Translate this page into:
Assessment of Utilization of Rehabilitation Services among Stroke Survivors
Address for correspondence: Dr. Manju Dhandapani, National Institute of Nursing Education, PGIMER, Chandigarh, India. E-mail: manjuseban@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Rehabilitation is probably one of the most important phases of recovery for many stroke survivors. The current study was conducted with the objective to assess the utilization of rehabilitation services and factors affecting nonutilization of rehabilitation services among the stroke survivors.
Materials and Methods:
The current study was carried out in the Neuro Outpatient Department of a tertiary care hospital in India. It was a descriptive study. Consecutive 55 stroke survivors who had met the inclusion and exclusion criteria were recruited in this study. Self-structured rehabilitation tool was used to collect the data.
Results:
Data were analyzed using the descriptive and inferential statistics. Majority of the patients comprised 70.9% of males and 29.1% of females. Among participants, 70.90% were aware about rehabilitation, 67% were utilizing rehabilitation services, whereas 33% were not utilizing rehabilitation services. In the current study, certain reasons were found behind not utilizing rehabilitation services. There were 83.3% of participants who had lack of awareness about rehabilitation services and 61.1% of participants who had no availability of rehabilitation services. Only 45.5% of rural inhabitants were utilizing rehabilitation services as compared to 81.2% of urban inhabitants and 83.23% of suburban inhabitants.
Conclusion:
Rehabilitation is of utmost importance. Hemiparesis, difficulty in performing activity of daily living, difficulty in performing social activities, and difficulty in reasoning were the most common problems faced by people suffering stroke after discharge from the hospital. There was lack of awareness and utilization of rehabilitation services by patients among Indian stroke population. Hence, health workers have an immense role in educating, motivating, and ensuring that rehabilitation services in rural inhabitants.
Keywords
Reasons for not utilizing rehabilitation services
stroke survivors
utilization of rehabilitation services
INTRODUCTION
Stroke is a functional abnormality of the central nervous system that occurs when the normal blood supply to the brain is disrupted. Of all the chronic diseases, stroke has the greatest destabilizing impact. The functional as well as psychological changes related to stroke affects not only the patient, but also the family. The psychological changes include emotional, behavioral, and cognitive after stroke. Rehabilitation is essential following a stroke, and it is important to start early. Rehabilitation cannot undo the damage done to the brain by the stroke, but it can help stroke patients to live better every day. After hospitalization for stroke, many patients still have problem with physical and mental functions. Rehabilitation for these problems can be provided in variety of setting, e.g., physiotherapy, yoga and meditation, occupational therapy, speech therapy, and counseling. Rehabilitation programs are critical in helping patients to regain lost skills, relearn task, and work independently again. Stroke rehabilitation typically starts while at hospital, ideally within a day or two after the stroke. Since recovery occurs most rapidly in the 1st year after the injury, it is critical to concentrate rehabilitative efforts during that time. Early rehabilitation takes advantage of the rapid improvement expected after the event to maximize gains although rehabilitation at any time after stroke is beneficial.[1]
In India, the rehabilitation is mainly centered on physiotherapists. There are 32,800 physiotherapists registered in the Indian Association of Physiotherapists till 2011. There are 3000 occupational therapists and 1700 speech therapists registered in the Rehabilitation Council of India. However, very few centers have organized in hospital and outpatient rehabilitation facilities in the country. Moreover, the use of complementary and alternative medicine treatments by the patients during the poststroke phase hampers the rehabilitation process.[2]
The rehabilitation program must be based on the result of physical, cognitive, communication, psychosocial, functional, and environmental assessments. Functional status is the sum total of all the activities that human performs to survive. Availability of rehabilitation services is important for stroke recovery. In India, stroke care and rehabilitation are only available to a limited number of patients with stroke, mostly in large cities. More than 150 rehabilitation clinics and centers are actively involved in long-term stroke care in India. Stroke awareness and services for stroke among the public and general practitioners are directly proportional to improved care and outcome.[3]
The current study was undertaken with the objective to assess the utilization of rehabilitation services and factors affecting nonutilization of rehabilitation services among the stroke survivors.
Stroke is the leading cause of death and disability in developing countries such as India. Residual disabilities negatively affect the stroke survivor's functional independence and quality of life.[4] Rehabilitation is necessary for them to regain the lost skills, to relearn task, and to be independent again. Hence, need for the study was to identify the factors leading to poor utilization and requiring necessary steps to be taken to enhance the utilization of rehabilitation services.
MATERIALS AND METHODS
The present study was conducted to assess the utilization of rehabilitation services among stroke survivors in the Neuro Outpatient Department (OPD), PGIMER, Chandigarh. Ethical clearance to proceed with the study was obtained from the Institutional Ethical Committee. The research approach was quantitative where data were collected in numerical forms and analyzed using descriptive or inferential statistics. The study constituted all the stroke survivors those reported in the Neuro OPD during the study period. The patients included those who gave consent, had stroke a month back, and were conscious without aphasia. Overall, 55 patients were selected using total enumeration technique. Questionnaire to assess utilization of rehabilitation services included symptoms on assessment, awareness about rehabilitation services, type of rehabilitation services utilized by subjects, and reasons for not utilizing rehabilitation services.
Descriptive and inferential statistics were used to analyze data using Statistical Package for the Social Sciences (SPSS version 16.0).
RESULTS
As shown in Table 1, the mean age of the patients was 52.3 ± 13 (24–80) years. Out of these, 39 (70.9%) were male, 33 (60.0%) were rural inhabitants, and 44 (80.0%) of them were Hindu. Nearly 28 (50.9%) of total participants had education up to secondary standard. About 43 (78.2%) of the participants have per capita income ranging from Rs. 500 to 15,000. Out of 55 participants, 46 (83.6%) were married.

Table 2 depicts clinical health profile of the patients. Among 55 participants, 36 (65.5%) were diagnosed thrombotic cerebrovascular accident (CVA), 8 (14.5%) with subarachnoid hemorrhage, 7 (12.7%) with intracranial hemorrhage, and 4 (7.3%) with thromboembolic CVA. While describing the stroke occurrence, 30 (54.6%) had occurrence of stroke before 1 year, whereas 16 (29.1%) had developed stroke before 6 months. During onset of stroke, 45 (81.8%) participants were at home and 19 (34.5%) were in lying position whereas 18 (32.7%) were in standing position and 28 (51.0%) were working.
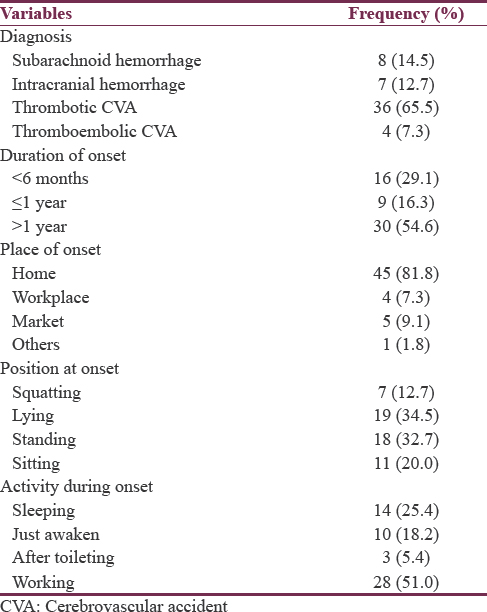
Table 3 elucidates that at the time of assessment, of 55 participants, 35 (63.6%) had hemiparesis, 29 (52.7%) had difficulty in performing activities of daily living, 25 (45.5%) had difficulty in performing social activities, 19 (34.5%) had loss of memory and difficulty in thinking and reasoning, and 16 (29.1%) had dysphasia.
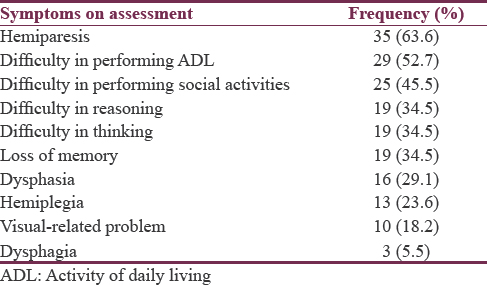
Figure 1 depicts that among 55 participants, 70.9% were aware about rehabilitation services and 29.1% participants were not aware of it.
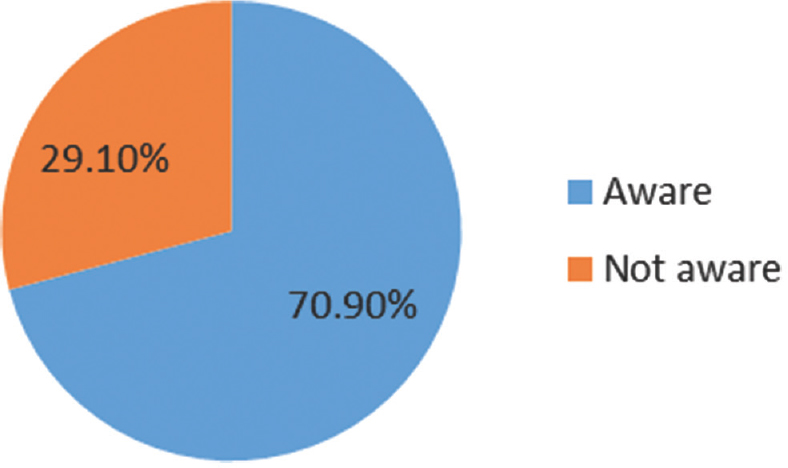
- Awareness of rehabilitation services, n = 55
Figure 2 shows utilization of rehabilitation services and nonutilization of rehabilitation services. Out of 55 participants, 67% were utilizing rehabilitation services, whereas 33% were not utilizing rehabilitation services.
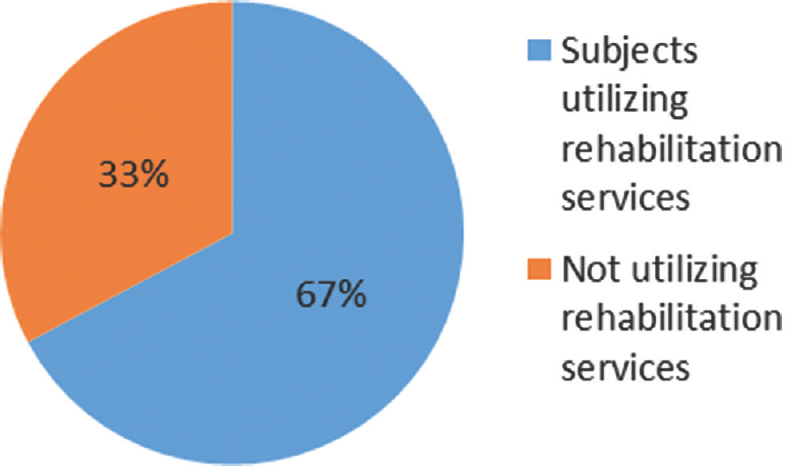
- Utilization of rehabilitation services by subjects, n = 55
Various types of rehabilitation services used by participants assessed are as shown in Figure 3. Overall, 60% among all participants were utilizing physiotherapy, 25.4% were doing yoga/meditation, 5.5% were utilizing occupational therapy, 7.3% were consulting counselor, whereas 1.8% were consulting speech therapist.
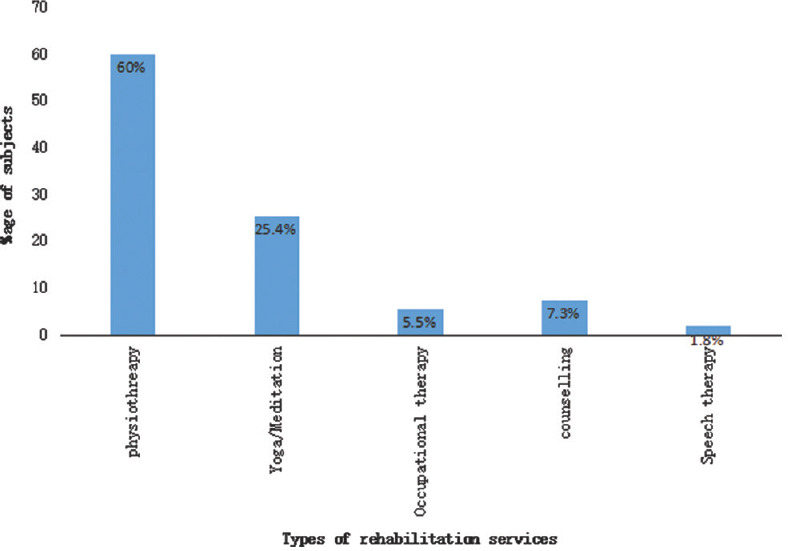
- Types of rehabilitation services utilized by subjects, n = 55
Table 4 elucidates reasons related to nonutilization of rehabilitation services. Out of 18 participants, 15 (83.3%) had lack of awareness about rehabilitation services, 11 (61.1%) had nonavailability of rehabilitation services, 6 (33.4%) had nonavailability of trained health professionals, and 3 (16.6%) had problem in consulting appointment and waiting time, and other reasons responsible for nonutilization of rehabilitation services were lack of family support, lack of transportation, lack of regular source of care, time limitations, financial problems, and superstition.
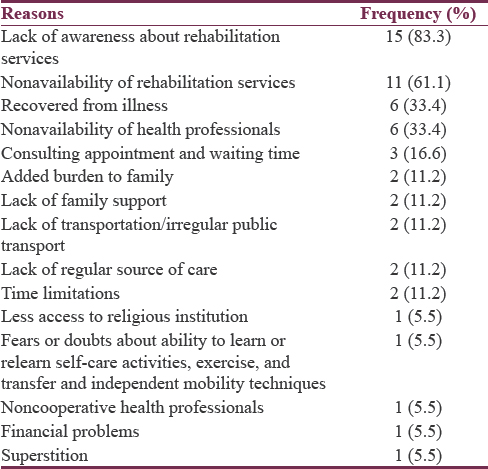
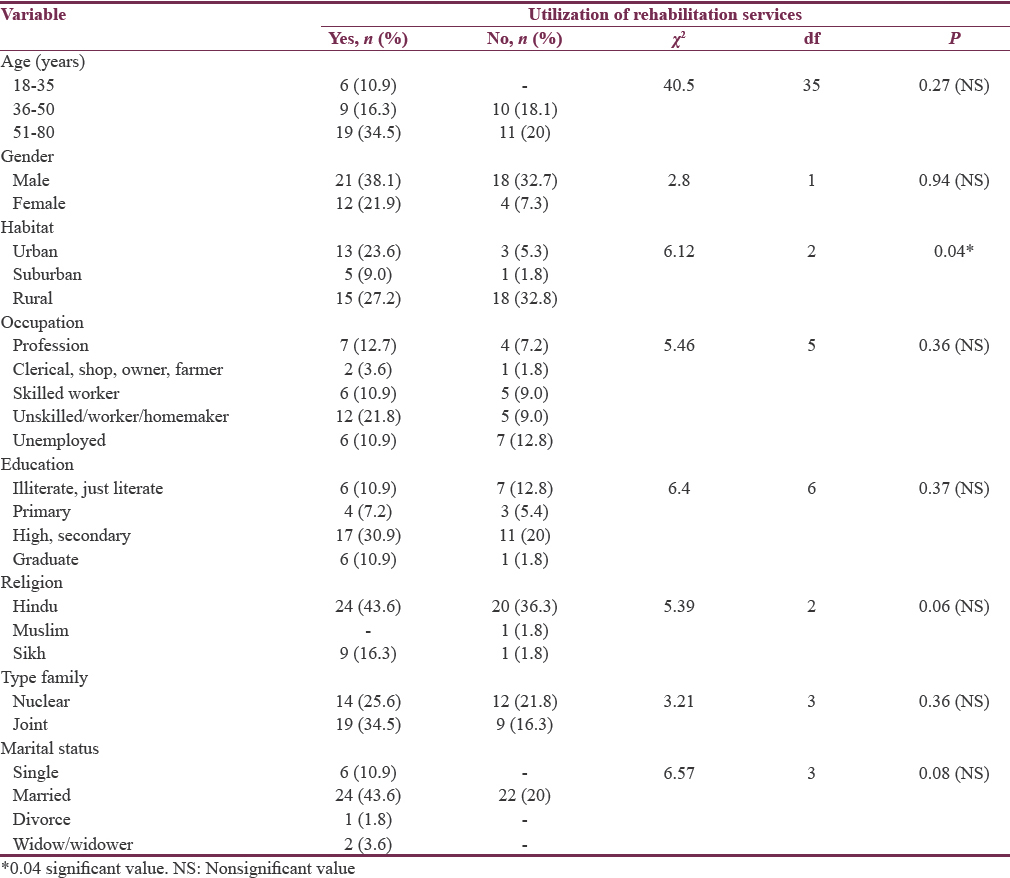
Table 5 depicts the association between sociodemographic profiles of the participants with utilization of rehabilitation services. It was found that condition of habitat was significantly associated with utilization of rehabilitation services (P = 0.04). Among 33 rural inhabitants, only 15 (45.5%) were utilizing rehabilitation services as compared to 81.2% of urban inhabitants and 83.4% of suburban inhabitants.
DISCUSSION
The social burden of various types of stroke is enormous, especially in developing countries.[567] The present study shows similar result as previous studies. Most of the patients were male and aged <45 years. Even in developed countries with advanced health care systems, 60% of the people who suffer stroke either die, become permanently disabled, or become dependent functionally.[5]
There are two major classes of functional impairment that can occur following stroke –hemiparesis in the upper limb and difficulty with independent walking.[6]
Stroke rehabilitation is an active process beginning during acute hospitalization, progressing for those with residual impairments to a systematic program of rehabilitation services, and continuing after the individual returns to the community.
Stroke rehabilitation can help stroke survivors to achieve functional independence and quality of life.[8] A study, conducted by Woodbury et al. Recommended that timely accesses to appropriate rehabilitation services for stroke survivors are needed to optimize recovery and reduce the long-term burden of stroke for patients, families, communities, and the economy. The key to minimize disability following stroke is rehabilitation to retrain patient to improve capacity. It should also be reinforcing that prescribed physical activity training, both aerobic and strength training, is essential to the rehabilitation process.[9]
In the current study, utilization of rehabilitation services was assessed using questionnaire. It was found that of 55 participants, 70.9% were aware of rehabilitation services whereas 67% were utilizing rehabilitation services. Maximum were utilizing physiotherapy. There was a significant association (P = 0.04) between habitat and utilization of rehabilitation services which showed that urban inhabitants had better utilization of rehabilitation services than rural. The reasons for not utilizing rehabilitation services were lack of awareness about rehabilitation services, nonavailability of rehabilitation services, and others including lack of family support, lack of transportation, consulting appointment, and waiting time or nonavailability of health professionals.
A cohort study assesses the effects of race and poverty differences on the process of inpatient rehabilitation services. There were no racial differences in receipt of inpatient rehabilitation services (Blacks, 76%; Whites, 70%) or in the proportion of patients referred within 3 days of admission (Blacks, 43.5%; Whites, 42.0%). Among patients who experienced delay in initiation of rehabilitation, only low-income Blacks experienced worse functional recovery over 12 months. Low-income Black stroke patients who experience delay in initiation of inpatient rehabilitation have a worse trajectory of functional recovery in the 1st year after stroke. Poverty-associated factors in the postdischarge setting may explain this phenomenon.[10]
There are multiple factors affecting outcome following stroke, such as age, nutritional status, etc.[1112] A study on rehabilitation outcome of elderly after a stroke showed that impaired cognition status at admission negatively affects the rehabilitation outcome of elderly stroke patient.[11]
Cognitive behavioral and functional impairment adds more burden on patient and caregivers.[131415] Nurses need to guide, motivate, and counsel patient and caregivers to utilize rehabilitation services in indoor departments as well as at outdoor departments.
Health action is influenced by an individual's state of readiness, beliefs shaped by personal, social and situational sources, as well as cues to action. Innovative technological advances in treatment also may bring down impairments.[16] Programs of health education should aim to minimize barriers to health services and provide cues to action. Large proportions of people may be in a state of readiness but lack the information or the cues required to take appropriate action. Public awareness programs need to take into account levels of health knowledge to provide the information and cues that are necessary to influence behavior.
It is an organized effort to help stroke patients maximize all opportunities for returning to an active and productive lifestyle. Because the clinical manifestations of stroke are multifaceted and complex, stroke rehabilitation is best implemented through the coordinated efforts of a team of rehabilitation professionals.
Hence, public awareness and education campaigns should be initiated by the nurses that targeted who are at risk of stroke and educate about treatment and important of follow-ups, rehabilitation services in accordance with their lower level of education, in a language that is easily understandable.
CONCLUSION
It has been concluded in this study that those participants who were utilizing rehabilitation services, i.e., physiotherapy, occupational therapy, yoga/meditation, speech therapy, and consulting counselor regularly, had better outcome in health status as compared to those who were not utilizing it. Most of the participants who were not utilizing rehabilitation services were rural inhabitant, and the factors responsible for not utilizing rehabilitation services were lack of awareness and nonavailability of rehabilitation services. Hemiparesis, difficulty in performing activity of daily living, difficulty in performing social activities, and difficulty in reasoning were the common problems faced by people suffering stroke after discharge from the hospital. There was lack of awareness and utilization of rehabilitation services by patients among Indian stroke population. Hence, health workers have an immense role in educating, motivating, and ensuring that rehabilitation services in rural inhabitants.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Complementary and alternative medicine treatments among stroke patients in India. Top Stroke Rehabil. 2012;19:384-94.
- [Google Scholar]
- Population-based stroke survey in Mumbai, India: Incidence and 28-day case fatality. Neuroepidemiology. 2008;31:254-61.
- [Google Scholar]
- Serum lipid profile spectrum and delayed cerebral ischemia following subarachnoid hemorrhage: Is there a relation? Surg Neurol Int. 2015;6:S543-8.
- [Google Scholar]
- Psychological problems after stroke and their management: State of knowledge. 2012. Neurosci Med. 3:83-9. Available from: http://www.ncbi.nml.nih
- [Google Scholar]
- Functional Impairment Following Stroke: Implication for Rehabilitation. Toronto Rehabilitation Institute. Available from: http://www.ncbi.nml.nih.gov
- [Google Scholar]
- Comparative evaluation of H&H and WFNS grading scales with modified H&H (sans systemic disease): A study on 1000 patients with subarachnoid hemorrhage. Neurosurgical Review. 2018;41:241-7.
- [Google Scholar]
- Recommendations for the establishment of stroke systems of care: Recommendations from the American Stroke Association's Task Force on the Development of Stroke Systems. Stroke. 2005;36:690-703.
- [Google Scholar]
- Community Based Rehabilitation for Stroke Survivors. Canadian Stroke Network, Toronto Rehabilitation Institute. Available from: http://www.ncbi.nlm.gob/pubmed
- [Google Scholar]
- Effect of Race and Poverty on the Process and Outcome of Inpatient Rehabilitation Services among Stroke Patients. Available from: http://www.ncbi.nlm.gob/pubmed
- [Google Scholar]
- Rehabilitation outcome of elderly patients after a first stroke: Effect of cognitive status at admission on the functional outcome. Arch Phys Med Rehabil. 2002;83:742-9.
- [Google Scholar]
- Serum albumin level in spontaneous subarachnoid haemorrhage: More than a mere nutritional marker! British Journal of Neurosurgery. 2018;32:47-52.
- [Google Scholar]
- Study of factors determining caregiver burden among primary caregivers of patients with intracranial tumors. Surg Neurol Int. 2015;6:160.
- [Google Scholar]
- Prevalence and Trends in the Neuropsychological Burden of Patients having Intracranial Tumors with Respect to Neurosurgical Intervention. Annals of Neurosciences. 2017;24:105-10.
- [Google Scholar]
- Trends in cognitive dysfunction following surgery for intracranial tumors. Surg Neurol Int. 2016;7:S190.
- [Google Scholar]
- Median Supraorbital Keyhole Approach for Clipping Ruptured Distal Anterior Cerebral Artery Aneurysm: Technical Report with Review of Literature. World neurosurgery. 2018;112:73-6.
- [Google Scholar]






