[68344344] while others have indicated that negative attitudes to antipsychotics are also very common.[1345] Secondly, comparisons of attitudes toward psychotropic medications between patients and family caregivers did not reveal any significant differences in the current study, except on one item. The factor structures found among both patients and caregivers were also largely similar. Very few studies have compared attitudes toward psychotropic medications among patients and caregivers. In some of these studies relatives have demonstrated more positive attitudes toward psychotropic medications than patients.[142546] This has been attributed to the fact that family caregivers do not suffer from the ill effects of the illness, are more aware about the illness and do not have to endure adverse effects of medications. This could lead to more positive attitudes toward psychotropic medications among them.[25] However, other studies have found that even caregivers had a rather negative attitude toward pharmacological treatment of psychiatric disorders.[134748] In this case it has been proposed that this negative perception of caregivers derives from both public opinion and the media, which often support the view that psychotropic medications involve an element of coercion and cause harm.[13] The fact that there was no difference in attitudes toward medications between patients and their family caregivers of this study may suggest that societal opinion or cultural factors are more influential in shaping the perceptions of patients and caregivers both, rather than factors related to the illness such as insight or awareness, or concerns about side effects such as harm or expense.
The findings of this study have to be considered in the light of its methodological limitations. Though the study sample included a large number of patients with diverse diagnoses and their caregivers, they were all from a single center. Moreover, they were all outpatients with relatively chronic and stable course of illnesses. The findings can thus not be readily generalized to other patient populations, such as acutely ill or hospitalized patients, or those attending community treatment facilities. The scale used to measure attitudes was a preliminary one and might not have assessed other prevalent attitudes. Less than half the variance in attitudes was explained by the factors derived from the data, which indicates that other factors, not measured by the scale could explain the formation of attitudes toward medications among patients and their caregivers.
However, despite these methodological problems the findings indicate that in line with the social-cognitive and psychological models, attitudes of patients with chronic psychiatric disorders and their caregivers toward psychotropic medications appear to be shaped by factors such as perceived efficacy or benefit from medicines, the necessity for taking treatment and concerns such as side effects, harm or expense. Since positive attitudes toward medications among patients and caregivers are likely to enhance adherence to medications, these aspects of attitudes deserve further attention.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- How often do patients with psychosis fail to adhere to treatment programmes. A systematic review? Psychol Med. 2003;33:1149-60.
- [Google Scholar]
- Antidepressant adherence: Are patients taking their medications? Innov Clin Neurosci. 2012;9:41-6.
- [Google Scholar]
- Adherence to long term therapies: Evidence for action. Geneva: World Health Organization; 2003. ISBN 9241545992 (NLM classification: W 85)
- Predicting treatment adherence: An overview of theoretical models. In: Myers LB, Midence K, eds. Adherence to Treatment in Medical Conditions. Amsterdam: Harwood Academic; 1998. p. :25-50.
- [Google Scholar]
- Attitudes of schizophrenia outpatients toward psychiatric medications: Relationship to clinical variables and insight. J Clin Psychiatry. 2004;65:1372-6.
- [Google Scholar]
- The content and context of compliance. Int Clin Psychopharmacol. 1995;9(Suppl 5):41-50.
- [Google Scholar]
- Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry. 2004;19:415-22.
- [Google Scholar]
- Effect of patient and family insight on compliance of schizophrenic patients. J Clin Pharmacol. 1997;37:147-54.
- [Google Scholar]
- Compliance in schizophrenia: Psychopathology, side effects, and patients’ attitudes toward the illness and medication. J Clin Psychiatry. 2004;65:1211-8.
- [Google Scholar]
- Predictors of poor adherence to medication among patients with first-episode schizophrenia-spectrum disorder. Early Interv Psychiatry. 2009;3:66-74.
- [Google Scholar]
- Understanding adherence to neuroleptic treatment in schizophrenia. Psychiatry Res. 2004;126:43-9.
- [Google Scholar]
- Subjective experience and mental side-effects of antipsychotic treatment. Acta Psychiatr Scand Suppl. 1999;395:113-7.
- [Google Scholar]
- Attitudes towards long-acting depot antipsychotics: A survey of patients, relatives and psychiatrists. Psychiatry Res. 2010;175:58-62.
- [Google Scholar]
- A scale for detection of negative attitudes towards medication among relatives of schizophrenic patients. Acta Psychiatr Scand. 1985;71:186-9.
- [Google Scholar]
- From burden to empowerment: The journey of family caregivers in India. In: Sartorius N, Leff J, Lo’pez-Ibor JJ, Okasha A, eds. Families and Mental Disorders. Chichester: John Wiley and Sons Ltd; 2005. p. :259-90.
- [Google Scholar]
- A self-report scale predictive of drug compliance in schizophrenics: Reliability and discriminative validity. Psychol Med. 1983;13:177-83.
- [Google Scholar]
- Rating of medication influences (ROMI) scale in schizophrenia. Schizophr Bull. 1994;20:297-310.
- [Google Scholar]
- Attitudes towards neuroleptic treatment: Reliability and validity of the attitudes towards neuroleptic treatment (ANT) questionnaire. Schizophr Res. 2000;45:223-34.
- [Google Scholar]
- Development of an antidepressant compliance questionnaire. Acta Psychiatr Scand. 2004;110:201-7.
- [Google Scholar]
- Risk factors for drug nonadherence in antidepressant-treated patients and implications of pharmacist adherence instructions for adherence improvement. Patient Prefer Adherence. 2012;6:863-9.
- [Google Scholar]
- Short-term clinical stability and lack of insight are associated with a negative attitude towards antipsychotic treatment at discharge in patients with schizophrenia and bipolar disorder. Patient Prefer Adherence. 2012;6:623-9.
- [Google Scholar]
- Adherence and continuation of treatment with first- and second-generation antipsychotics in schizophrenia. Indian J Psychol Med. 2014;36:33-9.
- [Google Scholar]
- Attitude towards second-generation antipsychotics among patients with schizophrenia and their relatives. Hum Psychopharmacol. 2013;28:457-65.
- [Google Scholar]
- Attitude towards antipsychotics among patients with schizophrenia on first- or second-generation medications. Indian J Psychol Med. 2014;36:288-93.
- [Google Scholar]
- Benefits and risks of psychotropic medication in the eyes of the general public: Results of a survey in the Federal Republic of Germany. Pharmacopsychiatry. 1993;26:114-20.
- [Google Scholar]
- Attitudes to antipsychotic drugs and their side effects: A comparison between general practitioners and the general population. BMC Psychiatry. 2006;6:42.
- [Google Scholar]
- Process of Translation and Adaptation of Instruments. Available from: http://www.who.int/substance_abuse/research_tools/translation/en/
- Statistical Package for Social Scientists version 14 (SPSS-14, Chicago, IL, USA).
- Principal Component Analysis (Springer Series in Statistics) (2nd ed). New York: Springer; 2002.
- Attitude of patients with schizophrenia towards antipsychotic therapy. Acta Medico-Biotechnica. 2010;3:35-42.
- [Google Scholar]
- The conceptual adequacy of the drug attitude inventory for measuring youth attitudes toward psychotropic medications: A mixed methods evaluation. Phd Dissertation. CASE Western Reserve University thesis
- [Google Scholar]
- Attitudes toward antipsychotics among outpatient clinic attendees with schizophrenia. J Clin Psychiatry. 2002;63:49-53.
- [Google Scholar]
- A prototype approach toward antipsychotic medication adherence in schizophrenia. Harv Rev Psychiatry. 2009;17:35-40.
- [Google Scholar]
- The health belief model: Explaining health behavior through expectancies. In: Glanz K, Lewis FM, Rimer BK, eds. Health Behaviour and Health Education. San Francisco: Josey Bass; 1990. p. :39-62.
- [Google Scholar]
- Predicting medication adherence in severe mental disorders. Acta Psychiatr Scand. 2000;101:119-24.
- [Google Scholar]
- Determinants of medication compliance in schizophrenia: Empirical and clinical findings. Schizophr Bull. 1997;23:637-51.
- [Google Scholar]
- Adherence to antipsychotic medications. J Clin Psychiatry. 1999;60(Suppl 21):25-30.
- [Google Scholar]
- Understanding medication non-adherence in bipolar disorders using a Necessity-Concerns Framework. J Affect Disord. 2009;116:51-5.
- [Google Scholar]
- Factors affecting therapeutic compliance: A review from the patient's perspective. Ther Clin Risk Manag. 2008;4:269-86.
- [Google Scholar]
- Medication non-adherence in the elderly: How big is the problem? Drugs Aging. 2004;21:793-811.
- [Google Scholar]
- Attitude towards antipsychotics among out-patients with schizophrenia in Nigeria. Acta Psychiatr Scand. 2006;113:207-11.
- [Google Scholar]
- Correlations of attitudes toward antipsychotic drugs with insight and objective psychopathology in schizophrenia. Compr Psychiatry. 2008;49:170-6.
- [Google Scholar]
- Attitudes toward medication change among chronically impaired psychiatric patients. Am J Psychiatry. 1981;138:801-3.
- [Google Scholar]
- Attitudes and subjective reasons of medication compliance and noncompliance among outpatients with schizophrenia in India. Int J Epidemiol 2008:7.
- [Google Scholar]
- Lay beliefs about schizophrenic disorder: The results of a population survey in Germany. Acta Psychiatr Scand Suppl. 1994;382:39-45.
- [Google Scholar]
- Attitudes toward medication in inpatients with schizophrenia: A cluster analytic approach. Psychiatry Res. 2008;158:324-34.
- [Google Scholar]






