Translate this page into:
Association of Cognitive and Noncognitive Symptoms of Delirium: A Study from Consultation-liaison Psychiatry Set-up
Address for correspondence: Dr. Sandeep Grover, Department of Psychiatry, Postgraduate Institute of Medical Education and Research, Chandigarh - 160 012, India. E-mail: drsandeepg2002@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aims:
This study aims to evaluate the cognitive functions of patients with delirium using Hindi Mental Status Examination (HMSE), to study the correlation of cognitive functions assessed by HMSE with noncognitive symptoms as assessed using Delirium Rating Scale-Revised 1998 (DRS-R-98) and to study the association of cognitive functions assessed using HMSE and DRS-R98.
Methods:
A total of 76 consecutive patients fulfilling the diagnosis of delirium were evaluated on DRS-R-98, HMSE, and Short Informant Questionnaire on Cognitive Decline in the Elderly (retrospective IQCODE).
Results:
The mean DRS-R-98 score 33.9 (standard deviation [SD] - 7.2) and the mean DRS-R-98 severity score was 25.9 (SD - 7.2). The mean score on HMSE was 19.3 (7.98). There were significant correlations of all the domains of HMSE with DRS-R-98 total score, DRS-R-98 severity score, DRS-R-98 cognitive subscale score, DRS-R-98 noncognitive domain subscale score, and DRS severity score without attention score. When the association of each item of DRS-R-98 and HMSE was evaluated, except for the items of delusions, lability of affect and motor retardation, there were significant negative association between all the items of DRS-R-98 and HMSE, indicating that higher severity of cognitive symptoms as assessed on HMSE is associated with higher severity of all the cognitive symptoms and most of the noncognitive symptoms as assessed by DRS-R-98.
Conclusion:
The present study suggests that attention deficits in patients with delirium influence the severity of cognitive and noncognitive symptoms of delirium. Further, the present study suggests an increase in the severity of cognitive symptoms in other domains is also associated with an increase in the severity of noncognitive symptoms of delirium.
Keywords
Cognitive symptoms
correlation
delirium
noncognitive symptoms
INTRODUCTION
Delirium is an acute complex neuropsychiatric condition, which is highly prevalent in inpatient treatment setting and is considered to lead to many adverse outcomes in medically ill patients.[1] The symptoms of delirium are generally categorized into cognitive and noncognitive domains. Although many studies have evaluated the phenomenology of delirium, very few studies have evaluated the relationship of cognitive and noncognitive symptoms. Existing data suggest that noncognitive features dominate the clinical picture during the early stages of delirium while cognitive impairments peak after 1 week and dominate the clinical picture thereafter.[2] In another study, the authors evaluated patients with delirium on Mini-Mental Status Examination (MMSE), Delirium Rating Scale (DRS), and Memorial Delirium Assessment Scale (MDAS) and reported high correlations between individual MDAS items and the MMSE total score when compared with the correlation between individual DRS items and the MMSE score.[3] Noncognitive items (e.g., perceptual disturbances, sleep-wake cycle disturbances) of both scales and certain specific DRS items (i.e., lability of mood, physical disorder) showed lower correlations with the MMSE.[3] A previous study from our center evaluated the patients of Delirium Rating Scale-Revised 1998 (DRS-R-98) and cognitive test for delirium (CTD) and showed that patients experiencing higher attention deficits had higher dysfunction on all other domains of cognition on CTD. In terms of the relationship between cognitive and noncognitive functions, it was seen that cognitive functions as assessed on CTD correlated positively with and total DRS-R-98 score, DRS-R-98 severity score, and DRS-R-98 severity score without the attention item score. However, there were few correlations between various domains scores and CTD total scores with cognitive domain score of DRS-R-98 (items 9–13) and noncognitive symptom total score of DRS-R-98 (items 1–8).[4]
Various instruments have been used to assess the symptom profile of patients with delirium.[5] The commonly used instrument for assessment of cognitive functions includes Mini-Mental State Examination (MMSE)[6] and CTD[7] and the cognitive subscale of delirium rating scale-revised 1998 version.[8] However, the use of MMSE is criticized for being only useful in cooperative patients, its practice effect and influence of level of education. On the other hand, CTD is considered to be more comprehensive which can be used in nonverbal intensive care unit patients. However, its use requires slightly higher level of cooperation of the patient which makes it use difficult in routine clinical situations. In view of these, there is always an effort to evaluate the cognitive functions of patients with delirium using more standardized instruments. Accordingly, there is a need to understand the suitability of instrument which can be used to assess cognitive functions among patients with delirium.
Studies done in India involving patients of dementia also suggest that MMSE is not a good instrument to evaluate cognitive functions among Indians, especially those who are illiterate.[9] Considering these limitations, researchers have developed Hindi Mental Status Examination (HMSE), which has been shown to be possibly more useful for illiterate subjects.[10] However, the usefulness of HMSE in delirium patients has not been evaluated. Accordingly, the aims of this study were: (1) To evaluate the cognitive functions of patients with delirium using HMSE; (2) to evaluate the correlation of cognitive functions assessed by HMSE with noncognitive symptoms as assessed using DRS-R-98; (3) to study the association of cognitive functions assessed using HMSE and DRS-R-98.
METHODS
The study was approved by the Institute Ethics Committee. Participants were recruited after obtaining written informed consent from the family caregivers, staying with the patients during the inpatient stay.
All the patients referred to psychiatry consultation-liaison (CL) psychiatric services during the study period of August 2014 to December 2014 and diagnosed with delirium were eligible for this study. For inclusion into the study, the patients were required to be aged 15 or more and not on any antipsychotic medications before assessment. Patients with loss of vision, hearing impairment, aphasia, axis-I psychiatric disorders were excluded from this study. Similarly, those with preexisting cognitive deficits were also excluded. The presence of preexisting cognitive deficits was ruled out on the basis of Short Informant Questionnaire on Cognitive Decline in the Elderly (retrospective IQCODE).[11] Those admitted to the intensive care units and on mechanical ventilation were excluded from this study.
Instruments
Delirium Rating Scale-Revised 1998
This scale is used for comprehensive assessment of cognitive and noncognitive symptoms of delirium. It has 13 items for rating of severity of illness and 3 diagnostic items. Each severity item is rated on a 4 point scale (0–3), and the mean severity score ranges from 0 to 39. It has been shown to have high inter-rater reliability, sensitivity, and specificity.[10]
Hindi Mental Status Examination
It is based on MMSE and assesses the same domains of cognitive functions as MMSE,[11] however, the items are designed by taking the literacy level and cultural issues into account. It has been used by many researchers for screening patients for dementia and also has been used in patients with delirium[12] but the authors did not present the detail scores.
Short Informant Questionnaire on Cognitive Decline in the Elderly (retrospective IQCODE)
It is a 16-item instrument which on the basis of the input provided by a key relative determines the cognitive status of the patient for the specified period (6 months for this study). Each item is rated on a 5-point scale with score 3 indicating no change, and scores higher than 3 indicating decline in cognitive functioning and lower scores indicates improvement in cognitive functions. To obtain the final score, score obtained for all items is added and divided by 16. A mean score >3.31–3.38 is considered to be an indicator of cognitive decline.[13]
Family carers of the patients diagnosed with delirium by the CL psychiatry team were approached and explained about the purpose of the study. Initially, the consenting caregivers were interviewed to confirm in the patient the diagnosis of delirium as per Diagnostic and Statistical Manual of Mental Disorders-4th edition text revision criteria and to rule out other psychiatric disorders. Then the patients with confirmed diagnosis of delirium were evaluated on short IQCODE to rule out preexisting cognitive deficits. Those without preexiting cognitive deficits were evaluated further on DRS-R-98 and HMSE. All the assessment was done over a period of 1 h with breaks in between.
Statistical analyses
Data were analyzed using SPSS-14 (SPSS for Windows, Version 14.0. Chicago, SPSS Inc.). For descriptive purposes mean, standard deviation (SD), frequency and percentages were calculated. Associations were studied using Pearson's product moment correlation and Spearman rank correlation.
RESULTS
The study included 76 consecutive patients fulfilling the selection criteria. The mean age of the study participants was 47.10 (SD - 16.5) years with a range of 15–75 years. About one-fifth (n = 18; 23.68%) of the study sample was aged 60 years or more. The majority of the participants were male (n = 55; 72.4%) and the mean duration of delirium at the time of assessment was 2.23 (SD - 3.1) days.
The symptom profile as per DRS-R-98 is shown in Table 1. All the patients had sleep-wake cycle disturbances, acute onset of illness, fluctuations of symptoms, and presence of a physical disorder. Motor retardation was the least common symptom. The mean DRS-R-98 score 33.9 (SD - 7.2) and the mean DRS-R-98 severity score was 25.9 (SD - 7.2). The mean score of noncognitive domain was more than mean score of cognitive domain.
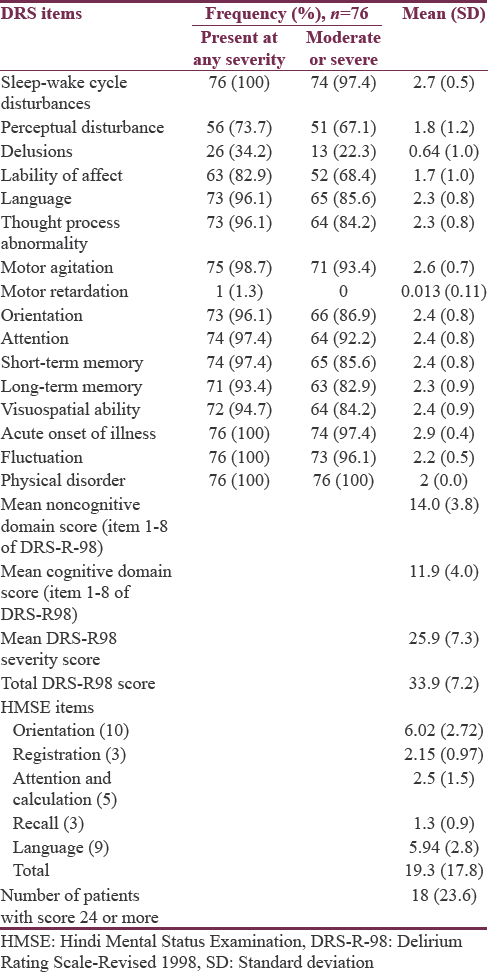
The mean score on HMSE was 19.3 (7.98). Cognitive deficits were seen in all the domains assessed.
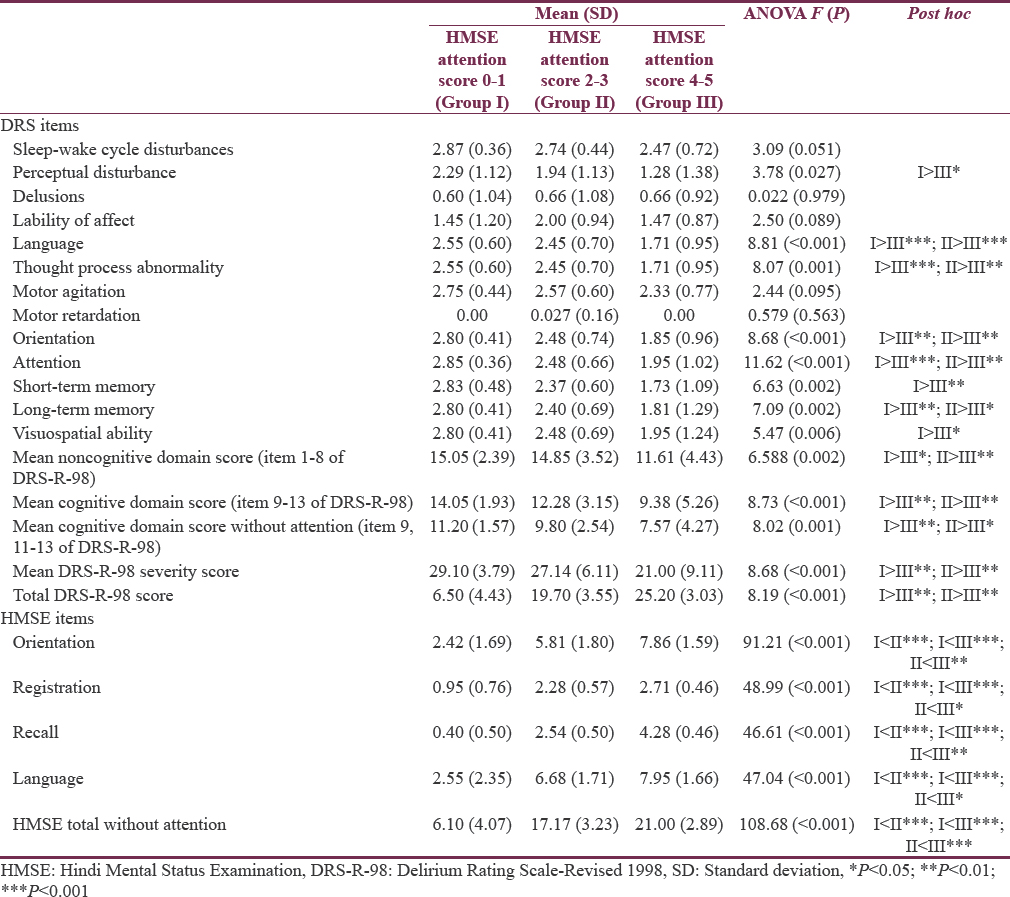
As attention is considered to be the “core” cognitive symptoms of delirium, based on the attention scores obtained on HMSE, the study sample was divided into three groups, i.e., those who scores 0–1, 2–3, and 4–5 and the three groups were compared for the DRS-R-98 score and scores in the other domains of HMSE [Table 2].
Association of cognitive functions with noncognitive symptoms of delirium
As shown in Table 3, there were significant correlations of all the domains of HMSE with DRS-R-98 total score, DRS-R-98 severity score, DRS-R-98 cognitive subscale score, DRS-R-98 noncognitive domain subscale score and DRS-R-98 severity score without attention score.
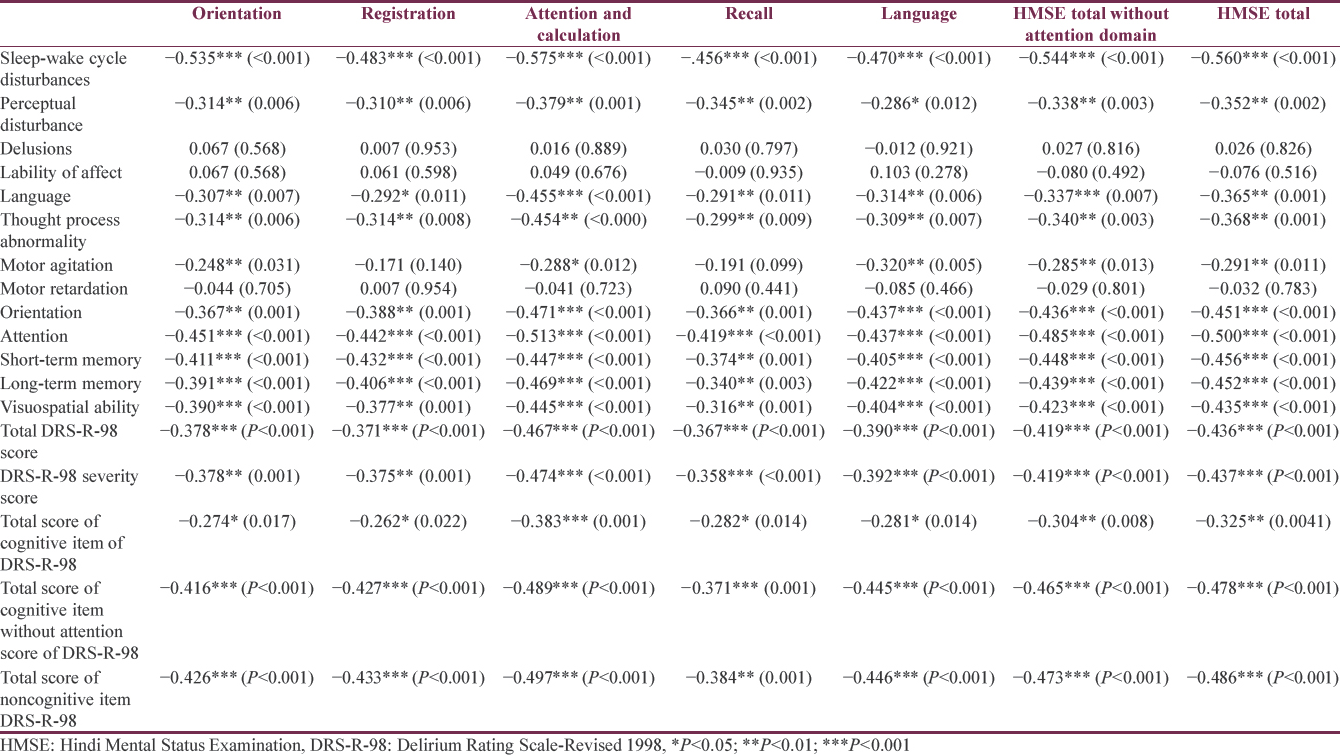
When the association of each item of DRS-R-98 and HMSE was evaluated, except for the items of delusions, lability of affect and motor retardation, there were significant negative association between all the items of DRS-R-98 and HMSE, indicating that higher severity of cognitive symptoms as assessed on HMSE is associated with higher severity of all the cognitive symptoms and most of the noncognitive symptoms as assessed by DRS-R-98.
DISCUSSION
Few studies have evaluated the association of cognitive and noncognitive symptoms of delirium. The present study utilized DRS-R-98 and HMSE.
The sample included in the present study is similar to the previous studies from CL psychiatry set-up from India, in terms of mean age, percentage of elderly, gender distribution, mean duration of education, duration of delirium, and mean number of associated etiologies[14151617] suggesting that the study sample was representative.
The DRS-R-98 symptom profile of the study sample is also similar to previous studies from this center, both in terms of frequency and severity of symptoms[1415161718] and literature from other parts of the world.[19]
In terms of associations of various symptoms domains, considering the fact that attention is the most important cognitive dysfunction in patients with delirium, we evaluated the correlation between attention and other cognitive functions as assessed by HMSE. It was seen that there was positive association between attention and all other cognitive domains as assessed by HMSE, suggesting that higher attention deficits are associated with higher dysfunction on all other domains. Previous studies have also evaluated the similar associations, however, using CTD and have reported similar positive association.[420] In terms of the influence of attention as assessed by using HMSE on other symptoms of delirium as assessed by DRS-R-98, findings of the present study suggest that attention has a significant influence on most of the other symptoms of delirium too, with higher level of attention associated with higher level of dysfunctions in other symptom domains. Previous studies which have evaluated the influence of attention as assessed by CTD are not conclusive. One study from the United Kingdom, reported significant influence of attention deficits as assessed by CTD on sleep-wake cycle disturbances, language, through process disturbance, orientation, short-term memory, long-term memory, visuospatial abnormalities, and total DRS-R-98 scores.[21] However, the previous study done at our center using the similar scales used in the study from the United Kingdom did not find such associations except for association of attention and motor retardation. Accordingly, it can be said that as suggested in previous study from the United Kingdom, attention deficits in patients of delirium influences other symptoms domain too. More clear influence of attention deficit noted in the present study could be due to use of a validated and culturally sensitive instrument to assess cognitive functions. This also possibly suggests that in Indian set-up HMSE may be a better instrument to assess cognitive functions than CTD.
When the association of HMSE and each item of DRS-R-98, DRS-R-98 total score, DRS-R-98 severity score, DRS-R-98 cognitive and noncognitive domains were evaluated, there was significant association of all the domains of cognitive functions assessed by HMSE with most of the DRS-R-98 items and all the total scores. The findings of an association of total HMSE score and various total scores of DRS-R-98 suggests that increasing severity of delirium is associated with higher level of cognitive dysfunction. These findings are supported by the previous studies too which have evaluated similar associations.[421] However, the previous study did not find such clear associations for each item of DRS-R-98 as noted in this study.[421] In contrast to the previous study from India which did not find an association between cognitive domains of CTD and DRS-R-98, the present study showed that there was a significant association between the HMSE domains and various cognitive functions as assessed using DRS-R-98. This finding also possibly suggests that HMSE may be better instrument for evaluation of cognitive functions in the Indian set-up.
The present study has certain limitations, which include cross-sectional evaluation of the patients, small sample size and inclusion of etiologically heterogeneous group. As the study did not include patients admitted to intensive care units, the findings cannot be generalized to this group of patients. Assessment of cognitive functions in the present study was limited to the use of HMSE and DRS-R-98. Accordingly, it cannot be conclusively suggested that HMSE is better than other instruments for assessment of cognitive functions in patients of delirium. Future studies must attempt to overcome these limitations. Future studies also must compare the use of various instruments such as MMSE, HMSE, CTD, and Montreal Cognitive Assessment for assessment of cognitive functions among patients with delirium.
CONCLUSION
The present study suggests that attention deficits in patients with delirium influence the severity of cognitive and noncognitive symptoms of delirium. Further, the present study suggests an increase in the severity of cognitive symptoms in other domains is also associated with increase in severity of noncognitive symptoms of delirium. The present study also provides some credence to the fact that HMSE may be a better instrument to assess cognitive functions of patients with delirium in the Indian setting.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Delirium research: Contributions from India. In: Malhotra S, Chakrabarti S, eds. Developments in Psychiatry in India: Clinical, Research and Policy Perspectives. New Delhi: Springer (India) Pvt. Ltd; 2015. p. :463-92.
- [Google Scholar]
- Clinical presentation of delirium in patients undergoing hematopoietic stem cell transplantation. Cancer. 2005;103:810-20.
- [Google Scholar]
- Assessing delirium in cancer patients: The Italian versions of the Delirium Rating Scale and the memorial delirium assessment scale. J Pain Symptom Manage. 2001;21:59-68.
- [Google Scholar]
- Relationship between cognitive and non-cognitive symptoms of delirium. Asian J Psychiatry. 2013;6:106-12.
- [Google Scholar]
- “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189-98.
- [Google Scholar]
- Validation of a cognitive test for delirium in medical ICU patients. Psychosomatics. 1996;37:533-46.
- [Google Scholar]
- Delirium. In: Yudofsky S, Hales R, eds. Textbook of Neuropsychiatry (5th ed). Washington, DC: American Psychiatric Press; 2007. p. :445-517.
- [Google Scholar]
- Applicability of the mini-mental state examination (MMSE) and the Hindi Mental State Examination (HMSE) to the urban elderly in India: A pilot study. Int Psychogeriatr. 2009;21:123-8.
- [Google Scholar]
- Validation of the Delirium Rating Scale-revised-98: Comparison with the delirium rating scale and the cognitive test for delirium. J Neuropsychiatry Clin Neurosci. 2001;13:229-42.
- [Google Scholar]
- A Hindi version of the MMSE: The development of a cognitive screening instrument for a largely illiterate rural elderly population in India. Int J Geriatr Psychiatry. 1995;10:367-77.
- [Google Scholar]
- Evaluation of delirium in elderly: A hospital-based study. Geriatr Gerontol Int. 2011;11:467-73.
- [Google Scholar]
- A short form of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): Development and cross-validation. Psychol Med. 1994;24:145-53.
- [Google Scholar]
- Symptoms of delirium: An exploratory factor analytic study among referred patients. Gen Hosp Psychiatry. 2011;33:377-85.
- [Google Scholar]
- Delirium in elderly people: A study of a psychiatric liaison service in North India. Int Psychogeriatr. 2012;24:117-27.
- [Google Scholar]
- Incidence, Prevalence and Phenomenology of Delirium in Respiratory Intensive Care Unit: A Prospective Study. Thesis Submitted to Post Graduate Institute of Medical Education and Research 2009
- [Google Scholar]
- A factor analytic study of the Delirium Rating Scale-Revised-98 in untreated patients with delirium. J Psychosom Res. 2011;70:473-8.
- [Google Scholar]
- Delirium phenomenology: What can we learn from the symptoms of delirium? J Psychosom Res. 2008;65:215-22.
- [Google Scholar]
- A new data-based motor subtype schema for delirium. J Neuropsychiatry Clin Neurosci. 2008;20:185-93.
- [Google Scholar]
- Phenomenology of delirium. Assessment of 100 adult cases using standardised measures. Br J Psychiatry. 2007;190:135-41.
- [Google Scholar]






