Translate this page into:
Association of Attention-deficit Hyperkinetic Disorder with Alcohol Use Disorders in Fishermen
Address for correspondence: Dr. Balaji Bharadwaj, Department of Psychiatry, Jawaharlal Institute of Postgraduate Medical Education and Research, Ground Floor, Hospital Block, Dhanvantri Nagar, Puducherry - 605 006, India. E-mail: bharadwaj.balaji@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Alcohol use is a widely prevalent problem and poses hazard during work for certain groups such as fishermen. Disorders such as Attention-Deficit/Hyperkinetic Disorder (ADHD) correlate with early onset and greater severity of alcohol use disorders.
Aims:
We planned to study the frequency of ADHD among fishermen in a fishing hamlet of southern India using adult ADHD self-reported scale (ASRS) and correlated with the severity of alcohol use disorder as evidenced by age at initiation of alcohol use, presence of harmful use, or dependence use as defined by Alcohol Use Disorders Identification Test (AUDIT).
Subjects and Methods:
This was a community-based interview using AUDIT questionnaire for severity of alcohol use and the ASRS to detect ADHD.
Results:
The prevalence of adult ADHD among fishermen in this study was 25.7% using the critical items of the ASRS. ADHD was about twice as likely in participants with dependence as those without dependence (odds ratio = 2.10). ADHD was also more likely in participants with onset of use before 30 years of age than others (25.1% vs. 15.4%) (P = 0.27).
Discussion:
We found a high frequency of alcohol use among fishermen (79.8%). However, only 9.9% had alcohol dependence which is higher than the general population (2.3%) in the region. Fishermen with alcohol dependence were twice as likely to have ADHD as those without alcohol dependence.
Conclusion:
In a community-based survey of fishermen, the prevalence of alcohol dependence was about 10%. The presence of alcohol dependence predicted a two times higher likelihood of ADHD among fishermen than those without alcohol dependence.
Keywords
Alcoholism
attention-deficit disorder with hyperactivity
occupational groups
hyperkinetic disorder
INTRODUCTION
According to the World Health Organization's Global Information System on Alcohol and Health,[1] an estimated 40.7% of Indian males have consumed some form of alcohol in their lifetime. Alcohol consumption contributes to about one-half of liver cirrhosis and one-fourth of road traffic accidents suffered by Indian men. The prevalence of alcohol use disorders (including harmful use and dependence) among Indian men was about 4.5%. One of the biological risk factors leading to alcohol use is said to be childhood externalizing spectrum disorders such as attention-deficit hyperkinetic disorder (ADHD) during adolescence.[2] While one-fifth of childhood ADHD persists into adulthood, only one-third of adult ADHD has an early childhood onset.[3] Adult ADHD may be an independent risk factor for early age of development of alcohol use disorders in adults.[4]
We conducted a study of alcohol use among fishermen in a village in southern India. We aimed to study the prevalence of adult ADHD among fishermen and to study the association between the presence of ADHD and alcohol use disorder severity. The hypothesis was that presence of ADHD as detected by the adult ADHD self-reported scale (ASRS) will be associated with greater severity of alcohol use disorder among fishermen. This would be reflected as earlier age at onset of drinking and greater probability of harmful use or dependence to alcohol among fishermen with ADHD compared to fishermen without ADHD.
SUBJECTS AND METHODS
This community-based cross-sectional study was carried out among fisherman in a coastal village of southern India. The total population of the village is around 6000 and most of them were fishermen. Only a small number of villagers are employed in other occupations such as farming and daily labor work. All fishermen above 18 years of age, who were residents of the village and went out to sea for catching fish at least once in the last 3 months, were eligible to participate in the study. Fishermen who were staying in the study setting for a minimum period of 6 months were considered as residents.
Alcohol Use Disorders Identification Test (AUDIT) questionnaire[5] was used to assess the dependence to alcohol among the study participants. It was administered in Tamil by the health-care worker. The AUDIT scores of 0–7 (Zone I) indicates no harmful patterns of use. Scores between 8 and 19 (Zones II and III) indicate harmful or hazardous drinking and scores of 20 or more (Zone IV) indicate probable alcohol dependence in the individual and require specialist referral.
Attention-deficit hyperkinetic disorder (ADHD) among adults was assessed using adult ASRS, an eighteen-item scale that elicits self-reported symptoms of ADHD in adults based on Diagnostic and Statistical Manual–IV criteria for ADHD.[6] It takes about 7 minutes to apply. We used a Tamil version of the scale. The responses are Likert type from “Never,” “Rarely,” “Sometimes,” “Often,” and “Very Often.” The symptoms in six critical questions in the scale consistent with adult onset ADHD, remaining 12 questions serve additional aid in assessing the ADHD. The coding of the scores is from 0 to 4. A cutoff score of 40 on the full version of the ASRS and 14 on the six-item version were taken as suggestive of ADHD. The full version was used in this study because the specific psychometric properties of the scales in the present population are unclear. For analysis, we analyzed the full version as well as the critical items version and used it in further statistical analyses of association as the full version appeared to overestimate ADHD in our study population.
Apart from the Institute Ethical Committee clearance, we also obtained verbal consent from the village leader before the onset of the study. All the fishermen who were registered with the fishermen guild of the locality were approached. After briefly explaining the purpose of the study and procedure, written informed consent was obtained from the individual participants before administration of the questionnaire. The respondents were neither intoxicated nor experiencing withdrawal symptoms at the time of interview to avoid bias in reporting. All the houses were visited up to 3 times in a period of 6 weeks to look for and interview eligible participants.
Statistical analysis
Data were entered in EpiData 3.1 software, Epidata (Version 2.2.2.178) (EpiData Association, Odense, Denmark), and analysis was done using EpiData Analysis software. Continuous variables such as age were expressed as mean and standard deviation. Monthly income was expressed as median and interquartile range as they were following nonnormal distribution. Alcohol use disorders were defined by AUDIT scores as follows: AUDIT 0–7 = no alcohol use disorder, AUDIT 8–20 = alcohol, harmful use, and ADUIT ≥20 = alcohol dependence. The presence or absence of ADHD was coded as binary variable (yes = 1, no = 0) using a cutoff score ≥40 on full-scale ASRS and ≥14 on critical items scale of ASRS. Association of sociodemographic and occupational characteristics with the presence or absence of ADHD was assessed using Chi-square test. Similarly, we used Chi-square test to assess whether the presence of ADHD was associated with alcohol dependence syndrome. A P < 0.05 was considered as statistically significant.
RESULTS
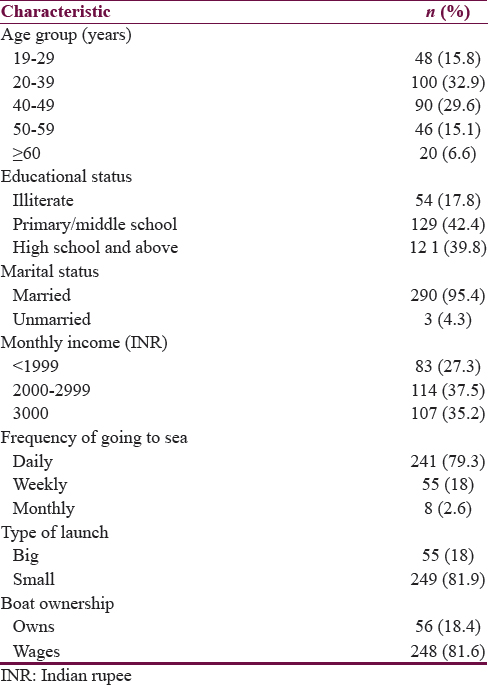
A total of 304 fishermen lived in the area of study. 62.5% (190/304) were between 20 and 49 years of age. Most of them (290/304; 95.4%) were married. A majority of the fishermen (249/304; 81.9%) rented a boat, and the rest were owners of boats. The detailed sociodemographic profile of the study population is depicted in Table 1.
As regards alcohol use, 241/304 (79.3%) of respondents had used alcohol at least once in the last 1 year. A total of 89/304 (29.3%) had no alcohol use disorder. This includes nonusers of alcohol. 185/304 (60.9%) had harmful use of alcohol and 30/304 (9.9%) had dependent use of alcohol.
Using the full-scale ASRS scores, 150/304 (49.3%) had ADHD and 78/304 (25.7%) had ADHD when determined by the critical items of the scale alone.
AUDIT was applied to the 241 participants. They were classified based on AUDIT scores as described under Statistics section. Only 30 (12.5%) of the 241 alcohol users were dependent on alcohol; however, a majority of them, 185 out of 241 (76.7%), had harmful use of alcohol. The remaining 26 out of 241 (10.8%) did not have alcohol use disorders. The 63 participants who did not use alcohol in the last 1 year were also diagnosed to have no alcohol use disorder.
A total of 150 (49.3%) volunteers screened positive for ADHD using the full scale (>40), but only 78 (25.7%) had scored positive for ADHD using the critical items scale (>14) of the ASRS.
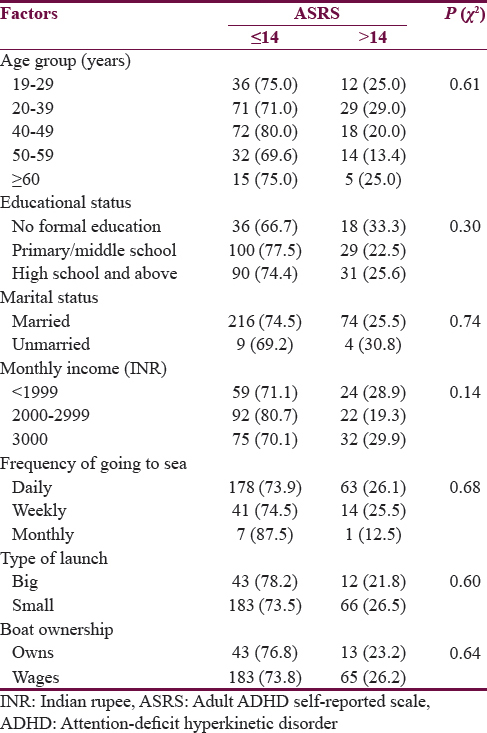
Table 2 depicts the sociodemographic profile of fishermen in relation to the presence or absence of ADHD. None of the parameters were significantly associated with ADHD.
The association of alcohol use parameters with ADHD (as defined by ASRS critical items scale) is depicted in Table 3. Participants with alcohol dependence were more likely to have ADHD (40%) than participants with harmful use (23.2%) (odds ratio [OR] = 2.20; 95% confidence interval [CI] = 0.98–4.93) or no alcohol use disorder (25.8%) (OR = 1.91; 95% CI = 0.80–4.57). When compared to those without alcohol dependence (no alcohol use disorder and alcohol harmful use), we found that those with alcohol dependence had a greater chance of having ADHD (OR = 2.10; 95% CI = 0.96–4.58). However, these differences were not statistically significant (Chi-square test, P = 0.14).
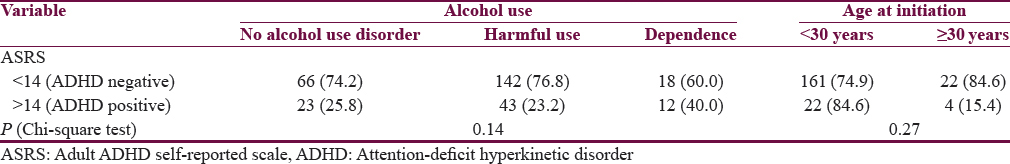
The frequency of ADHD was 25.1% among those with alcohol initiation before the age of 30 years. On the other hand, only 15.4% of those initiating alcohol after the age of 30 years had ADHD. Again, this was not statistically significant (Chi-square test, P = 0.27).
DISCUSSION
A study done among fishermen in Scotland also found similarly high rates of alcohol use among fishermen (80.6%) compared to 79.3% in our sample. This is very high compared to the national average of 24.8% of Indian men as per the GIASH, India report.[1] However, 9.9% of the fishermen in our study had alcohol dependence. This indicates a greater prevalence of alcohol use (79.3% vs. 39.8%), alcohol use disorder defined as AUDIT >8 (60.9% vs. 10.9%), and a higher proportion of probable dependent users defined as AUDIT >20 (9.9% vs. 2.3%) among fishermen compared to general population of Puducherry.[7]
Using the critical items of ASRS (ASRS ≥ 14), we found that 25.7% of fishermen screened positive for ADHD. The rate of 25.7% on the critical items scale compares well with the 23.6% prevalence among college students of Chandigarh by Jhambh et al.[8] and the 21.8% among Kenyan University students by Atwoli et al.[9] However, the studies done in Chandigarh and Kenya used the full ASRS scale (49.3% prevalence in our study). The study among college students of Chandigarh showed that only 5.48% could be truly diagnosed as ADHD based on symptom presence from childhood. However, we have not done a confirmation of diagnosis in our study using either a DSM IV-based structured interview or enquiry about childhood onset of symptoms. The use of full-scale ASRS may have overestimated the ADHD prevalence in our study, but the critical items’ scale of ASRS has given similar estimates found in other adult population of students. One reason for such an overestimation may be the wide or nonspecific nature of symptoms in the full scale as compared to the more focused or “critical” items in the short form of the scale. The critical items of the scale may be more specific to ADHD.
ADHD has been shown to be a risk factor for the development of alcohol use disorders among adolescents. In our study, we found that alcohol-dependent participants were about twice as likely to have ADHD as compared to patients without alcohol use disorders or those with harmful use. The results were not statistically significant and the 95% CI of the OR included unity.
To summarize the key findings, the prevalence of alcohol dependence and harmful use of alcohol appears to be higher among fishermen as among the general population. Although our study did not find a statistically significant association between ADHD and the presence and degree of alcohol use disorders, we found that patients with alcohol dependence were twice as likely to have ADHD than those with harmful use or without alcohol use disorders. The results approached significance.
The study findings are important and indicate the need for improving the availability of treatment of alcohol use disorders at the primary care level, especially among occupational groups who face high levels of stress and are likely to have higher morbidity.
However, future studies that assess risk factors for alcohol use disorders in larger samples must definitely continue to study the contribution of ADHD toward addiction.
The strengths of this study are that, being a community-based study, it is free from self-selection bias and hospital bias that happens in selection of patients in hospital-based studies.
The study has the following limitations: (1) ADHD was assessed cross-sectionally in an adult population using a single measure and false positivity is a concern, especially in view of lack of a confirmatory test. (2) Self-reported questionnaires were used and a reporting bias cannot be ruled out. (3) We do not have information on other risk factors such as family history of alcohol use disorders or ADHD. We have not assessed comorbid substance use, medical diseases, or psychiatric illnesses in this study.
CONCLUSION
In an occupational group of fishermen, the prevalence of alcohol dependence is higher than that in the general population. Fishermen with alcohol dependence are twice as likely to have ADHD as those without alcohol dependence.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 2014. Global Information System on Alcohol and Health. Available from: http://www.who.int/substance_abuse/publications/global_alcohol_report/profiles/ind.pdf?ua=1
- Substance use disorders in adolescents with attention deficit hyperactivity disorder: A 4-year follow-up study. Addiction. 2013;108:1503-11.
- [Google Scholar]
- Evaluation of the persistence, remission, and emergence of attention-deficit/hyperactivity disorder in young adulthood. JAMA Psychiatry. 2016;73:713-20.
- [Google Scholar]
- The association between attention-deficit/hyperactivity disorder and early-onset alcohol dependence: A retrospective study. Indian J Psychiatry. 2008;50:262-5.
- [Google Scholar]
- The Alcohol Use Disorders Identification Test Guidelines for Use in Primary Care (2nd ed). Geneva: WHO; 2001.
- American Psychological Association. Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR Fourth Edition Text Revision. Washington D.C: American Psychiatric Association; 2000.
- Alcohol use and alcohol use disorder among male outpatients in a primary care setting in rural Puducherry. Ind Psychiatry J. 2015;24:135-9.
- [Google Scholar]
- Cross-sectional study of self-reported ADHD symptoms and psychological comorbidity among college students in Chandigarh, India. Ind Psychiatry J. 2014;23:111-6.
- [Google Scholar]
- Self-reported attention deficit and hyperactivity disorder symptoms among university students in Eldoret, Kenya. East Afr Med J. 2010;87:187-91.
- [Google Scholar]






