Translate this page into:
A Young Patient with Stroke and Primary Tuberculosis
Address for correspondence: Dr. Narenraj Arulprakash, 25B/2 Masilamanipuram, 3rd Street, Tuticorin - 628 008, Tamil Nadu, India. E-mail: naren.tr7@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A 21-year-old woman presented with left hemiparesis, fever, dyspnea, tachycardia, and pericardial rub on examination. She was provisionally diagnosed with infective endocarditis and received the final diagnosis of the primary pulmonary tuberculosis (PTB) and extra PTB (EPTB) with pericardial effusion and thoracic lymphadenitis. Left hemiparesis due to a pontine infarct was attributed to TB with neurovasculitis. The diagnosis was supported by findings on imaging studies such as echocardiography, computed tomography of the thorax, and magnetic resonance imaging of the brain. She improved with anti-TB treatment. It is interesting to note that she was not immunodeficient, with the usual suspects such as acquired immunodeficiency syndrome, diabetes mellitus, and renal failure ruled out. We conclude that PTB and EPTB must be considered in any febrile illness, even in patients who are not immunodeficient, considering its atypical presentation and prevalence in India.
Keywords
Extrapulmonary tuberculosis
neurovasculitis
pericardial effusion
pulmonary tuberculosis
INTRODUCTION
India comprises one-fourth of the global tuberculosis (TB) burden. In 2016, the World Health Organization estimated the incidence of TB in India to be 211/100,000 and the associated mortality to be 32/100,000. Extrapulmonary TB (EPTB), which accounts for one-fifth of all TB cases, has protean manifestations and uncertainty in its diagnosis and management. Although primary PTB is the common form, EPTB is usually only associated with immunodeficient conditions such as acquired immunodeficiency syndrome (AIDS), diabetes mellitus, and renal failure. A prompt diagnosis of EPTB is essential since the disease process is reversible with anti-TB treatment (ATT).
CASE REPORT
A 21-year-old unmarried woman presented with complaints of the left-sided weakness in the arm and leg, and fever with chills and rigors for 5 days. She recalled a febrile episode that occurred 2 months prior, which was treated as typhoid fever by her general practitioner. On examination, she was febrile, anemic, dyspneic, tachycardic, but not jaundiced or cyanosed. Central nervous system examination showed the left hemiparesis of the upper motor neuron type with powers of 4/5 in the upper limb and 1/5 in the lower limb. She had no cranial nerve involvement. There were no signs of meningeal involvement. Fundus examination result was unremarkable. Cardiovascular examination showed an elevated jugular venous pressure and a pericardial rub over the precordium. No petechial hemorrhages or osler's nodes were detected.
The patient was provisionally diagnosed with infective endocarditis based on high-grade fever, tachycardia, pericardial rub, and associated focal neurological deficits; she was initiated on intravenous vancomycin, ceftriaxone, and gentamicin treatment.[1] Baseline investigations revealed hemoglobin levels of 9.1 g/dL; white blood cell counts within normal limits, erythrocyte sedimentation rate of 48 mm/h, C-reactive protein levels of 2.4 mg/dL, and random blood sugar levels of 96 mg/dL. A chest X-ray revealed cardiomegaly. Renal, liver, and thyroid function test results were normal. She had underwent magnetic resonance imaging of the brain externally, which showed subacute infarct in the right pons.
In view of persistent tachycardia, high-spiking fever and worsening dyspnea, she was shifted to the Intensive care unit. A two-dimensional echocardiogram showed moderate pericardial effusion with fibrous strands suggestive of tuberculous etiology, heart valves that appeared normal, and preserved ejection fraction [Figure 1]. High-resolution computed tomography (CT) of the thorax was performed, showed necrotizing pneumonia, segmental atelectasis in the superior segment of the left lower lobe, focal consolidation, and subsegmental atelectasis in the superior segment of the right lower lobe, multiple enlarged lower paratracheal lymph nodes with central necrosis, and diffuse pericardial thickening with minimal pericardial effusion [Figures 2 and 3]. A cardiologist's opinion was obtained, who suggested performing CT-guided pericardial fluid aspiration. The patient was not willing to undergo the procedure. There was no sputum available to examine for Mycobacterium tuberculosis. Meanwhile, three samples of blood culture tested negative. A carotid Doppler study of the neck vessels revealed Grade 2 intimal changes with no flow limitations. She tested negative for human immunodeficiency virus (HIV) 1 and 2. Vasculitis screening (antinuclear antibodies, antineutrophil cytoplasmic antibodies, and rheumatoid factors) revealed negative results. Antiphospholipid titers and homocysteine levels were normal.[2]
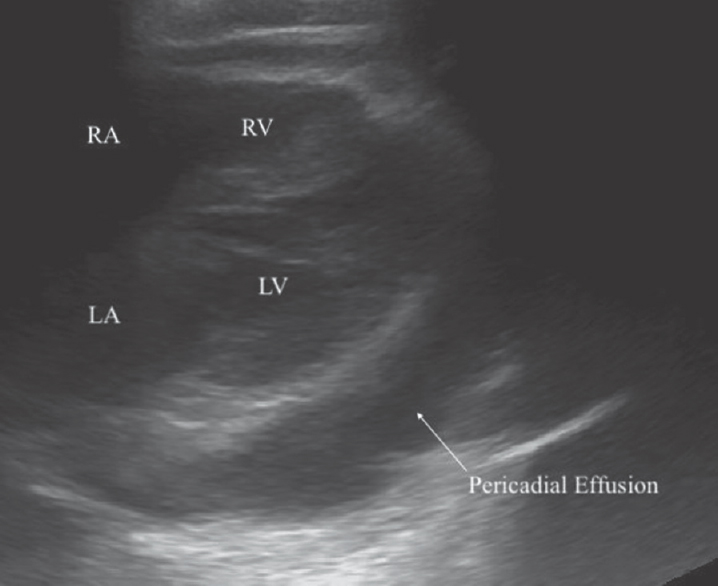
- Ultrasound: moderate Pericardial Effusion. Arrow shows echo-free signal from pericardial fluid. Fibrin strains are also seen within the fluid
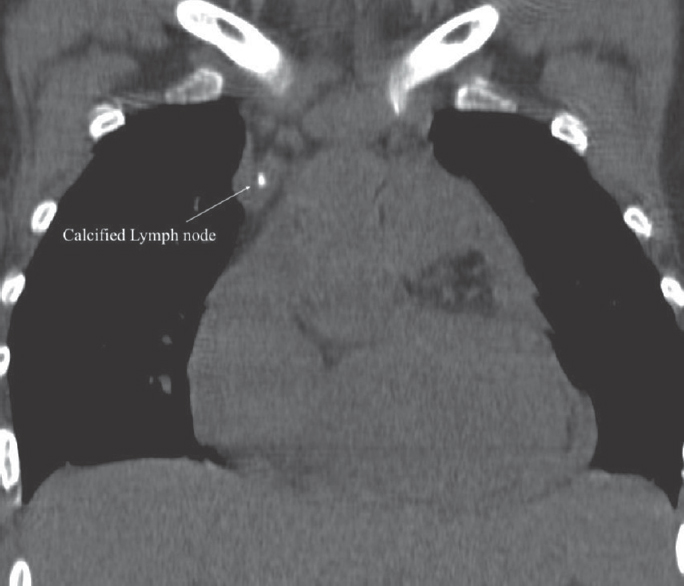
- Computed Tomography: coronal view of the thorax; Calcified lymph node. Noncontrast coronal computed tomography scan shows hyperattenuation of paratracheal lymph nodes
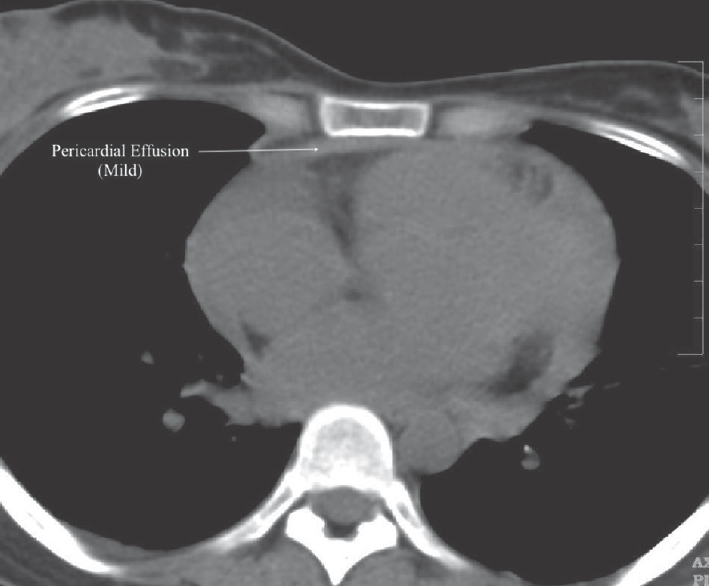
- Computed tomography: axial view of the thorax; mild pericardial effusion. Noncontrast axial computed tomography scan shows diffuse pericardial thickening and mild pericardial effusion
With this “atypical” presentation, we finally diagnosed her with primary PTB and EPTB involving the pericardium.[34] ATT was initiated with a four-drug regimen namely, isoniazid, rifampicin, pyrazinamide, and ethambutol.[5] Temperature spikes settled after a few days. There was also a mild improvement in her hemiparesis. In view of negative results for young-age stroke work-up, her hemiparesis was attributed to TB with neurovasculitis. The patient desired to be discharged at request and was advised to follow-up with the cardiologist and physician.
DISCUSSION
Primary pulmonary TB usually presents with fever, which is generally low-grade but could be as high as 102.2°F. Fever is not accompanied by other symptoms, although some patients can develop pleuritic or retrosternal chest pain. After primary infection, 90% of individuals with intact immunity enter the “latent” phase. The remaining 10% develop TB pneumonia with hilar lymphadenopathy or present with disease at more distant sites, commonly cervical lymphadenopathy, meningitis, pericarditis, or miliary dissemination. The diagnosis of PTB is definitively established by the isolation of M. tuberculosis from bodily secretions or tissue biopsies. Radiographic studies are important supportive diagnostic tools. Reactivated TB often presents with cough, weight loss, fatigue, fever, and night sweats. Radiographic studies show the involvement of the apical lobes with cavitation and fibrosis.[67] “Atypical” presentations of PTB and EPTB are usually associated with primary TB and severe immunodeficient states.[8]
Pericardial effusion in TB results from the breakdown of infection in mediastinal nodes and spreads directly into the pericardium and particularly those at the tracheobronchial bifurcation. The spread is over lymph channels that merge at points where the parietal pericardium and the pleura separate. In rare cases, there may be direct spread from tuberculous pneumonia. The onset is usually insidious with loss of weight and fatigue but could be more acute and occasionally explosive with tamponade. Other causes of pericarditis must be ruled out (viral, rheumatic, purulent, and collagen disorders). Neurological TB usually takes the form of meningitis and vasculitis of arteries of the base of skull.[9] Meningeal deposits and tuberculoma may be demonstrable in imaging studies. Xpert may be used as an adjunctive test for tuberculous meningitis but was not included in our case.[510] Studies from North and Central India concluded that pleural TB is the most common presentation of EPTB. Both PTB and EPTB affect younger individuals 20–40 years of age more commonly. Studies have also shown female preponderance among EPTB cases compared to among PTB cases. In the female population, EPTB affects younger individuals than in male patients in whom PTB was found to be more common. A higher proportion of patients with EPTB are found to be HIV-positive and have diabetes as compared to patients with PTB.
Our patient had evidence of PTB and EPTB. She did not have any immunodeficiency, AIDS, diabetes, or renal failure. The infarct in her right pons was attributed to TB with neurovasculitis. She was hence diagnosed with primary PTB and EPTB and was initiated empirically on ATT.
CONCLUSION
From our case report, we conclude that primary PTB and EPTB can masquerade as other febrile illnesses and should be differentiated even in the absence of immunodeficiency. This is also evidenced by the prevalence of TB in India. This approach would help manage a potentially curable disease and prevent its spread.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 2015 ESC guidelines for the management of infective endocarditis: The task force for the management of infective endocarditis of the European society of cardiology (ESC). Endorsed by: European association for cardio-thoracic surgery (EACTS), the European association of nuclear medicine (EANM) Eur Heart J. 2015;36:3075-128.
- [Google Scholar]
- World Health Organization. Stop TB Department. Treatment of Tuberculosis: Guidelines. Geneva: World Health Organization; 2010.
- Incidence and clinical profiles of pulmonary and extra-pulmonary tuberculosis. Int J Res Dev Pharm Life Sci 2017 doi: 10.13040/IJRDPL. 2278-0238.6(5).2773-2778
- [Google Scholar]
- Comparison of extra-pulmonary and pulmonary tuberculosis cases: Factors influencing the site of reactivation. Int J Tuberc Lung Dis. 2005;9:1220-3.
- [Google Scholar]
- Mapping the pattern and trends of extrapulmonary tuberculosis. J Glob Infect Dis. 2013;5:54-9.
- [Google Scholar]
- Clinico-epidemiological profile of extra-pulmonary tuberculosis in Central India. Int J Med Res Rev. 2016;3:2.
- [Google Scholar]






