Translate this page into:
Assessment of Depression, Anxiety, and Sleep Disturbance in COVID-19 Patients at Tertiary Care Center of North India
Ramakant Yadav, DM Department of Neurology, UP University of Medical Sciences, Saifai Etawah, 206130, Uttar Pradesh India rkyadav_2003@yahoo.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background and Objective The novel Coronavirus pandemic surfaced in Wuhan, China in December 2019 and spread rapidly across the globe. In recent available literature, most of the studies were done to estimate the burden of psychiatric problems among general population due to this pandemic, Therefore, this study was planned to assess depression, anxiety, and sleep disturbance among Coronavirus disease-2019 (COVID-19) patients.
Materials and Methods A hospital-based, cross-sectional study was done from June 2020 to August 2020 among 100 COVID-19 patients who were admitted and fulfilled the inclusion criteria. Assessment of depression, anxiety, and sleep disturbance were done by patient health questionnaire-9 (PHQ-9) scale, generalized anxiety disorder-7 (GAD-7) scale and Pittsburg sleep quality index (PSQI), respectively.
Results In this study, 73% were males and 27% were females. The mean age of the patients in present study was 42.90 ± 16.33 years. This study reveals that depression was in 27%, anxiety in 67%, and sleep disturbance in 62% of patients. Depression and anxiety were found significantly associated with presence of comorbidity and severity of illness (p < 0 0.05). The association of sleep disturbance with severity of illness was also found statistically significant (p < 0.05).
Conclusion The risk of psychological stress is high in COVID-19 patients. The psychological problems among COVID-19 patients are commonly related to the consequences of disease, and severity and contagiousness of the disease. Therefore, in this present pandemic situation, it is more important to identify these psychological problems among COVID-19 patients, so that better care and timely interventions can be done with respect to psychological issues.
Keywords
COVID-19
depression
anxiety
sleep disturbance
Introduction
Central nervous system (CNS) is infected by variety of viruses, and it can be manifested as neuropsychiatric syndromes of cognitive and behavioral impairment.1 2 3 Coronaviruses are single-stranded RNA viruses, and there are many strains of Coronavirus which have been affected humans and manifested as mild upper respiratory tract infections in healthy individuals.4 5 These Coronaviruses also have been found in the cerebrospinal fluid (CSF) of the patients who presented with seizures, encephalitis, and encephalomyelitis.6
The severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS) outbreaks were caused by novel strains of Coronavirus in 2002 and 2012, respectively.5 The novel Coronavirus pandemic, which broke out in Wuhan, China, in December 2019 and spread rapidly across the globe, was caused by severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2). Both SARS-CoV-2 infected patients and general population might be at increased risk of psychological problems due to the consequences of pandemic such as physical isolation and stressful environment.7 8 9
These COVID-19 patients are more vulnerable to develop neuropsychiatric syndromes because of the stigma associated with disease and concern about the outcome of this infection.10 11 In recent studies, it was found that psychological problems affected the general well-being of SARS-CoV-2 infected patients as well as the general public significantly.12
Sleep is very important for good quality of life, and in previous studies, it was found that sleep disturbances was an important risk factor for suicidal tendencies, and sleep abnormalities were also associated with anxiety and depression.13
There are multiple causes of psychiatric manifestation of Coronavirus infection; they might be immunological response toward infection, cerebrovascular disease and level of physiological impairment and psychological effect of this contagious viral illness.14
Psychological problems are gaining attention in this present situation of pandemic, and there is very little information on increase in psychological problems in this present scenario.15
There is already evidence of neuropsychiatric manifestations among COVID-19 patients, so physicians should be alert to evaluate mental disorders in these patients, so that timely intervention can be done. Therefore, this study was planned to assess the anxiety, sleep disturbance, and depression among COVID-19 patients.
Materials and Methods
A hospital-based, cross-sectional study was done from June 2020 to August 2020 among 100 COVID-19 patients who were admitted, and fulfilled the study protocol, in the indoor of a COVID-19 hospital of a tertiary care center in rural Uttar Pradesh, north India. This institution is run by state government, and patients were referred from nearby districts.
These patients were classified into mild, moderate, and severe categories of COVID-19 illness, depending upon severity of symptoms like those patients who had fever, dry cough, myalgia and other nonspecific symptoms were categorized as mild illness, while those patients had above symptoms along with dyspnea on exertion or tachypnoea (respiratory rate [RR] > 24/minute) and saturation of peripheral oxygen (SpO2) 90 to 94% on room air were categorized as moderate illness; patients having any of the above signs and symptoms with SPO2 less than 90% on room air or RR > 30/minutes were categorized into “severe illness” category.
Sample Size
This study was done from June 2020 to August 2020; 100 COVID-19 patients among those admitted and who fulfilled the inclusion criteria were taken for study.
Inclusion and Exclusion Criteria
Age 18 years or more who were admitted with positive reverse transcriptase-polymerase chain reaction (RT-PCR) test for SARS-CoV-2 were included. Those who refused to provide consent to participate in the study, critically ill (SpO2 < 90% with shock or altered sensorium) and requiring ventilatory support for management, hemodynamically unstable, with other known mental health disorders, and/or those who were taking such drugs which can affect the mind, emotions, and behavior, were excluded from the study.
Data were collected from patients according to a predesigned and pretested proforma gathering sociodemographic characteristics, comorbidity, and disease severity. Assessment of depression, anxiety, and sleep disturbance were done by patient health questionnaire-9 (PHQ-9) scale, generalized anxiety disorder-7 (GAD-7), scale and Pittsburg sleep quality Index (PSQI), respectively.
PHQ-9 scale: This scale is a 9-question instrument used for assessment of presence and severity of depression. The range of PHQ-9 score is 0 to 27, as response of each of the 9 question will be scored from 0 (not at all) to 3 (nearly every day). If score is 0 to 4, then there is no depression; if score is 5 to 9, then there is mild depression; if score is 10 to 14, then there is moderate depression; if score is 15 to 19, then there is moderately severe depression; if score is 20 to 27, then there is severe depression.16
GAD-7 scale: The range of GAD-7 score is 0 to 21, as response of each question is scored from 0 (not at all) to 3 (nearly every day). If score is 0 to 5, then there is no anxiety; if score is 6 to 10, then there is mild anxiety; if score is 10 to 15, then there is moderate anxiety; if score is 16 to 21, then it is labeled as severe anxiety.17
Assessment of sleep disturbance was done by PSQI. This index is used to assess sleep quality in the previous month. It has 19 self-rated questions which are divided into seven components: sleep quality, sleep duration, sleep latency, habitual sleep efficiency, sleep disturbance, use of sleeping medicine, and daytime dysfunction. Response to each of the components can be scored from 0 (no difficulty) to 3 (severe difficulty), so the range of total score (global score) of these seven components can be 0 to 21. In this study, score > 7 was taken for determination of sleep disturbance.18
Statistical Analysis
The data were analyzed using SPSS software, version 25 (IBM Corp., Chicago, USA). Chi-square test was used to establish the relationship among different variables, and p < 0.05 was considered statistically significant.
Results and Observations
The mean age of the patients in the study was 42.90 ± 16.33 years, with a range from 18 to 70 years. There were 28% of patients found in the age group of 18 to 29 years, which was the most common age group. Out of 100 patients, there were 73% males and 27% females. Majority of the patients in study were literate (85%) and above the poverty line (93%). There were 24% smokers, 14% alcoholics, and 9% both smokers and alcoholics, and among alcoholics, all were occasionally alcoholic none of them was addicted to alcohol .In this study, we found diabetes in 13%, hypertension in 13%, chronic obstructive pulmonary disease (COPD) in 4%, and asthma in 3% of COVID-19 patients . There were 61% mild cases, 19% moderate cases, and 15% severe cases in the study (Table 1).
|
S. no. |
Variable name |
Subgroups |
Total n = 100(%) |
|---|---|---|---|
|
Abbreviations: APL, above poverty line; BPL, below poverty line; COPD, chronic obstructive pulmonary disease; SD, standard deviation. |
|||
|
1 |
Age (years) |
18–29 |
28 (28.0) |
|
30–39 |
19 (19.0) |
||
|
40–49 |
16 (16.0) |
||
|
50–59 |
18 (18.0) |
||
|
60–69 |
12 (12.0) |
||
|
70–79 |
05 (05.0) |
||
|
≥80 |
02 (02.0) |
||
|
Mean ± SD |
42.90 ± 16.33 |
||
|
2 |
Gender |
Male |
73 (73.0) |
|
Female |
27 (27.0) |
||
|
3 |
Socioeconomic status |
APL |
93 (93.0) |
|
BPL |
07 (7.0) |
||
|
4 |
Behavioral factors |
Smoker |
24 (24.0) |
|
Alcoholic |
14 (14.0) |
||
|
Smoker and alcoholic |
09 (9.0) |
||
|
5 |
Presence of comorbidity |
Diabetes |
13 (13.0) |
|
Hypertension |
13 (13.0) |
||
|
COPD |
04 (4.0) |
||
|
Asthma |
03 (3.0) |
||
|
6 |
Severity of illness |
Mild |
66 (66.0) |
|
Moderate |
19 (19.0) |
||
|
Severe |
15 (15.0) |
||
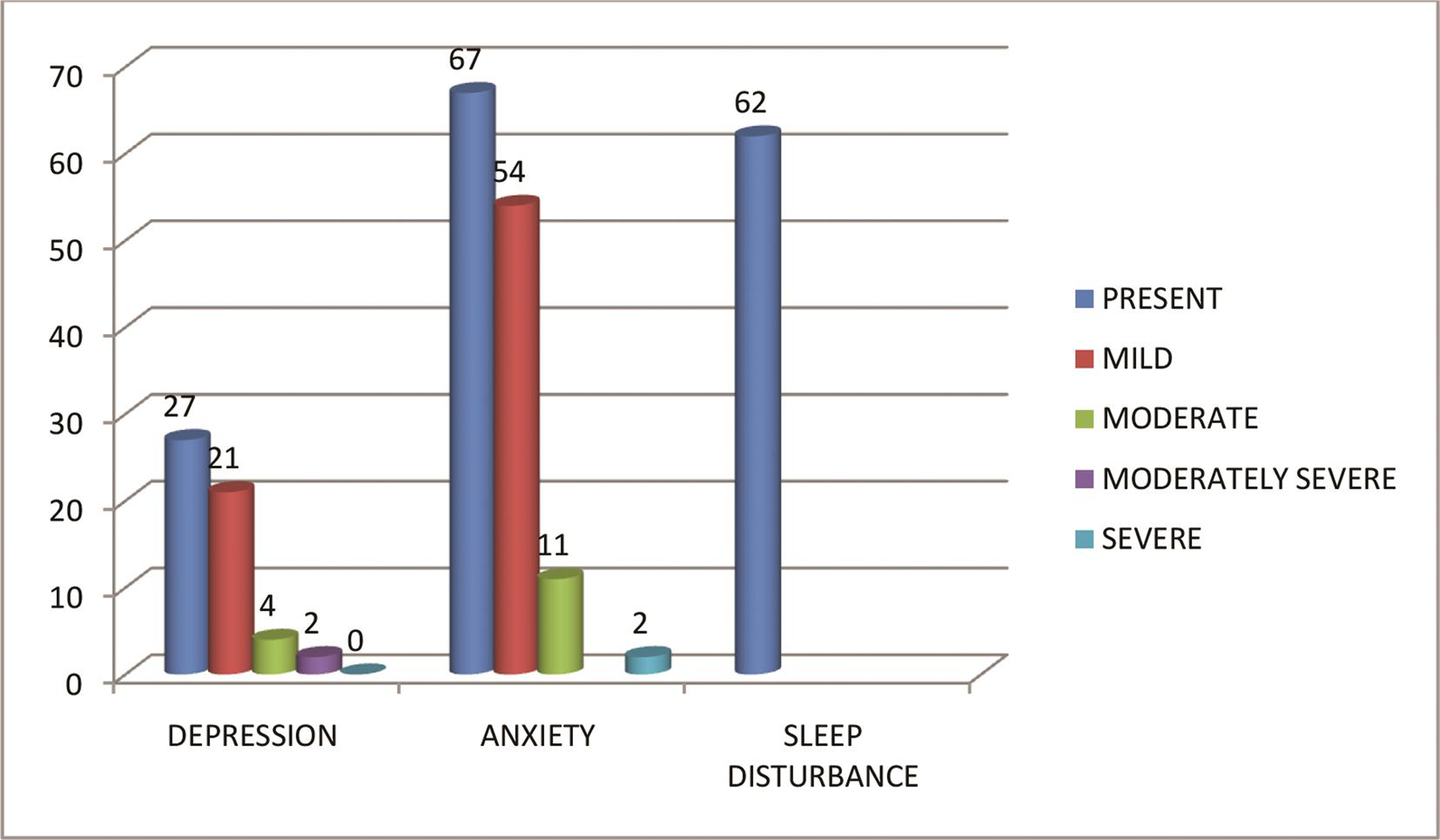
In this study depression was found among 27% COVID-19 patients. Among depression, mild depression 21%, moderate 4%, moderately severe was 2% (Fig. 1) In this study, mean PHQ-9 score was 3.54 ± 2.93, and when PHQ-9 score of depressive patients was compared with their severity of illness, it was found to be statistically significant (p < 0.05).
-
Fig. 1 Distribution of depression, anxiety, and sleep disturbance in COVID-19 patients
Fig. 1 Distribution of depression, anxiety, and sleep disturbance in COVID-19 patients
Table 2 depicts the various associations of depression with age group, gender, socioeconomic status, behavioral factors, presence of comorbidity, and severity of illness. We found the association to be statistically significant in age group, comorbidity, and severity of illness (p < 0.05), while it was not statistically significant with regard to gender, behavioral factors, and socioeconomic status.
|
S. no. |
Variable name |
Subgroups |
Depression (%) |
Chi-square (p-value) |
|---|---|---|---|---|
|
Abbreviations: APL, above poverty line; BPL, below poverty line; COPD, chronic obstructive pulmonary disease. aStatistically significant. |
||||
|
1 |
Age (years) |
18–29 |
04 (14.3) |
15.19 (p < 0.05)a |
|
30–39 |
05 (26.3) |
|||
|
40–49 |
03 (18.8) |
|||
|
50–59 |
09 (50.0) |
|||
|
60–69 |
04 (33.3) |
|||
|
70–79 |
00.00 |
|||
|
≥80 |
02 (100.0) |
|||
|
Total |
27 (27.0) |
|||
|
2 |
Gender |
Male |
21 (28.8) |
0.43 (0.51) |
|
Female |
06 (22.2) |
|||
|
3 |
Socioeconomic status |
APL |
25 (26.9) |
0.009 (0.92) |
|
BPL |
02 (28.6) |
|||
|
4 |
Behavioral factors |
Smoker |
07 (29.2) |
2.43 (0.48) |
|
Alcoholic |
06 (42.9) |
|||
|
Smoker and alcoholic |
02 (22.2) |
|||
|
5 |
Presence of comorbidity |
Diabetes |
08 (61.5) |
9.81 (p < 0.05)a |
|
Hypertension |
03 (23.1) |
|||
|
COPD |
01 (25.0) |
|||
|
Asthma |
00 (0.0) |
|||
|
6 |
Severity of illness |
Mild |
12 (18.2) |
8.82 (p < 0.05)a |
|
Moderate |
07 (36.8) |
|||
|
Severe |
08 (53.3) |
|||
In this study, anxiety was found in 67% COVID-19 patients, mild anxiety in 54%, moderate in 11%, and severe anxiety in 2% (Fig. 1). Mean GAD-7 score was 5.81 ± 3.70, and when GAD-7 score of anxiety was compared with severity of illness, it was found to be statistically significant (p < 0.05).
Table 3 depicts the various associations of anxiety with age group, gender, socioeconomic status, behavioral factors, presence of comorbidity, and severity of illness. We found this association statistically significant in the presence of comorbidity and severity of illness (p < 0.05), while it was not statistically significant with regard to age group, gender, behavioral factors, and socioeconomic status.
|
S no. |
Variable name |
Subgroups |
Anxiety (%) |
Chi-square value (p-value) |
|---|---|---|---|---|
|
Abbreviations: APL, above poverty line; BPL, below poverty line; COPD, chronic obstructive pulmonary disease. aStatistically significant. |
||||
|
1 |
Age (years) |
18–29 |
20 (71.3) |
21.41 (0.30) |
|
30–39 |
14 (26.3) |
|||
|
40–49 |
07 (44.7) |
|||
|
50–59 |
14 (77.8) |
|||
|
60–69 |
07 (59.3) |
|||
|
70–79 |
03 (60.0) |
|||
|
≥80 |
02 (100.0) |
|||
|
Total |
67 (67.0) |
|||
|
2 |
Gender |
Male |
47 (74.4) |
0.93 (0.18) |
|
Female |
20 (61.3) |
|||
|
3 |
Socioeconomic status |
APL |
62 (76.4) |
1.45 (0.70) |
|
BPL |
05 (71.4) |
|||
|
4 |
Behavioral factors |
Smoker |
14 (59.3) |
10.22 (0.33) |
|
Alcoholic |
07 (50.0) |
|||
|
Smoker and alcoholic |
08 (89.9) |
|||
|
5 |
Presence of comorbidity |
Diabetes |
11(84.6) |
24.16 (p < 0.05)* |
|
Hypertension |
10 (76.9) |
|||
|
COPD |
03 (75.0) |
|||
|
Asthma |
01 (33.7) |
|||
|
6 |
Severity of illness |
Mild |
39 (59.9) |
27.41(< 0.05)a |
|
Moderate |
14 (73.7) |
|||
|
Severe |
14 (93.3) |
|||
In this study, sleep quality disturbance was found in 62% patients and mean PSQI score was 8.84 ± 3.28; when PSQI score was compared with severity of illness, it was found to be statistically significant (p < 0.05).
Table 4 depicts the various association of sleep quality disturbance with age group, gender, socioeconomic status, behavioral factors, presence of comorbidity, and severity of illness. We found this association statistically significant in severity of illness (p < 0.05), while it was not statistically significant with regard to age group, gender, behavioral factors, socioeconomic status, and presence of comorbidity.
|
S. no. |
Variable name |
Subgroups |
Sleep quality disturbance (%) |
Z value, p-value |
|---|---|---|---|---|
|
Abbreviations: APL, above poverty line; BPL, below poverty line; COPD, chronic obstructive pulmonary disease. aStatistically significant. |
||||
|
1. |
Age (years) |
18–29 |
14 (50) |
0.93 (0.16) |
|
30–39 |
14 (73.7) |
|||
|
40–49 |
07 (43.7) |
|||
|
50–59 |
14 (77.80) |
|||
|
60–69 |
09 (75.0) |
|||
|
70–79 |
02 (40.0) |
|||
|
≥80 |
02 (100) |
|||
|
Total |
62 (62.0) |
|||
|
2. |
Gender |
Male |
44 (60.30) |
0.86 (0.35) |
|
Female |
18 (66.66) |
|||
|
3. |
Socioeconomic Status |
APL |
57 (61.20) |
0.23 (0.63) |
|
BPL |
05 (71.40) |
|||
|
4. |
Behavioral factors |
Smoker |
16 (66.66) |
0.41 (0.33) |
|
Alcoholic |
08 (57.10) |
|||
|
Smoker and alcoholic |
06 (66.67) |
|||
|
5. |
Presence of comorbidity |
Diabetes |
11 (84.60) |
4.55 (0.34) |
|
Hypertension |
9 (69.20) |
|||
|
COPD |
02 (50) |
|||
|
Asthma |
1 (33.70) |
|||
|
6. |
Severity of illness |
Mild |
31 (46.96) |
18.43 (p < 0.05)a |
|
Moderate |
16 (84.20) |
|||
|
Severe |
15 (100) |
|||
Discussion
The quality of life of people worldwide has been affected by this COVID-19 outbreak, and the impact of this disease on mental health can be quite complex.16 An association between epidemic and mental disorder has been found from the studies during the outbreak of SARS and MERS outbreak in the past.19 20 Similarly, in previous studies, higher risk of psychiatric impairment was identified in a significant proportion of patients of H1N1.21 22 In this study, depression (27%), anxiety (67%), and sleep quality disturbance (62%) were found in COVID-19 patients. Wang et al found in their study that 53.8% of individuals among general population experienced severe psychological effects of this outbreak.23
In this study, depression was found in 27% patients and males experienced more depression than females (21% vs. 06%). Depression was associated with presence of comorbidity and severity of illness, and this association was statistically significant (p < 0.05). In other studies, prevalence of depression was found to be 8.3 to 48.3% in China,24 25 25% in India, and 15.4 to 17% in Italy among general population.26 27
In this study, we found anxiety in 67% cases; among them, 47% were male and 20% were female. We found 54% mild, 11% moderate, and 2% severe anxiety cases in the study. The association of anxiety with severity of illness (p < 0.05) and presence of comorbidity (p < 0.05) were statistically significant. Xiao et al found high levels of anxiety and stress in their study done on medical staff in China.28
Anxiety was found as predominated manifestation of emotion in the study done by Lima et al.29 The prevalence of anxiety was reported in 2 to 37% of general Chinese population;24 26 30 31 in India, prevalence of anxiety was reported to be approximately 28%.26 30
In this study, sleep quality disturbance was found in 62% cases; among them, 44% male and 18 were female. The association of sleep disturbance with severity of illness was also statistically significant (p < 0.05); however, in recent studies, the prevalence of insomnia reported in China ranged from 18.2 to 23.2%.24 31
Qiu et al conducted a study in Chinese population and found 34.43% were experiencing psychological distress.32 Bo et al included an online assessment of attitudes toward mental health services and a screener for posttraumatic stress disorder (PTSD) symptoms in stable COVID-19 patients (n = 714) in Wuhan, China. They found approximately half of these subjects felt that available psychological interventions were helpful (49.8%). The prevalence of psychological distress among COVID-19 patients was understandably much higher.33 It has been found that physical distancing, severity of disease, unpredictability, and misinformation, can cause anxiety and fear.34 In recent study, it has been seen that those patients who were kept in isolation and quarantine suffered higher level of stress and anxiety.7
Conclusion
Psychological stress is one of the important aspects in the management of COVID-19 patients. In this study, we found that depression was 27%, anxiety was 67%, and sleep disturbance was 63% among admitted COVID-19 patients. Depression was statistically significantly associated with age group, presence of comorbidity, and severity of disease. Anxiety was statistically significantly associated with presence of comorbidity and severity of disease, and sleep disturbance was statistically significantly associated with severity of illness.
The psychological problems among COVID-19 patients commonly related to consequences of disease, severity of illness, and contagiousness of the disease. Therefore, in this present pandemic situation, it is more important to identify these psychological problems among COVID-19 patients, so that better care and timely interventions can be arranged with respect to psychological issues.
Limitations
This is a single-center, cross-sectional study which limits the generalizability of our findings. Therefore, further research should be done regarding evaluation of psychological problems and their interventions in COVID-19 patients.
Ethical Approval
Informed written consent was obtained from each participant at the time of their enrollment in the study. `Ethical clearance was taken from the Ethical Committee of the University before the commencement of the study.
Conflict of Interest
None declared.
Funding None.
References
- Viral encephalitis: neuropsychiatric and neurobehavioral aspects. Curr Psychiatry Rep. 2004;6(5):372-379.
- [Google Scholar]
- Neuropsychiatric manifestations of HIV infection and AIDS. J Psychiatry Neurosci. 2005;30(4):237-246.
- [Google Scholar]
- Neuropsychiatric aspects of HIV infection among older adults. J Clin Epidemiol. 2001;54(01):S44-S52.
- [Google Scholar]
- Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565-574. (10224)
- [Google Scholar]
- Human coronaviruses and other respiratory viruses: underestimated opportunistic pathogens of the central nervous system? Viruses. 2019;12(1):14.
- [Google Scholar]
- Neurologic alterations due to respiratory virus infections. Front Cell Neurosci. 2018;12:386.
- [Google Scholar]
- The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912-920. (10227)
- [Google Scholar]
- Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368:m1211.
- [Google Scholar]
- Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228-229.
- [Google Scholar]
- The SARS-associated stigma of SARS victims in the post-SARS era of Hong Kong. Qual Health Res. 2008;18(6):729-738.
- [Google Scholar]
- The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7(3):e14.
- [Google Scholar]
- Depressive symptoms after critical illness: a systematic review and meta-analysis. Crit Care Med. 2016;44(9):1744-1753.
- [Google Scholar]
- Prevalence of Depression, Anxiety, and Stress during COVID-19 Pandemic. J Neurosci Rural Pract. 2020;11(4):519-525.
- [Google Scholar]
- The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613.
- [Google Scholar]
- A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092-1097.
- [Google Scholar]
- The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213.
- [Google Scholar]
- Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. 2007;52(4):241-247.
- [Google Scholar]
- The forgotten plague: psychiatric manifestations of Ebola, Zika, and emerging infectious diseases. J Glob Infect Dis. 2017;9(4):151-156.
- [Google Scholar]
- REVA Study Group. Long-term outcomes of pandemic 2009 influenza A(H1N1)-associated severe ARDS. Chest. 2012;142(3):583-592.
- [Google Scholar]
- Depression and the risk of severe infections: prospective analyses on a nationwide representative sample. Int J Epidemiol. 2016;45(1):131-139.
- [Google Scholar]
- Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729.
- [Google Scholar]
- Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954.
- [Google Scholar]
- Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15(4):e0231924.
- [Google Scholar]
- Depression, anxiety, and stress and socio-demographic correlates among general Indian public during COVID-19. Int J Soc Psychiatry. 2020;66(8):756-762.
- [Google Scholar]
- Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica. 2020;36(4):e00054020.
- [Google Scholar]
- The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26:e923549.
- [Google Scholar]
- The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease) Psychiatry Res. 2020;287:112915.
- [Google Scholar]
- Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr. 2020;51:102083.
- [Google Scholar]
- Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med. 2020;74:39-47.
- [Google Scholar]
- A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33(2):e100213.
- [Google Scholar]
- Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med 2020 (e-pub ahead of print)
- [CrossRef] [Google Scholar]
- Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. 2020;16(10):1732-1738.
- [Google Scholar]






