Translate this page into:
Analysis and Clinical Importance of Skull Base Fractures in Adult Patients with Traumatic Brain Injury
Address for correspondence: Dr. Milesh Nagar, Department of Neurosurgery, Government Medical College, Thiruvananthapuram - 695 011, Kerala, India. E-mail: millesh.kem@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aims and Objectives:
Basal skull fracture (BSF) is rare in head injury (HI) patients and occasionally goes unnoticed which may lead to cerebrospinal fluid (CSF) fistula. With changing trends in HI, there is a need to reassess incidence and pattern of BSF pattern, CSF leak, meningitis, and management protocol, especially in this part of the world where detailed literature is lacking.
Subjects and Methods:
We closely followed adult patients admitted with BSF in our institute between January 2013 and December 2014. Associated clinical features were recorded. In case of CSF leak, detailed CSF study was done and patients were managed accordingly. Patients with persistent CSF leak were managed surgically.
Results:
During the study period, 194 of 5041 HI patients had evidence of BSF (3.85%). BSF was most commonly associated with moderate-to-severe HI (73.19%). About 81.44% patients were male and 29.9% were <30 years. Most common cause was road traffic accident (84.54%). Isolated anterior cranial fossa (ACF) fracture was most common (50%). About 63.92% patients had raccoon eyes. Forty-three patients had CSF leak with CSF rhinorrhea being more common. Culture of only 5 patients suggested bacterial meningitis. CSF leak lasted for more than 10 days in 8 patients, of which 4 patients required surgical repair.
Conclusions:
BSF is rare in victims of HI. It is more common in young adult males. ACF fractures are most common in our setup. Clinical signs of BSF are supportive but not definitive; high resolution computed tomography head is gold standard to detect BSF. CSF leak is rare and most of the cases can be managed conservatively. Leak persisting more than 7–10 days has high risk of developing meningitis and likely to need surgical intervention.
Keywords
Cerebrospinal fluid leak
meningitis
road traffic accident
skull base fracture
traumatic brain injury
INTRODUCTION
According to the latest data, road traffic accidents (RTAs) have emerged into the list of top 10 causes of mortality in the world. As per WHO data of 2015, it is tenth in the list and is expected to become sixth major cause of death and third leading cause of disability-adjusted life years lost by 2020 globally. Most important to note is that it is the most common cause of death among young people (15–29 years) globally.[123] The condition may even be worse in developing countries like India due to inadequate implementation of data collection system where head injury (HI) appears to be the single most common cause of mortality, morbidity, and loss of productivity among cases of RTA.[45]
With the rising trend in HI associated with RTA and mortality due to the severe head injuries, much more emphasis has been given to extradural hematoma, subdural hematoma, intracerebral hematoma, depressed fracture, and other facial injuries, which are either clinically and/or radiologically distinct with obvious findings whereas basal skull fracture (BSF) may occasionally go unnoticed due to suboptimal computed tomography (CT) brain as many patients are alcoholic as well as irritable and hence are not cooperative during the study. Moreover, there is heavy work load in emergency setup for the radiologist, trauma team and neurosurgeon, so BSF may further remain undiagnosed.
BSF following trauma predisposes to the formation of cerebrospinal fluid (CSF) leak and CSF fistula which is the most frequent complication of BSF.[67] Sometimes, fistula formation may be delayed and may get missed initially.[89] Patients with CSF fistula have higher chances of contracting meningitis and may require surgical intervention.[10]
The cause and pattern of BSF and pattern of CSF leak is also different in various parts of the world.[11] With recent surge of HI in spite of better and strict implementation of traffic rules, there is a need to reassess BSF pattern, incidence and pattern of CSF leak and meningitis and management protocol in head trauma patients, especially in this part of the world as most of the recent literature is from the western world.[1213141516]
SUBJECTS AND METHODS
We closely followed the patients who had high resolution CT (HRCT) scan (1 mm thickness) and/or clinical evidence of BSF admitted between January 2013 and December 2014 at our institute. Patients were evaluated with detailed history and repeated clinical examinations during the course of the hospital stay. Patient characteristics in the form of age and sex were recorded. The clinical features in the form of ear bleed or nose bleed at the time of admission, raccoon eyes, postauricular ecchymosis, and CSF leak if any were recorded. If there was any CSF leak, detailed CSF studies were done and patients with meningitis were treated with appropriate antibiotics. For the first 2–3 days, patients were managed conservatively. Those with persistent CSF leaks or high-volume CSF leak at presentation were further investigated with cisternography to localize the site of CSF leak. Patients with persistent CSF leak were operated. Data were analyzed using Statistical Package for the Social Sciences (SPSS) software (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp).
RESULTS
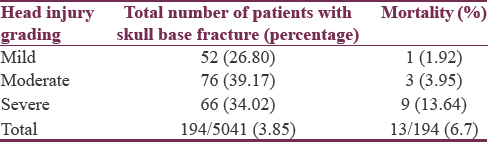
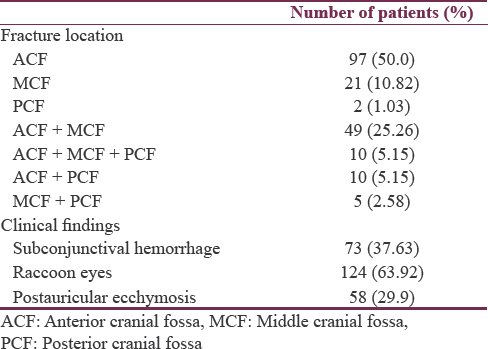
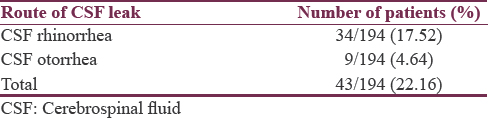
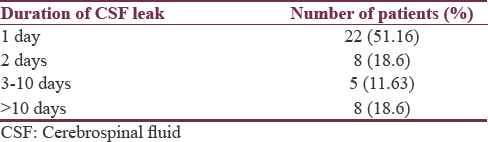
Overall 5041 adult individuals were admitted with HI, out of which only 194 patients (age range 18–86 years) had CT scan evidence of BSF (3.85%) [Table 1]. Most of the BSF were associated with moderate-to-severe head injuries (73.19%) [Table 2]. Most of the patients were male (81.44%) and were between 18 and 30 years’ age group (29.9%) [Table 3]. Overall mortality rate was around 6.7% (13 patients) and was higher in patients with severe HI (13.64%). Most common mode of injury was RTA (84.54%) [Table 3]. On CT brain, most common fracture was that of isolated anterior cranial fossa (ACF) fracture (50%) [Table 4]. Seventy-three patients (37.63%) had subconjunctival hemorrhage and 124 patients (63.92%) had raccoon eyes [Table 4]. Fifty-eight patients (29.9%) had postauricular ecchymosis [Table 4]. As many as 43 patients (22.16%) had clinical evidence of CSF leak at some time during the course of stay. Of these 43 patients, 34 (79.07%) had CSF rhinorrhea and 9 (20.93%) had CSF otorrhea [Table 5]. CSF of only 12 out of 43 (27.91%) patients with CSF leak was biochemically suggestive of meningitis, of which in only 5 patients (41.67%), culture confirmed evidence of bacterial meningitis [Table 6]. In most of the patients (22 patients; 51.16%), CSF leak subsided within 1 day whereas it lasted for more than 10 days in 8 patients (18.6%) [Table 7]. Four of these patients (9.3%) required surgical repair for the site of leak [Table 8].




DISCUSSION
Fracture of base of skull usually occurs in context of significant head trauma.[17] According to various series, BSF has been reported to occur in 3.5%–45.4% of all HI patients. Most of the published data are from the western and developed countries having lower prevalence of HI compared to underdeveloped and developing countries.[12181920] Traumatic CSF leakage is a complication in around 2% of all head injuries and in 12%–30% of all cases of BSF.[212223] In our study, BSF incidence is 3.85% (194/5041) [Table 1] whereas CSF leak was observed in 22.16% (43/194) of patients with BSF [Table 5]. Overall incidence of CSF leak in all HI patients through base of skull turned out to be 0.08% (43/5041). Similar to elsewhere, moderate-to-severe HI accounted for most of the BSF (73.19%) [Table 2].[17]
The reason of male preponderance (81.44%) in our study is because in our society, males are generally more engaged in outdoor activities, rendering them more prone to trauma when compared to the females. Most of the victims were in the age group 18–30 years (29.9%) which may be due to inexperience, tendency to take risks, and alcoholism. Relatively lower prevalence (3.85%) of BSF in our study is comparable to prevalence in developed countries. Better implementation of traffic rules and compliance of vehicle occupants with safety measures such as seatbelts for car occupants and helmets for motorcycle riders could be accounted for that.
Various studies have revealed middle cranial fossa (MCF) to be most commonly involved in BSF which has been attributed to thin bones in MCF consisting of multiple foramina.[121924] However, few others have reported ACF to be most common site of BSF.[1825] In our study, fractures of ACF (50%) followed by multiple fractures (38.14%) and MCF (10.82%) were more common [Table 3]. Posterior cranial fossa fractures are rare likely due to thick occipital bone and tendency for falling forward following RTA.[19] This is the same reason why ACF and to some extent MCF fracture is more common.
Several investigators have advocated multislice HRCT as well as various other advanced methodology in imaging to detect BSF.[2627282930] Others have specifically stressed on importance of clinical signs suggestive of BSF.[19313233] According to Pretto Flores et al., battle's sign and unilateral blepharohematoma (periorbital ecchymosis) had 100% positive predictive value (PPV) for detecting BSF while bilateral periorbital ecchymosis and otorrhagia had 70% PPV.[31] Savastio et al. proposed that rhinorrhea, otorrhea, and Battle's sign have high predictive values (100%) for intracranial sequelae.[32] Furthermore, Goh et al. found statistically significant association between clinical signs of BSF and CT findings.[33] In our series also, BSF was associated with raccoon eyes in 63.92% (124), subconjunctival hemorrhage in 37.63% (73), and Battle's sign in 29.9% (136) patients [Table 4]. Forty-three patients (22.16%) had CSF leak, of which 34 (79.07%) had rhinorrhea whereas 9 (20.93%) had otorrhea [Table 4]. There is higher prevalence of raccoon eyes and rhinorrhea as compared to other signs in our study which may be due to most of the BSF location in ACF. It is also a known fact that otorrhea in case of fracture through temporal bone tends to occur if tympanic membrane is ruptured along with temporal bone fracture whereas CSF rhinorrhea can occur through Eustachian tube.[34]
Being a high-volume center, after basic clinical examination, we first screen all patients suspected to have HI using CT brain plain with bone window. HRCT (1 mm cuts) with axial, coronal, and sagittal reconstructions is taken if there is any suspicion of BSF clinically and/or radiologically in CT brain. This saves us a lot of time and resources in emergency setup as HRCT is more time-consuming and costly compared to CT brain plain.
We admit and closely follow these patients with clinically or radiologically proven BSF and look for development of CSF leak or other signs of BSF. In case of CSF leak, lumbar puncture is done and CSF is send for evaluation of cells, glucose, protein content, Gram's staining, and culture studies. Of our 43 patients with CSF leak, 12 (27.91%) had abnormal CSF report with low sugar and high proteins, but only 5 patients (41.67%; overall 11.63% of all patients with CSF leak and 2.58% of all patients with BSF) had meningitis having positive CSF culture [Table 6]. Among these patients, most common organism isolated was Klebsiella species (60%; 3/5). Many of the early authors recommended routine use of prophylactic antibiotics in patients with BSF.[353637] However, Ratilal et al. reviewed five RCTs with 208 participants and 17 non-RCTs comparing different types of antibiotic prophylaxis with placebo or no intervention in patients with BSF and concluded that evidence from RCTs does not support use of prophylactic antibiotic in patients with BSF, whether there is CSF leakage or not.[38] Low rate of meningitis (2.85%) in BSF in our series also support the view that there is no indication to administer prophylactic antibiotics to patients with BSF propagated and proposed by many other authors recently.[123940]
Once a CSF leak is confirmed and localized radiologically, we prefer conservative management at least in first 2–3 days as a significant number of traumatic CSF leaks resolve spontaneously within the first 24–48 h. Conservative treatment consists of nursing strictly resting in bed with elevation of head end to around 30°. In addition, patients are taught to refrain from coughing, sneezing, nose blowing, and straining at stools. Stool softeners, antiemetics, and antitussives are recommended wherever indicated. Those patients in which leak persists for more than 2–3 days or with high-volume CSF leak, we do CT/magnetic resonance imaging cisternography and place lumbar drain with regular monitoring of CSF values. Those which persists more than 7–10 days have high risk of developing meningitis are likely to need surgical intervention.[2141424344] In our series, in eight patients (18.6%), CSF leak persisted for more than 10 days [Table 7], of which four (50%; 9.31% of all patients with CSF leak and 2.06% of all patients with BSF) required surgical intervention [Table 8]. In all these patients, CSF rhinorrhea was present and CSF leak was from the site in ACF. Two patients had extensive or large ACF defects and we preferred transcranial approach in them while in the remaining two patients, endoscopic transnasal repair of the defect was performed. All four patients were put on perioperative antibiotics with the advice to avoid coughing, sneezing, and straining. All of the four patients did well postoperatively. There was no recurrence.
Overall mortality in our BSF series was 6.7%. Mortality was distinctly higher in BSF patients with severe HI (13.64%) [Table 2]. Associated serious intracranial injuries accounted to the higher mortality rates in these patients. One patient each died in mild and moderate HI due to meningitis whereas other 11 patients died due to other consequences associated with HI rather than meningitis. Mortality rates due to posttraumatic CSF meningitis is quite variable in various series and ranges from 0% to 65%.[45] In our series, it is 16.67% (2/12 patients) which is much more than overall mortality due to all patients with BSF (6.7%). The only patient who died among mild HI patients was due to meningitis. This is an indicative that death in the mild to moderate HI with BSF and CSF leak can be prevented if meningitis is diagnosed and managed at appropriate time.
With changing trends of HI and safety measures, more studies are to be conducted, especially in developing countries to throw more light on the subject matter of head trauma and BSF. This study may serve as pilot study for further studies on large scale.
CONCLUSIONS
BSF is rare in victims of head trauma. It is more common in young adult males. Pattern of BSF and CSF leak varies from one region to another and knowing this fact helps to prevent the complications. ACF fractures are most common in our setup. Clinical signs of BSF are supportive but not definitive; HRCT brain scan is gold standard to detect BSF. CSF leak is rare and most of the cases can be managed conservatively under close observation. Those persisting more than 7-10 days have high risk of developing meningitis and are more likely to need surgical intervention.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 2013. World Health Organization. Road Traffic Injuries. Fact Sheet. Available from: http://www.who.int/mediacentre/factsheets/fs310/en/
- World Health Organization. Ch. 2. World Report on Road Traffic Injury Prevention. Available from: http://www.who.int/violence_injury_prevention/publications/road_traffic/world_report/chapter 2.pdf?ua=1
- 2013. World Health Organization. Road Traffic Injuries. Fact Sheet. Available from: http://www.who.int/mediacentre,/factsheets/fs358/en/
- Head injury: The principal killer in road traffic accidents. J Indian Acad Forensic Med. 2006;28:12-4.
- [Google Scholar]
- Epidemiology and clinical characteristics of traumatic brain injuries in a rural setting in Maharashtra, India 2007-2009. Int J Crit Illn Inj Sci. 2012;2:167-71.
- [Google Scholar]
- Traumatic, spontaneous and postoperative CSF rhinorrhea. In: Advances and Technical Standards in Neurosurgery. Berlin: Springer; 1984. p. :169-207.
- [Google Scholar]
- Management of closed head injury in the patient with maxillofacial trauma. J Oral Maxillofac Surg. 1993;51:298-303.
- [Google Scholar]
- Delayed presentation of traumatic cerebrospinal fluid rhinorrhea: Case report and literature review. Allergy Rhinol (Providence). 2015;6:188-90.
- [Google Scholar]
- Unusually delayed posttraumatic CSF rhinorrhea. Indian J Neurotrauma. 2010;7:171-2.
- [Google Scholar]
- The pattern of maxillofacial fractures in Sharjah, United Arab Emirates: A review of 230 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:166-70.
- [Google Scholar]
- Clinical significance of skull base fracture in patients after traumatic brain injury. J Clin Neurosci. 2016;25:111-5.
- [Google Scholar]
- Extensive traumatic anterior skull base fractures with cerebrospinal fluid leak: Classification and repair techniques using combined vascularized tissue flaps. J Neurosurg. 2016;124:647-56.
- [Google Scholar]
- Management of CSF leak in base of skull fractures in adults. Br J Neurosurg. 2016;30:596-604.
- [Google Scholar]
- A 7-year study of 1,278 patients with maxillofacial trauma and cerebrospinal fluid leak. J Maxillofac Oral Surg. 2015;14:258-62.
- [Google Scholar]
- Skull base fractures and their complications. Neuroimaging Clin N Am. 2014;24:439-65. vii-viii
- [Google Scholar]
- A comparison of temporal bone fracture classification systems. Clin Otolaryngol. 2006;31:287-91.
- [Google Scholar]
- Skull base fractures: An institutional experience with review of literature. Indian J Neurotrauma. 2013;10:120-6.
- [Google Scholar]
- Comparative analysis of clinical and computed tomography features of basal skull fractures in head injury in Southwestern Nigeria. J Neurosci Rural Pract. 2015;6:139-44.
- [Google Scholar]
- The contribution of high-resolution multiplanar reformats of the skull base to the detection of skull-base fractures. Clin Radiol. 2005;60:878-85.
- [Google Scholar]
- Management of complications from 820 temporal bone fractures. Am J Otol. 1997;18:188-97.
- [Google Scholar]
- Cerebrospinal fluid rhinorrhea in nonmissile head injuries. Clin Neurosurg. 1964;12:237-52.
- [Google Scholar]
- Computerized tomography assessment of cranial and mid-facial fractures in patients following road traffic accident in South-West Nigeria. Ann Afr Med. 2012;11:131-8.
- [Google Scholar]
- Head trauma in a newly established neurosurgical centre in Nigeria. East Cent Afr J Surg. 2008;13:86-94.
- [Google Scholar]
- Imaging of skull base cerebrospinal fluid leaks in adults. Radiology. 2008;248:725-36.
- [Google Scholar]
- Cerebrospinal fluid fistula: Frequency in head injuries. Rev Laryngol Otol Rhinol (Bord). 1992;113:423-5.
- [Google Scholar]
- Frontobasilar fractures: Proposal for image reviewing algorithm. J Craniomaxillofac Surg. 2014;42:305-12.
- [Google Scholar]
- CSF leaks: Correlation of high-resolution CT and multiplanar reformations with intraoperative endoscopic findings. AJNR Am J Neuroradiol. 2008;29:536-41.
- [Google Scholar]
- Positive predictive values of selected clinical signs associated with skull base fractures. J Neurosurg Sci. 2000;44:77-82.
- [Google Scholar]
- Cranial trauma: The predictability of the presentation symptoms as a screening for radiologic study. Radiol Med. 1991;82:769-75.
- [Google Scholar]
- Is routine computed tomographic (CT) scanning necessary in suspected basal skull fractures? Injury. 1997;28:353-7.
- [Google Scholar]
- Management of temporal bone trauma. Craniomaxillofac Trauma Reconstr. 2010;3:105-13.
- [Google Scholar]
- Role of prophylactic antibiotics in open and basilar fractures of the skull: A randomized study. Injury. 1992;23:377-80.
- [Google Scholar]
- Conservative and operative management for cerebrospinal-fluid leakage after closed head injury. Lancet. 1973;1:1013-6.
- [Google Scholar]
- Do prophylactic antibiotics prevent meningitis after basilar skull fracture? Pediatr Infect Dis J. 1991;10:87-8.
- [Google Scholar]
- Antibiotic prophylaxis for preventing meningitis in patients with basilar skull fractures. Cochrane Database Syst Rev. 2015;28(4):CD004884.
- [Google Scholar]
- Immunisations and antibiotics in patients with anterior skull base cerebrospinal fluid leaks. J Laryngol Otol. 2014;128:626-9.
- [Google Scholar]
- What is the efficacy of prophylactic antibiotics in basilar skull fractures? Laryngoscope. 2014;124:8-9.
- [Google Scholar]
- Current insights in CSF leaks: A literature review of mechanisms, pathophysiology and treatment options. Rom J Rhinol. 2017;7:143-51.
- [Google Scholar]
- Management of cerebrospinal fluid leak associated with craniomaxillofacial trauma. J Oral Maxillofac Surg. 2004;62:676-84.
- [Google Scholar]
- Endoscopic management of cerebrospinal fluid rhinorrhea. Asian J Neurosurg. 2016;11:183-93.
- [Google Scholar]
- Post traumatic meningitis: Risk factors, clinical features, bacteriology and outcome. 2004. Internet J Neurosurg. :2. Available from: http://www.ispub.com/journal/the-internetjournalof-neurosurgery/volume-2-number-1/post-traumaticmeningitisrisk-factors-clinical-features-bacteriology-andoutcome.html)
- [Google Scholar]






