Translate this page into:
Assessment of Sleep Quality among Medical Doctors in a Tertiary Hospital in a Semi-Rural Setting
Address for correspondence: Dr. Ibrahim Aliyu, Department of Paediatrics, Aminu Kano Teaching Hospital, Kano, Nigeria. E-mail: ibrahimaliyu2006@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Sleep is an integral part of human physiology; therefore, disorders of sleep may result in significant derangement in human functionality. Sleep medicine has received little attention in Nigeria. Against this backdrop, this survey seeks to evaluate the quality of sleep among doctors.
Methodology:
This was a cross-sectional descriptive study involving 59 doctors working with Federal Medical Centre Birnin Kebbi, Kebbi State, Nigeria; it was done between August 2017 and December 2017. Purposive sampling method was adopted. The Pittsburgh Sleep Quality Index (PSQI) and the Epworth Sleepiness Scale (ESS) were adopted. The questionnaire was self-administered.
Results:
There were 34 (57.6%) males and 25 (42.4%) females. Their age ranged from 20 to 66 years, with a mean of 34.39 ± 8.00. The Epworth score ranged from 8 to 29, with a mean of 16.1 ± 4.4, while the PSQI score ranged from 5 to 19, with a mean of 9.5 ± 2.7. The mean work hour per week was 90.3 ± 36.2 h, and majority of the respondents worked for >80 h and or >24 h consecutively in the preceding week, and most had high ESS scores; however, this observation was not statistically significant (Fisher's exact test = 4.0904, P = 0.213). All respondents were poor sleepers and majority sleep for <7 h in the night. Respondents had worked for 5 years and less; house officers and medical offers had more tendencies for daytime sleepiness.
Conclusion:
All respondents were poor sleepers and also had prolonged work hours per week; there was also heightened daytime sleepiness.
Keywords
Doctors
Nigeria
sleep quality
work hours
INTRODUCTION
Sleep is an integral part of human physiology; it could be refreshing and healing. Therefore, disorders of sleep may result in significant derangement in human functionality. Therefore, the need for getting sufficient sleep cannot be overemphasized. Lack of sufficient sleep has been associated with significant weight gain, cardiovascular diseases such as hypertension, neurologic disorders such as Alzheimer's disease, and stroke. Quite recently, a Chinese doctor in 2018 collapsed and died after an 18-h nonstop shift duty without sleep though this was attributed to a subarachnoid hemorrhage from a ruptured cerebral aneurysm; whether lack of sleep had a significant role in her death remains unclear.[1] Lack of sleep also depresses the immune system and also results in loss of memory; this will be particularly alarming for health workers whose primary responsibility is to care for the sick; their job is delicate and gives no room for error, especially in times of decision-making, drug calculation, and administration.
The National Sleep Foundation in the United States of America states that sleep duration vary with age; in the first 3 months of life it is between 14 and 17 h; between 4 and 11 months is 12–15 h; among toddlers it is 11–14 h; in preschoolers and schoolers it is between 10 and 13 h; in teenagers it is 8–10 h while adults should sleep for between 7 and 9 h.[2] However, the mean sleep duration has been shown to vary in different countries; Sweileh et al.,[3] in Nablus, Palestine, reported a mean sleep duration of 6.4 ± 1.1 h in 400 subjects studied in 2009.
Poor sleep quality had been reported among health professionals, Nazatul et al.,[4] Chien et al.,[5] and Aliyu et al.[6] reported poor sleep quality among Malaysian, Chinese, and Nigerian nurses; similar observations were reported by Surani et al.[7] and Vela-Bueno et al.[8] among physicians. Sleep disorder may result in excessive daytime sleepiness, impaired judgment, and poor neurocognitive and psychomotor performance; these may result in error of clinical decision-making detrimental to patient health.[6]
Sleep medicine has received little attention in Nigeria. There is obviously dearth of local information on sleep disorders, especially among health workers.[69] Against this backdrop, this study sought to determine the quality of sleep among doctors and to determine the relationship between duration work hours and the sleep scores among doctors in our hospital.
METHODOLOGY
Federal Medical Centre (FMC) Birnin Kebbi is located in Birnin Kebbi which is the capital of Kebbi State, located in North West Nigeria; it is a 300-bedded hospital and the only tertiary hospital in the state with an estimated population of over 3 million people. The hospital has well-established clinical and laboratory departments ran by doctors, nurses, and laboratory scientists. Just like most hospitals in Nigeria, doctors do their routine daily duties which start from 8.00 am to 4.00 pm on weekdays, while call duty starts from 4.00 pm to 8.00 am the next days. On weekends, we run 24 h call. Call duties are undertaken by teams which consist of house officers, medical officers, and consultants.
This study was cross-sectional descriptive involving 59 doctors working with FMC Birnin Kebbi, Kebbi State, Nigeria; it was conducted between August 2017 and December 2017. Purposive sampling method was adopted. Using a poor quality sleep prevalence of 52% among doctors reported by Kolo et al.,[9] a sample size of 383 was calculated, and for a population <10,000 (N/1 + N/n), the sample size of 59 was calculated based on a targeted population of 70 doctors. All doctors working at FMC Birnin Kebbi were included in this study; however, participants who were on annual/study leave at the time of this study, those with known history of chronic illnesses such as diabetes mellitus and asthma, those on beverages such as caffeine that could affect sleep parameters, and those who declined consent were excluded from the study. The Pittsburgh Sleep Quality Index (PSQI)[10] which has been validated in Nigeria by Oshinaike et al.[11] was adopted in this study; a PSQI total score >5 was diagnostic of poor sleep quality, and the Epworth Sleepiness Scale (ESS)[12] was also adopted: A score of 0–7 was considered normal, 8–9 was average tendency of daytime sleepiness, 10–15 was signified presence of excessive daytime sleepiness, and 16–24 was daytime sleepiness requiring medical intervention.[13] These scales were pretested among 10 selected volunteer doctors to ensure that the contents were understood and internal consistency was maintained with a Cronbach's alpha score of 0.80. The questionnaire was self-administered and other relevant information such as age, sex, years of working experience, and rank were obtained from the respondents. Work hour of doctors was broadly classified into two groups based on the recommendation of the United States of America Accreditation Council for Graduate Medical Education,[13] namely, >80 h of work in a week and or >24 consecutive hours of work and those with <80 h of work in a week.[14] Respondents were assured of anonymity and confidentiality, and the returned questionnaires were sealed in an develop before delivery to the researchers, which should minimize social desirability bias.
Ethical approval was obtained from the Research Ethics Committee of FMC Birnin Kebbi. Informed consent was also obtained from the participants.
Data analysis
Obtained data were entered into the Statistical Package for the Social Sciences version 20 (IBM Inc., Armonk, New York; United States of America). The staffs’ rank and years of working experience and physician work hours were summarized using frequency tables. Chi-square or Fisher's exact tests were deployed where appropriate to test for relationship among categorical variables, and P < 0.05 was set as statistically significant.
RESULTS
There were 34 (57.6%) males and 25 (42.4%) females. Their age ranged from 20 to 66 years, with a mean of 34.39 ± 8.00; the sleep latency ranged from 1.00 to 120.00 min, with a mean of 18.22 ± 4.00 min; hours of night sleep ranged from 1.00 to 9.00 h, with a mean of 6.31 ± 1.60 h.
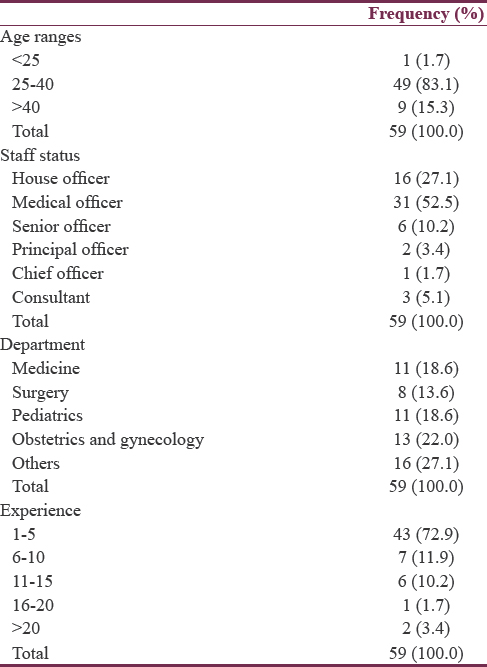
Most respondents were of the 20–40 years’ age group; furthermore, medical officers and doctors in the obstetrics and gynecology (O and G) department were mostly represented, and most respondents had worked for between 1 and 5 years [Table 1]. Years of working experience ranged from 1 to 25 years, with a mean of 5.4 ± 2.3 years.
The Epworth score ranged from 8 to 29, with a mean of 16.1 ± 4.4; the PSQI score ranged from 5 to 19, with a mean of 9.5 ± 2.7. The Epworth score for males ranged from 8.0 to 28.0, with a mean of 15.0 ± 4.0, while the PSQI score ranged from 5.0 to 19.0, with a mean of 9.0 ± 3.0; however, the Epworth score for females ranged from 10.0 to 29.0, with a mean of 17.5 ± 4.7, while the PSQI score ranged from 5.0 to 14.0, with a mean of 10.1 ± 2.2.
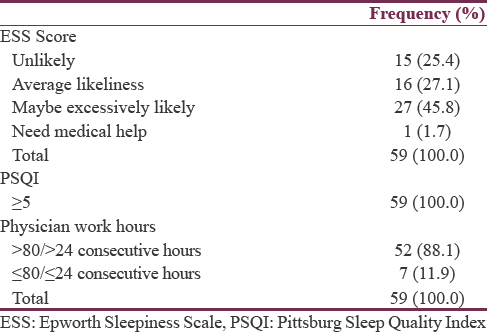
Work hours per week ranged from 23.0 to 216.0 h, with a mean of 90.3 ± 36. 2 h. Most respondents had ESS score in the “maybe excessively likely scale” while all were poor sleepers; however, majority of them worked for >80 h and or >24 h consecutively in the preceding week [Table 2].
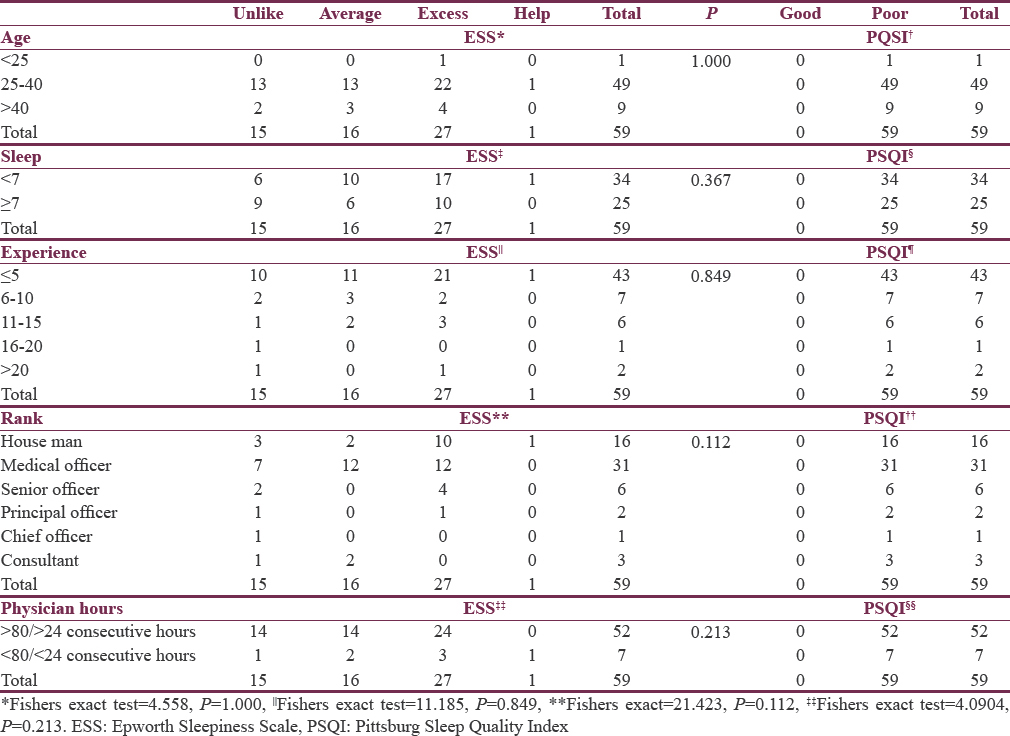
Most respondents in the 20–40 years’ age group had excessive likelihood for dozing and the only recorded respondent in the need medical help category was also of the 20–40 years’ age group; however, this observation was not statistically significant (Fisher's exact test = 4.558, P = 1.000). Furthermore, respondents who sleep for <7 h had greater tendencies for daytime dozing, but this observation was not statistically significant (Fisher's exact test = 3.007, P = 0.367). The years of working experience and the respondents rank had no statistically significant relationship with ESS score (Fisher's exact test = 11.185, P = 0.849; Fisher's exact test = 21.423, P = 0.112); however, those had worked for 5 years and less; house officers and medical offers had more tendencies for daytime sleepiness. Although majority of the respondents worked for >80 h in a week and or >24 h consecutively in the preceding week, most had high ESS scores; however, this observation was not statistically significant (Fisher's exact test = 4.0904, P = 0.213). Irrespective of their subgroups, all respondents were poor sleepers [Table 3].
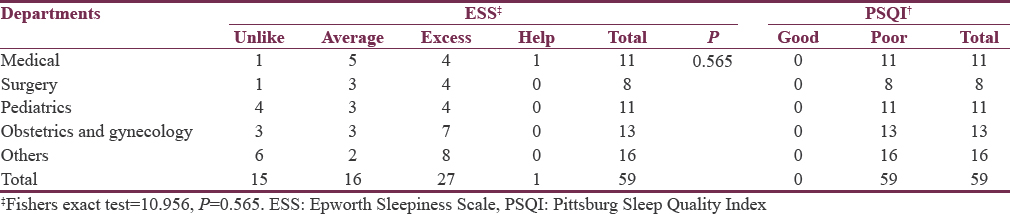
Majority of the respondents had either average tendencies or excessive tendency to dozing, and a single respondent needed help for daytime sleepiness though this observation was not statistically significant (Fisher's exact test = 10.956, P = 0.565). All respondents in this study were poor sleepers irrespective of their departments [Table 4].
DISCUSSION
The effect of sleep loss is cumulative; significant buildup may result in complications ranging from mood swings to cognitive malfunction and errors of judgment.[15] This study explored the sleep quality of medical doctors in a tertiary center in a semi-urban setting. The age range of the respondents was between 20 and 66 years, with a mean of 34 ± 8 years; this observation was similar to that of Kolo et al.[9]
Unfortunately, all respondents in this study were poor sleepers; this observation is higher than the 85% reported by Zamanian et al.,[16] 43.1% reported by Ghalichi et al.,[17] 54.2% reported by Aliyu et al.,[6] and 61% reported by Kolo et al., respectively;[9] the fewer staff strength in our institution mean that doctors arelikely to have frequent call duties, and in a setting of high patient load, they are likely to be overburdened resulting in more sleep loss and deprivation.
The tendency to doze during daytime was mostly experienced among the younger doctors; understandably, the younger doctors are the house officers and young residents/medical officers who are first and second on calls; therefore, they sleep in the hospital; hence, they have a greater tendency of being sleep deprived. This observation differed from that of Menon et al.[18] who reported more daytime sleepiness among older nurses who ran shift duties. This finding is of great concern because poor sleep has been associated with risk of physical injury; Comondore et al.[19] reported that a resident physician who is sleep deprived is at risk of motor vehicle collision; sleep deprivation is among the leading cause of motor accidents due to falling asleep while driving in the United States of America,[20] and this has been linked to prolonged work hours.[21] Furthermore, the risk of injury from needle sticks or lacerations is heightened in sleep-deprived physicians,[22] and the risk of prescription error is also heightened; a case in point is the 1989 death of Libby Zion which was partly attributed to sleep deprivation of young medical doctors who were poorly supervised.[23] This is a common scenario in many developing countries with limited manpower – this means many deaths in our setting if properly audited might be quite revealing; this resulted in “the 405.5 rule” restricting working hours for doctors to 24 consecutive h or 80 h per week.[24] Most respondents in our study worked for >80 h in a week; therefore, regulation of doctors’ work hour should be strictly enforced. To mitigate this, more doctors need to be employed and the shift system, especially in the emergency unit, should be practiced.
Limitations
We noted some limitations in this study; this study was single center based with relatively small sample size that notwithstanding, our observation may be applicable to most health facilities in rural setting who have similar staff strength – with more staffs in the urban hospitals and less staffing in rural hospital – therefore resulting in frequent call duties. Furthermore, the sampling method adopted is another limitation identified. Although the ESS and PSQI scores were based on the subject's self-reportage, therefore bias may not be completely ruled out; however, respondents were assured of anonymity and confidentiality, and the returned questionnaires were sealed before delivery to the researchers. The objective measurement of sleepiness remains measuring sleep latency by multiple sleep latency test (MSLT).[25] However, several investigators have established correlations between ESS- and MSLT-defined sleepiness.[2627]
CONCLUSION
This study showed that the respondents were poor sleepers; furthermore, most had >80 working hours in a week. Hence, we recommend that there should be a strict regulation of working hours for doctors, especially house and medical officers; this will require employing more doctors in this cadre to ensure efficient rotation of doctors; furthermore, supervising physicians should monitor the sleep hygiene practices of junior doctors under their watch, so that anomalies are detected early and remedies instituted.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Chinese Doctor Dies from Stroke after Working 18 Hours: Reports. Available from: https://www.channelnewsasia.com/news/asiapacific/chinese-doctor-dies-from-stroke-after-working-18-hours-reports-9827212
- National Sleep Foundation Recommends New Sleep Times. Available from: https://www.sleepfoundation.org/press-release/national-sleep-foundation-recommends-new-sleep-times/page/0/1
- Sleep habits and sleep problems among Palestinian students. Child Adolesc Psychiatry Ment Health. 2011;5:25.
- [Google Scholar]
- Prevalence of sleep disturbance among nurses in a Malaysian government hospital and its association with work characteristics. JUMMEC. 2008;11:66-71.
- [Google Scholar]
- Sleep quality among nurses in a tertiary hospital in North-West Nigeria. Niger Postgrad Med J. 2017;24:168-73.
- [Google Scholar]
- To assess sleep quality among Pakistani junior physicians (House officers): A cross-sectional study. Ann Med Health Sci Res. 2015;5:329-33.
- [Google Scholar]
- Insomnia and sleep quality among primary care physicians with low and high burnout levels. J Psychosom Res. 2008;64:435-42.
- [Google Scholar]
- Sleep health of healthcare workers in Kano, Nigeria. Niger J Clin Pract. 2017;20:479-83.
- [Google Scholar]
- The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213.
- [Google Scholar]
- Quality of sleep in an HIV population on antiretroviral therapy at an urban tertiary centre in Lagos, Nigeria. Neurol Res Int 2014 2014:298703.
- [Google Scholar]
- A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540-5.
- [Google Scholar]
- Accreditation Council for Graduate Medical Education. Common Program Requirements. 2004. Available from: http://www.acgme.org/acwebsite/dutyhours/dh_dutyhourscommonpr.pdf
- [Google Scholar]
- Cumulative effects of sleep restriction on daytime sleepiness. Psychophysiology. 1981;18:107-13.
- [Google Scholar]
- Influence of sleep on quality of life among hospital nurses. Electron Physician. 2016;8:1811-6.
- [Google Scholar]
- Sleep quality and health complaints among nursing students. Ann Indian Acad Neurol. 2015;18:363-4.
- [Google Scholar]
- The impact of sleep deprivation in resident physicians on physician and patient safety: Is it time for a wake-up call? BCMJ. 2008;50:560-4.
- [Google Scholar]
- Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352:125-34.
- [Google Scholar]
- Emergency medicine resident related auto accidents-is sleep deprivation a risk factor? Acad Emerg Med. 2000;7:1171.
- [Google Scholar]
- Effects of work hour reduction on residents’ lives: A systematic review. JAMA. 2005;294:1088-100.
- [Google Scholar]
- The Libby Zion case. One step forward or two steps backward? N Engl J Med. 1988;318:771-5.
- [Google Scholar]
- Sleep loss in resident physicians: The cause of medical errors? Front Neurol. 2010;1:128.
- [Google Scholar]
- Application of the multiple sleep latency test in disorders of excessive sleepiness. Electroencephalogr Clin Neurophysiol. 1982;53:443-52.
- [Google Scholar]
- The Epworth Sleepiness Scale may not reflect objective measures of sleepiness or sleep apnea. Neurology. 1999;52:125-31.
- [Google Scholar]
- Correlating subjective and objective sleepiness: Revisiting the association using survival analysis. Sleep. 2011;34:1707-14.
- [Google Scholar]






