Translate this page into:
Arterial infarct following surgery for pituitary adenoma
Address for correspondence: Dr. Narasinga Rao K.V.L, Department of Neurosurgery, National Institute of Mental Health and Neuro Sciences, Bangalore, Karnataka, India. E-mail: neuronarsi@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
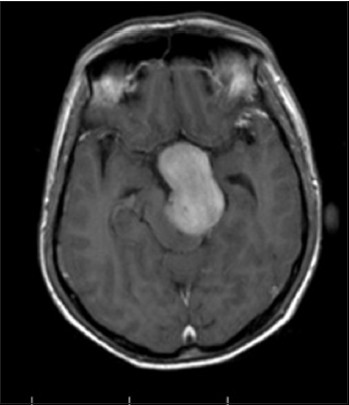
Transsphenoidal surgery for pituitary adenomas is a routine, safe, and widely accepted procedure.[1] Vascular complications following this surgery are very rare, but whenever they occur they are fatal.[2] We are reporting three cases of post-operative arterial infarcts that had fatal outcome, two of them following transsphenoidal decompression and one following the transcranial decompression of large pituitary adenomas. In case 1, a 29-year-old female had large sellar, supra-sellar mass measuring 4.7 × 3.4 × 5.1 cm. The tumor was reaching up to the floor of 3rd ventricle superiorly and encasing the bilateral internal carotid artery (ICA) to the sides. Clinically she had no perception of light in the left eye and was barely able to count fingers on the right side at 1 meter. She was operated by transspheoidal approach, partial decompression done [Figure 1]. On the 10th post-op (post-operative) day she developed left ICA infarct, and lapsed into altered sensorium with weakness in the right half of the body [Figures 2 and 3]. In case 2, a 50-year-old male, had large mass measuring 4.8 × 4 × 5.5 cm in sella with supra-sellar extension up to foramen Monro and obstructive hydrocephalus [Figures 4 and 5]. He was operated by the same transsphenoidal route, partial decompression done, developed infarct in right ACA territory [Figure 6] on the second post-op day. In case 3, a 42-year-old male underwent bifrontal craniotomy subfrontal approach and decompression for large pituitary adenoma [Figure 7], who developed infarct in the left thalamus on the fourth post-op day though, there was no vascular injury noted intra-operatively [Figure 8]. All the three cases ultimately succumbed, despite decompressive craniectomy and best medical management was done.
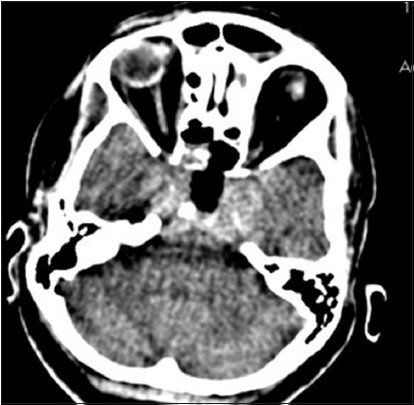
- Case 1: CT scan brain plain done on 1st post op day showing partial decompression of the tumor with a residual tumor in sella supra-sellar region and bilateral cavernous sinuses
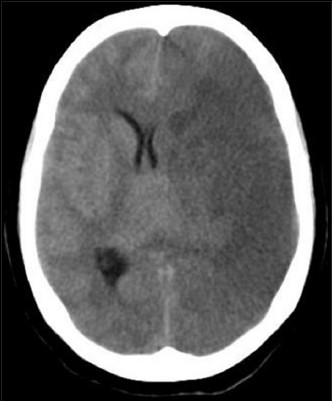
- Case 1: CT scan brain plain done on 10th post op day showing LT ICA infarct
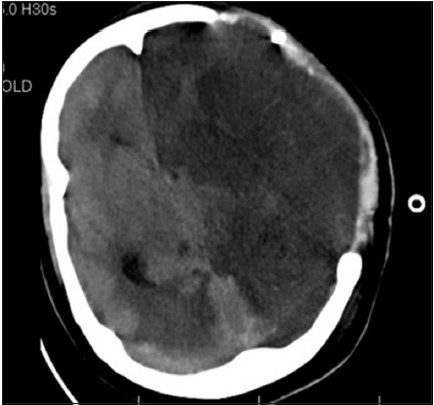
- Case 1: CT scan brain plain after decompressive craniectomy showing established LT ICA infarct with evolving RT PCA infarct
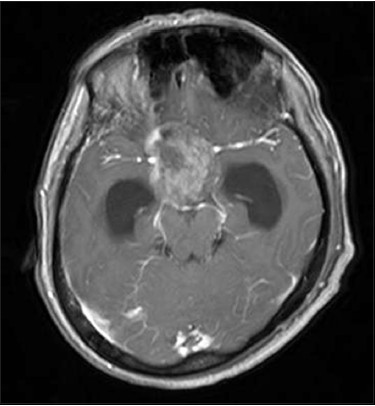
- Case 2: MRI brain contrast axial section showing displacement of both ICA
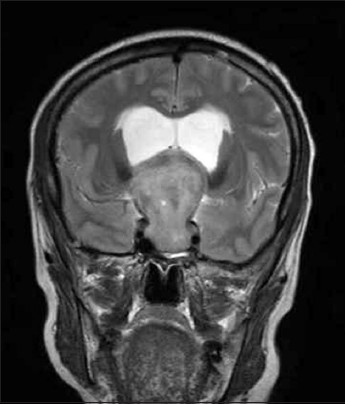
- Case 2: MRI T2WI coronal section showing large tumor with supra-sellar extension to foramen of Monro with obstructive hydrocephalus and elevation of both ACA

- Case 2: Post-op CT scan on the second post-op day showing residual tumor with an increase in hydrocephalus and RT ACA infarct
- Case 3: MRI contrast axial section showing large pituitary adenoma with compression of LT cerebral peduncle

- Case 3: Post op CT scan done on the fourth post-op day showing infarct in LT thalamus
Vascular occlusion leading to infarcts can occur in large pituitary adenomas either spontaneously or post operatively. Thirteen cases of spontaneous infarcts in various territories following of pituitary apoplexy are described literature previously.[34] Post-operative vascular occlusion can be due to overzealous packing of sella or due to post-operative edema/hemorrhage in the residual tumor. S. Kurschel described ICA infarct in pituitary adenoma following partial decompression by the transsphenoidal route[5] and Goel reported in two cases operated by the transcranial route.[6] Both of them attributed compression of vessels by edema/hemorrhage in residual tumor. Post-operative Vasospasm is also described as the possible mechanism of vascular infarcts in four reported cases.[7] Various possible causes for vasospasm after surgery include direct mechanical damage to arterial walls, blood in the basal cisterns, meningitis, or release of some chemical substances during tumor removal. Interesting points in these cases are, all the tumors were large and had significant cavernous sinus and supra-sellar extensions. In one case ICA is totally encased by the tumor. These findings prompted us to propose a novel mechanism for the cause of ICA infarct. The changes in the tumor which occur following surgery surrounding the ICA may literally strangulate ICA which as it is already compromised by the tumor [Figures 9 and 10]. We did a decompressive craniectomy for the all cases to prevent herniation; however none of the patients survived. A pre-op MRI finding of encasement of ICA should alert the neurosurgeon to this rare complication.
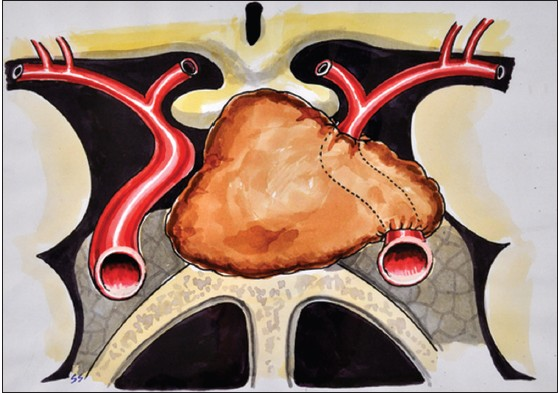
- Artist's impression of encasement of ICA by tumor before surgery
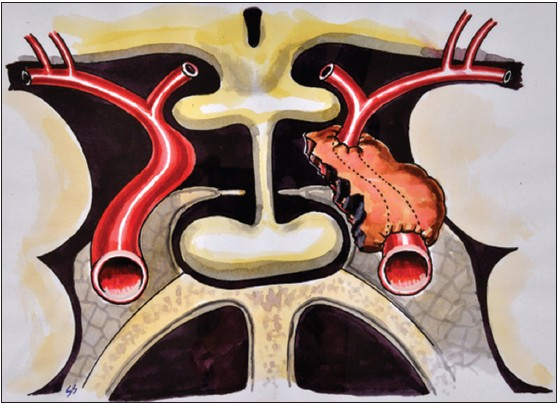
- Artist's impression of strangulation of ICA by residual tumor after the surgery
References
- Transsphenoidal microsurgery of the normal and pathological pituitary. Clin Neurosurg. 1969;16:185-217.
- [Google Scholar]
- Surgical results for pituitary adenomas: Results of an international survey. In: Black P, Zervas NT, Ridgeway E, eds. Secretory Tumors of the Pituitary Gland. New York: Raven Press; 1984. p. :377-85.
- [Google Scholar]
- Pituitary apoplexy producing internal carotid artery compression: A case report. J Korean Med Sci. 2008;23:1113-7.
- [Google Scholar]
- Pituitary apoplexy associated with a triple bolus test. Case report. J Neurosurg. 1984;61:586-90.
- [Google Scholar]
- Rare fatal vascular complication of transsphenoidal surgery. Acta Neurochir (Wien). 2005;147:321-5.
- [Google Scholar]
- Fatal postoperative ‘pituitary apoplexy’: Its cause and management. Br J Neurosurg. 1995;9:37-40.
- [Google Scholar]
- Post operative‘pituitary apoplexy’ in giant pituitary adenomas: A series of cases. Neurol India. 2005;53:326-8.
- [Google Scholar]





