Translate this page into:
Ankylosing spondylitis masquerading as generalized spasticity in a patient with spinal cord injury in neurological rehabilitation setting: A case report
*Corresponding author: Meeka Khanna, Department of Neurological Rehabilitation, NIMHANS, Bengaluru, Karnataka, India. meekakhanna@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sannyasi G, Khanna M, Gupta A, Prakash N. Ankylosing spondylitis masquerading as generalized spasticity in a patient with spinal cord injury in neurological rehabilitation setting: A case report. J Neurosci Rural Pract 2023;14:346-8.
Abstract
A thorough history and examination in rehabilitation settings are paramount. We present a case of spinal cord injury with quadriparesis with severe axial stiffness and increasing spasticity not responding to high doses of medication. Only after repeated inquiry, patient gave history of symptoms suggestive of ankylosing spondylitis (AS). Initiating treatment for AS resulted in decreased stiffness and spasticity and improved functional outcome in the patient.
Keywords
Ankylosing spondylitis
Spinal cord injury
Rehabilitation
INTRODUCTION
Ankylosing spondylitis (AS) is a seronegative spondyloarthropathy that primarily affects young men’s vertebral column and sacroiliac joints. It is characterized by ossification of the vertebral discs, joints and ligaments leading to progressive pain, stiffness, rigidity, and thoracolumbar kyphotic deformity. AS is occasionally diagnosed late and the interval between the onset of symptoms and diagnosis may take on average 8–11 years.[1] People diagnosed with AS are at risk of developing a vertebral fracture, even with minor trauma, due to the altered biomechanics of the ankylosed and osteoporotic spine. Cervical vertebral fracture is the most common among AS patients.[2]
CASE REPORT
A 39-year-old male, businessman by profession, diagnosed case of traumatic cervical spinal cord injury (SCI), presented to our neurological rehabilitation outpatient department with complaints of worsening in walking and generalized stiffness for 1 year. He had an alleged history of a trivial ground level fall at washroom in March 2021, leading to weakness of all four limbs. MRI spine at time of injury showed C4-5 subluxation with cord edema extending from C4 to 5. He underwent surgical fixation elsewhere. There was gradual sensorimotor recovery in all four limbs over next 6 months. He started walking with the help of one person support for a short distance. He experienced severe stiffness in the whole body despite taking multiple anti-spasticity medication (Tablet Baclofen 60 mg, Tizanidine 12 mg, and Tolperisone 900 mg in divided doses in a day). He came to us for further opinion.
The patient was admitted in neurological rehabilitation ward for evaluation and further management. On examination, he was classified as ASIA D SCI with neurological level at C5. He had predominantly axial stiffness along with MAS 1 + spasticity in bilateral wrist flexor, triceps, hamstring, and gastrocnemius muscle. Schober test was positive, FABER was negative. On detailed history taking, he revealed history of early morning stiffness in low back for the past 10 years for which he used to take over the counter medication. He could carry out his daily activities without difficulty before SCI. He denied any history of red eye, burning micturition, altered bowel habits, and skin or nail lesions. At that time, he was diagnosed with AS but patient was reluctant to take medicines for long-term and discontinued medication on his own. Radiographic evaluation was subsequently done, suggesting bridging syndesmophytes with bilateral sacroiliitis [Figures 1 and 2]. MRI of cervical spine showed myelomalacic changes at C4 spinal level [Figure 3]. The pulmonary function test revealed severe restrictive lung disease. Rheumatology consultation was sought and patient was diagnosed with AS and started on tablet methotrexate and injection etanercept. Gradually, his anti-spasticity medication was tapered and he was managed with Tablet Baclofen 30 mg in a day. The urodynamic study revealed good cystometric capacity and terminal detrusor overactivity with detrusor-sphincter-dyssynergia. He was advised to continue voluntary voiding with tamsulosin 0.4 mg once a day.

- X-ray of the dorsal spine of the patient showing classical bamboo spine in ankylosing spondylitis (AS).

- X-ray of the lumbar spine of the patient showing classical syndesmophytes and osteopenia in AS.
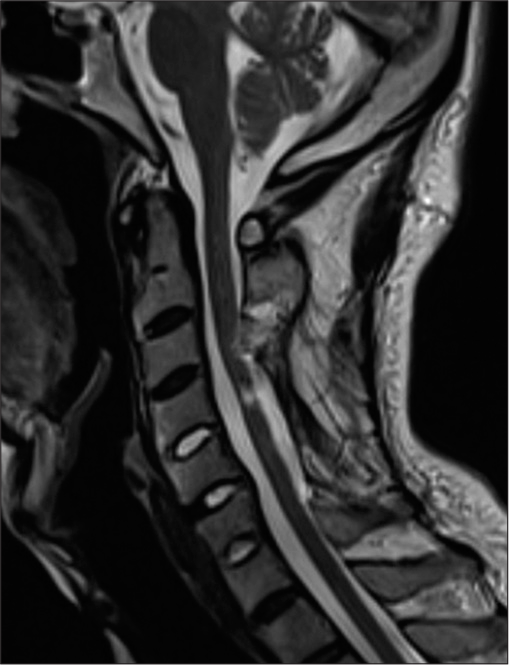
- MRI of cervical spine of patient showing myelomalacic changes.
A customized rehabilitation plan was formulated for the patient. In physiotherapy, the focus was on gentle ROM exercise of the thoracolumbar spine, strengthening exercises, and gait training. Initially, he was trained to walk inside parallel bars that progressed to walking with a walker. Occupational therapy included activities of daily living assessment and training. Psychosocial counseling was initiated to alleviate the distress.
DISCUSSION
AS is a chronic autoimmune inflammatory condition that causes severe low back pain, spinal deformity and can be associated with extra-articular features. In addition, this rigid spinal column becomes osteoporotic due to demineralization by enhanced bone resorption. The vertebral column in AS patients behaves like a long bone due to the loss of flexibility that has a propensity to fracture with minor forces.[3] In people with SCI, spasticity occurs below the neurological level. People with incomplete SCI suffer more severe grade spasticity than complete spinal cord injuries.[4] A thorough history and examination in rehabilitation settings cannot be overemphasized. In patients with SCI, development of spasticity is natural phenomenon; however, spasticity reduces as the muscle power improves with an increment of ASIA grading. In this case, the patient had predominantly axial stiffness than spasticity. A young patient with a history of neurological deficits following trivial trauma should raise a suspicion of pathological vertebral fracture that warrants further investigation.[3] The diagnosis of AS is usually based on a combination of symptoms, physical examination, imaging, laboratory testing, and contextual factors. Early diagnosis and treatment can delay the progression of disease and can prevent many complications such as osteoporosis. In this case, the patient had neglected his initial low back pain symptoms that progressed leading to bony changes before the fall. Knowledge about fall prevention strategies may result in a substantial decline in traumatic fractures in people with AS.[5] A rational understanding of patient-specific demands, individual comorbidities, and knowledge of treatment options for the underlying conditions are helpful during the rehabilitation of SCI patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Age at disease onset and diagnosis delay in HLA-B27 negative vs. positive patients with ankylosing spondylitis. Rheumatol Int. 2003;23:61-6.
- [CrossRef] [PubMed] [Google Scholar]
- Spinal fractures in patients with ankylosing spinal disorders: A systematic review of the literature on treatment, neurological status and complications. Eur Spine J. 2009;18:145-56.
- [CrossRef] [PubMed] [Google Scholar]
- Spinal cord injury in patients with ankylosing spondylitis: A 10-year review. Spine (Phila Pa 1976). 2007;32:2989-95.
- [CrossRef] [PubMed] [Google Scholar]
- Management of spasticity after spinal cord injury: Current techniques and future directions. Neurorehabil Neural Repair. 2010;24:23-33.
- [CrossRef] [PubMed] [Google Scholar]
- Retrospective analysis of spinal trauma in patients with ankylosing spondylitis: A descriptive study in Indian population. Spinal Cord. 2015;53:353-7.
- [CrossRef] [PubMed] [Google Scholar]






