Translate this page into:
An innovative low-cost head-rest for anesthesia in prone position
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A wide variety of injuries are known to occur secondary to prone positioning as a result of the pressure exerted on the dependent parts of the body. Here we would like to discuss a self-made, low-cost, head rest for prone position which we have used for more than 1100 patients.
Prone positioning is a challenging task which requires a fine tuning between anesthetic depth and maintenance of hemodynamic stability, avoiding pressure injuries at the same time. The two most commonly described injuries are ischemic optic neuropathy[12] and central retinal artery occlusion.[34]
It is warranted to turn a patient from supine to prone position carefully, avoiding excessive neck movement and allowing normal blood flow in the carotid and vertebral arteries. Blindness is a rare but devastating complication of spinal surgery in the prone position, where both prolonged duration of surgery and the magnitude of the blood loss are the risk factors.[5]
Keeping this in mind, we tried to create a face and head protection device [Figure 1]for a patient in prone keeping the head in neutral position [Figure 2]. Additionally, it provides a soft forehead and chin support along with an aperture for easy passage of the endotracheal tube (ETT). All over, it was coated with thick cotton roll of around 3.0 cm [Figure 3]. The device was placed on to the patient's face before turning them prone as that was providing better support for facial structures and ETT. Skin surface pressure on facial structures remained low due to cotton thickness as assessed intermittently during surgery. A small window is present as shown in Figure 2 for checking any pressure effect intermittently. It is made up of soft plastic pieces used for packing various delicate equipments. The length is approximately 35 cm and breadth is 30 cm. Height of the device is 15 cm with a window of 8 cm by 6 cm for checking. A 6 cm thick bar is present for forehead support and a 4 cm gap is there for the passage of ETT. This device can be reused by simply changing the cotton cover. We found it comfortable, safe and cost effective too. Literatures speak about head-rest for pediatric patients designed with the help of boxing cap[6] of different sizes. Our device is meant to be used in adult patients only.

- Depicts the final face and head protection device made by us for a patient in prone
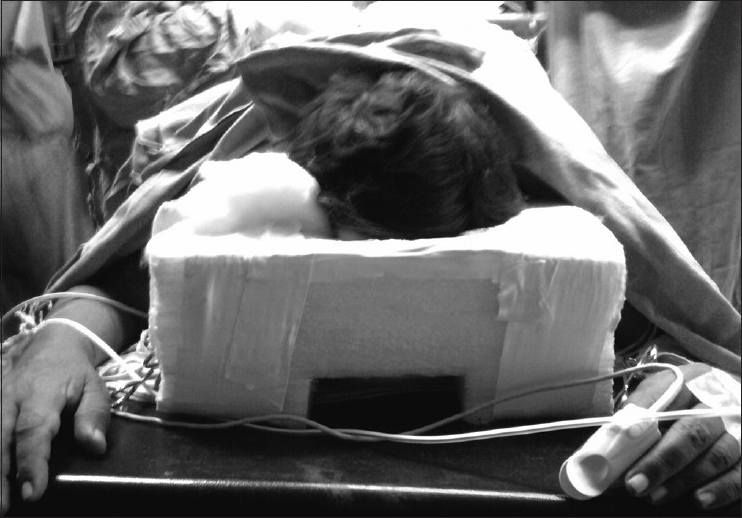
- The head of a patient supported by the device in the neutral position

- The thick cotton roll used on the device for a cushion effect
References
- Ischemic optic neuropathy following spine surgery. J Neurosurg Anesthesiol. 2005;17:38-44.
- [Google Scholar]
- Postoperative visual loss following prone spinal surgery. Br J Anaesth. 2005;95:257-60.
- [Google Scholar]
- Central retinal artery occlusion after scoliosis surgery with a horseshoe headrest. Case report and literature review. Spine (Phila Pa 1976). 1993;18:1226-8.
- [Google Scholar]
- Central retinal artery occlusion and ophthalmoplegia following spinal surgery. Br J Ophthalmol. 2004;88:1350-2.
- [Google Scholar]
- Practice advisory for perioperative visual loss associated with spine surgery: A report by the American society of anesthesiologists task force on perioperative blindness. Anesthesiology. 2006;104:1319-28.
- [Google Scholar]
- Creation of a head and face protection device for children undergoing procedures in prone position. Paediatr Anaesth. 2009;19:587-92.
- [Google Scholar]





