Translate this page into:
A Study on the Clinical and Angiographic Spectrum of Spontaneous Extracranial Dissections in the Cerebral Vasculature
Address for correspondence: Col. Dr. Ravi K. Anadure, Department of Medicine, Command Hospital Air Force, Agram Post, Bengaluru - 560 007, Karnataka, India. E-mail: ravi.anadure@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
To prospectively study the clinical profile, angiographic features, and functional outcomes, in consecutive cases of extracranial dissection seen at two tertiary stroke care centers in South India.
Materials and Methods:
In this observational study, spanning 4 years (December 12–December 16), a total of 442 patients presented with an acute ischemic stroke/transient ischemic attack (TIA) at our study centers. 14/546 (3.2%) of these patients had magnetic resonance angiography (MRA)/computed tomography angiography (CTA) evidence of extracranial dissections. All cases underwent detailed clinical evaluation on arrival, and data were recorded on a predesigned stroke pro forma. Contrast MRA was done on arrival in all cases as part of a standard stroke protocol, and CTA was done only if MRA was inconclusive. The pattern of the vessel involved and morphology of vessel dissection was analyzed as per a standard radiology protocol. All the cases were managed with short-term anticoagulation using low-molecular-weight heparin followed by oral anticoagulants for 3–6 months. All cases were followed up for 1–2 years and the functional outcomes were recorded using the modified Rankin Scale (mRS).
Results:
There were 11 males and 3 females in the study, and the mean age was 45.1 years (range = 27–65 years). Focal neurological symptoms occurred in all these patients (10 patients had a stroke, and 4 had TIA). Nearly 64.2% of these (9/14) were stroke in young (age <45 years). The internal carotid artery was the most common vessel involved in 85.7% (12/14) cases. Of the ten patients with completed stroke, a good functional outcome (mRS 1–2) was seen in 8/10 (80%). Digital subtraction angiography and revascularization procedures were needed only in a minority of cases 3/14 (21%).\
Conclusion:
This hospital-based study highlights the importance of suspecting arterial dissections in young strokes of unexplained etiology, and offering optimum anticoagulant therapy in the acute phase, to achieve good long-term outcomes.
Keywords
Angiography
cerebral dissections
heparin
INTRODUCTION
Arterial dissection is an increasingly recognized cause of stroke, which accounts for up to 10%–25% of ischemic strokes in young adults.[12] Cerebral vessel dissections lead to cerebral ischemia due to either artery-to-artery embolism or due to hemodynamic failure. It was understood only in the late 1970s when Fisher et al.[1] and Mokri et al.[2] described dissections of carotid and vertebral arteries as detected by modern diagnostic approaches. Spontaneous dissections of the cerebral arteries affect all age groups, including children, but there is a distinct peak in the fifth decade of life.[34] Dissections of the carotid and vertebral arteries usually arise from an intimal tear. The tear allows blood under arterial pressure to enter the wall of the artery and form an intramural hematoma, the so-called false lumen.[5] A subintimal dissection tends to result in stenosis of the arterial lumen, whereas a sub-adventitial dissection may cause aneurysmal dilatation of the artery, often referred to as “pseudoaneurysms.” While occasional case reports and small case series exist on this subject, there is a paucity of literature from our country. We thus undertook a systematic prospective study of angiographically confirmed cases of spontaneous extracranial cerebral dissection, to bring out their wide clinical spectrum and pattern of vessel involvement along with clinical outcomes.
MATERIALS AND METHODS
This prospective observational study was carried out at the Departments of Neurology and Radiology at INHS Asvini, Mumbai and Command Hospital Air Force, Bengaluru. These are tertiary referral centers of the Armed Forces, with state-of-the-art dedicated stroke set up, including 1.5 Tesla magnetic resonance imaging (MRI), 16 Slice multidetector computerized tomography, and a digital subtraction angiography (DSA) laboratory, and get referrals from the southern and western regions of India. All cases underwent an MRI brain with contrast magnetic resonance angiography (MRA), as a part of standard stroke protocol. Where ever dissections were not conclusively established on contrast MRA, a computed tomography angiography (CTA) was in addition done to confirm the diagnosis and define the culprit vessel. The case files and neuroimaging of patients with angiographically (contrast MRA/CTA) proven spontaneous cerebral dissection were preserved and analyzed, for the period covering December 12 to December 16. The diagnosis of cerebral dissection was made based on standard clinical and neuroradiologic criteria, i.e., sudden onset of ischemic or hemorrhagic symptoms; MRI of brain consistent with clinical symptoms; and angiographic findings characteristic of arterial dissection, such as double lumen sign (the presence of a false lumen or an intimal flap), intra-mural hematoma (in vessel wall), stenosis (string sign or tapered narrowing), stenosis with dilation (pearl and string sign), smoothly tapered occlusion (flame sign), and complex pseudoaneurysm formation. Patients with histories of head trauma or cranial surgery within 6 months before onset were excluded from the study.
The following radiologic and clinical parameters were evaluated and compared: type of onset, vascular risk factors, neuroimaging features, angiographic findings, management strategy, and clinical outcome (by modified Rankin Scale [mRS]). A standard stroke MR protocol (T1, T2, fluid-attenuated inversion recovery, diffusion with ADC Maps and Gradient Echo) was followed in all cases on a 1.5 Tesla Seimens MRI machine. Neurovascular imaging by contrast MRA was performed within 24–72 h of onset in all cases. Contrast-enhanced MRA was done with dynamic coronal sequences, including the aortic arch to cranial vault, after intravenous injection of gadolinium chelate at 0.2 mmol/kg body weight. Manual scan triggering was done once contrast was noted in the proximal aorta. CTA was performed in 6 of these cases within 3–5 days after the stroke, since MRA was not conclusive for dissection in these cases. CTA was done after bolus injection of nonionic contrast (1.5 ml/kg body weight) at the rate of 4 ml/s. The acquisition was timed by bolus tracking technique with the trigger set in the ascending aorta. Caudocranial acquisition from the aortic arch to the cranial vault was obtained after minimum post threshold delay. Therapeutic DSA for mechanical thrombectomy or stenting was performed using a Siemens Polystar Top machine at Mumbai and FD 10 Philips Allura machine at Bengaluru.
RESULTS
A total of 546 MRA were done at the two institutes during the study period of 4 years (December 12 to December 16). Of these, 442 cases had an ischemic stroke/transient ischemic attack (TIA) as the clinical and radiological presentation, and 104 had hemorrhagic presentations (subarachnoid hemorrhage [SAH] or intracranial [IC] bleeds). In the ischemic subset of cases, 14/442 (3.2%) were diagnosed with cervico-vertebral dissection (extracranial). In the hemorrhagic subset, 4/104 (3.8%) had IC dissection. Major differences exist between dissections involving the IC and extracranial cervical-cephalic arteries. The plane of dissection in the cervical internal carotid artery (ICA) or vertebral artery (VA) is usually within the media.[6] Intracranially, the media is significantly simplified, and dissections of IC arteries are usually subintimal but may extend outward through the adventitia resulting in SAH. We, therefore, focused and selectively analyzed the subset of 14 extracranial dissections only [Table 1].
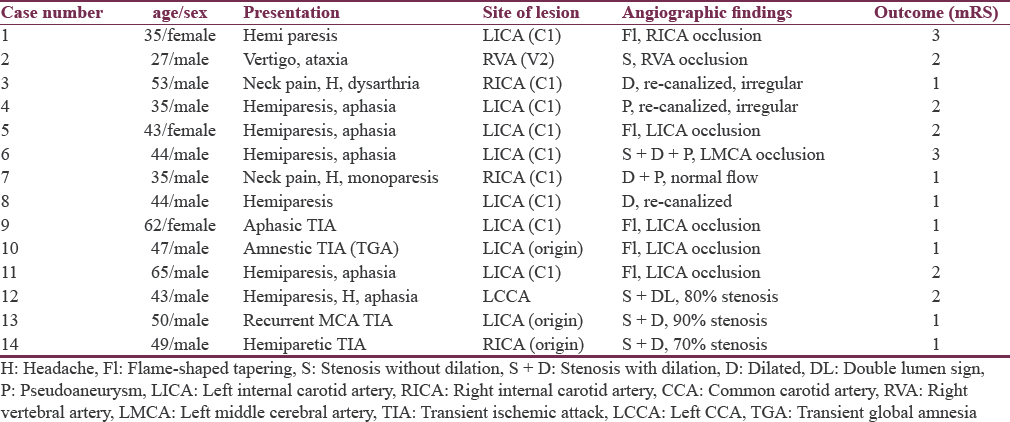
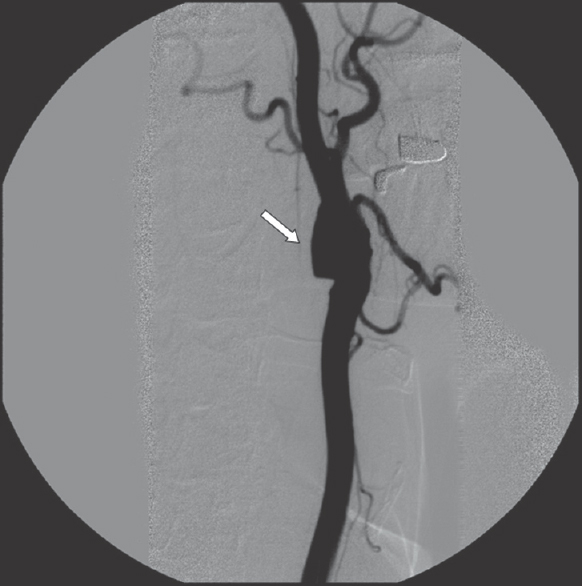
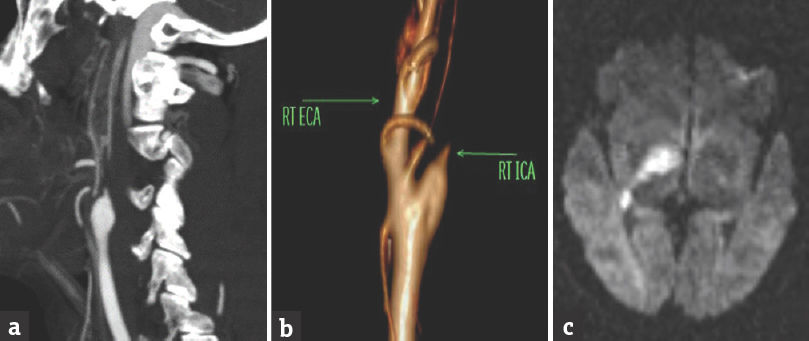
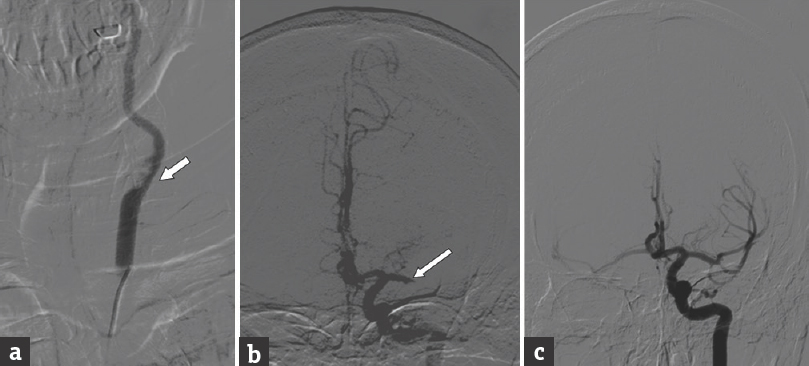
In this study, out of 546 patients presenting with an acute stroke/TIA, we had 14 patients (14/546, 2.56%) with MRA/CTA evidence of extracranial dissections, seen over a span of 4 years. Further, these constituted 3.2% (14/442) of all ischemic strokes. Focal neurological symptoms occurred in almost all these patients (10 patients had a stroke, and four had TIAs). The common carotid was involved in only one case with double lumen sign on angiogram in the bulb region [Figure 1] and distal M3 segment embolism on the same side. The angiographic features of the 12 ICAs involved by dissection were “flame-shaped” narrowing with “cutoff” in five cases [Figure 2], stenosis (usually an elongated irregular segment) in three [Figure 3a], an intimal flap in one, and pseudoaneurysm formation in three. The only VA involved by extracranial dissection on angiography showed stenosis with distal occlusion in the V3 segment and left posterior inferior cerebellar artery infarct on MRI [Figure 4]. Follow-up angiograms were available only in 4/12 left internal carotid artery (LICA) dissections at varying periods (8–12 months) and showed complete recanalization in one, partial recanalization with an irregular lumen in two and a chronic total occlusion with good collaterals in the remaining one.
- Digital subtraction angiography left common carotid artery injection: Spontaneous dissection of Left carotid bulb with a filling defect and double lumen sign
- Computed tomography angiogram maximum intensity projection (a) and volume rendering (b) showing flame shaped tapering of the right internal carotid artery distal to the carotid bulb with distal embolic infarcts (c) in right middle cerebral artery territory on diffusion magnetic resonance imaging
- Digital subtraction angiography left common carotid artery injection: (a). Left internal carotid artery origin dissection with diffuse stenosis of internal carotid artery and complete external carotid artery cut off on the same side (b). Distal embolism to left middle cerebral artery with complete M1 cut off in the intra-cranial view (c). Re-canalization of left middle cerebral artery after thrombectomy with solitaire stentriever
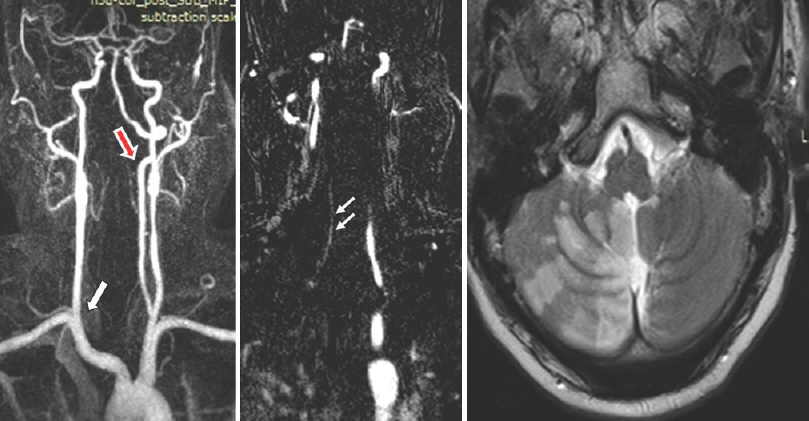
- Contrast enhanced-magnetic resonance angiography coronal images show right vertebral artery dissection (single arrow) near origin with diffuse narrowing and cut off in V2 segment (double arrow). Normal left vertebral artery (red arrow) is clearly seen. Axial T2 weighted image showing acute right posterior inferior cerebellar artery territory infarcts due to distal extension of dissection to involve the posterior inferior cerebellar artery branch from V4 segment of right vertebral artery
All these patients were treated with anticoagulants in the acute phase of the dissection (1–2 weeks) and subsequently kept on long-term anti-platelets for stroke prophylaxis. Only those patients who had disabling embolic stroke in window period or remained symptomatic with recurrent TIA or fresh strokes, despite optimized medical management, were managed with endovascular intervention. One patient with LICA dissection and embolism to left middle cerebral artery (MCA) in the hospital [Figure 3b], underwent a successful mechanical thrombectomy with a Solitaire Stentriever [Figure 3c], and made a good clinical recovery (mRS-1). Two patients in this study group had recurrent TIA of the anterior circulation despite optimal medical therapy and underwent stenting of the stenosed vessel. One had a common carotid artery disease and other an ICA (C1) segment dissection. All three cases had a favorable outcome with near complete remodeling of the diseased vessel segment on angiogram. There were no procedural complications noted. Follow-up in this entire group ranged from 1 to 2 years and no mortality was associated with cervical arterial dissections. Of the 10 patients with completed stroke, two had near complete recovery (mRS-1), and five had a mild residual neurologic deficit (mRS-2). Only two patients had a significant deficit impairing activities of daily living (mRS-3). Headache at presentation was noted in only 3/14 cases (21%). Essential hypertension was noted in 4/14 (28.5%), diabetes in 3/14 (21%), and 6/14 (42.8%) were smokers in this study group. Optimization of medical therapy in these patients needed tight blood pressure and glycemic control and smoking cessation measures. None of the patients had a history of migraine headaches or use of oral contraceptives.
DISCUSSION
Spontaneous dissections of the carotid or VA account for only about 2% of all ischemic strokes,[6] but they are an important cause of ischemic stroke in young and middle-aged patients and account for 10%–25% of such cases.[7] Overall, the extracranial ICA is the most frequently affected vessel, as was the finding in this study (12/14). In a population-based study from Rochester, Minnesota, the annual incidence of spontaneous dissections of the cervical ICA for all ages was 2.5/100,000.[8]
The management of cervico-cephalic arterial dissections remains a controversial issue. Our patients received a standardized treatment, with low-molecular-weight heparin in the acute phase and dual antiplatelets for 3–6 months. Most, but not all, focal cerebral ischemic symptoms associated with cervical arterial dissections are presumed to be thrombo-embolic in origin. Therefore, a course of anticoagulation therapy is usually recommended in patients with ischemic symptoms in the absence of intra-cranial hemorrhage or an already completed major infarct. In Intra-cranial arterial dissections, a hemodynamic mechanism due to luminal narrowing may be as important as embolic phenomena. Furthermore, some patients with intra-cranial arterial dissections may develop a SAH. Therefore, anti-coagulation therapy for this group of patients may call for caution.
Spontaneous cervical arterial dissections are generally associated with good clinical recovery. This probably is due to a higher index of suspicion and improved diagnostic methods allowing early diagnosis and treatment. In adults with spontaneous extracranial cervico-cephalic dissection, the rate of recurrent dissection during the 1st month is 2%, but from that time on, it is approximately 1% per year and inversely related to age.[3] Surgical intervention and repair or endovascular remodeling of the aneurysm are generally reserved for patients with a SAH due to an intra-cranial dissecting aneurysm or for those with an extracranial residual dissecting aneurysm that contains thrombus and causes cerebral embolization and symptoms of recurrent ischemia. 1/14 in this study had an embolic occlusion of MCA in the acute phase of stroke and benefitted from a thrombectomy. 2/14 patients in this study group had recurrent TIA/stroke despite optimum medical therapy and underwent stenting of the stenosed vessel. All three had a favorable outcome with near complete remodeling of the diseased vessel segment on angiogram. Extracranial-Intra-cranial arterial bypass operations may occasionally be justified for patients with hemodynamic cerebral ischemic symptoms caused by proximal vessel stenosis or occlusion, but this indication is rare.
The pathogenesis of arterial dissections is not clear in all cases. Mechanical factors and an underlying arteriopathy have been blamed.[910] History of a trivial and often doubtful trauma is frequent, understandably more so in children than in adults. A predisposing disorder of the arterial wall, although suspected, cannot be documented in most patients. There are reported associations of spontaneous cervico-cephalic arterial dissections with fibromuscular dysplasia, cystic medial necrosis, Marfan syndrome, Ehlers–Danlos.[111213] In the present study, no such risk factors or collagenosis could be identified clinically or angiographically.
Noninvasive vascular imaging (CT/MRA) is mandatory in the evaluation of all forms of cranio-cerberal ischemia and one or a combination of both modalities suffices in clinching the diagnosis. The characteristic angiographic finding is a long segment tapering or occlusion of the cervical ICA with typical sparing of the carotid bulb (distinguishing feature from an atherosclerotic occlusion).[14] The classic intimal flap is diagnostic, but variably seen. Evaluation of the major collaterals across the Circle of Willis helps to prognosticate the extent of likely hemodynamic cerebral compromise, and also serves to plan an endovascular intervention if needed. Intramural hematoma is less often seen in a VA dissection and the diagnosis should be suspected with observation of an increased vessel diameter and crescentic mural thickening.[15] High resolution vessel wall MRI can elegantly demonstrate the intra-mural hematoma and distinguish it from a lipid-rich plaque, in cases where a diagnostic dilemma still exists after CT/MRA.[16]
The reported rate of death from dissections of the carotid and vertebral arteries is <5%, and about three-fourths of patients who have had a stroke make a good functional recovery.[17] Headache associated with dissection resolves within a week in about 90% of patients, but in a few patients, it can persist for many years.[18] The follow-up in this study group ranged from 1 to 2 years, and no mortality was associated with cervical arterial dissections. Of the 10 patients with completed stroke, three had a near complete recovery (mRS-1) and five had a mild residual neurologic deficit (mRS-2). These findings are consistent with the findings from previous studies on this subject.[17]
Dissection of the carotid and vertebral arteries is a dynamic processes. The radiographic findings may change dramatically within a period of days or even hours. Although the radiographic appearance may worsen during the acute phase of dissection, about 90% of stenosis eventually resolve.[15] Two-thirds of occlusions are recanalized, and one-third of aneurysms decrease in size over 3–6 months.[19] Follow-up angiograms were available only in 4/14 LICA dissections in this study, at varying periods of 8–12 months, and showed complete re-canalization in one, partial re-canalization with irregular lumen in two and a chronic total occlusion with good collaterals in the remaining one. This reflects the dynamic nature of dissections as noted in previous studies.[20]
CONCLUSION
In this prospective observational study, spanning 4 years, the prevalence of extracranial dissections in ischemic stroke subset was 3.2% (14/442). 64.2% of these (9/14) were stroke in young (age <45 years), suggesting dissections as an important cause of young strokes, which requires a high index of suspicion, and special MR sequences/CTA. Therapy with short-term anticoagulation seems safe and effective with no mortality in this study and good functional outcomes (based on mRS 1–2) in 12/14 (86%) cases. DSA and revascularization procedures like thrombectomy/stenting were needed only in a minority of cases 21% (3/14) who either had window period embolic strokes or persistent symptoms despite optimum medical therapy. Unlike Western studies, arteriopathies and collagenosis are rare in an Indian population, and no such cases were identified in this study. Most cases of extracranial dissections in our population are probably still related to premature atherosclerosis or trivial trauma (often not reported). This Indian hospital-based study highlights the importance of suspecting dissections in young strokes of unexplained etiology, and offering optimum therapy in the acute phase, to achieve good long-term functional outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Spontaneous dissection of cervico-cerebral arteries. Can J Neurol Sci. 1978;5:9-19.
- [Google Scholar]
- Spontaneous internal carotid dissection, hemicrania, and Horner's syndrome. Arch Neurol. 1979;36:677-80.
- [Google Scholar]
- Follow-up of patients with history of cervical artery dissection. Cerebrovasc Dis. 1995;5:43-9.
- [Google Scholar]
- Recurrence of cervical artery dissection. A prospective study of 81 patients. Stroke. 1996;27:1804-7.
- [Google Scholar]
- Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med. 2001;344:898-906.
- [Google Scholar]
- Spontaneous dissections of cervicocephalic arteries in childhood and adolescence. Neurology. 1994;44:1607-12.
- [Google Scholar]
- Internal carotid artery dissection in a community. Rochester, Minnesota, 1987-1992. Stroke. 1993;24:1678-80.
- [Google Scholar]
- Dissections and trauma of cervicocerebral arteries. In: Barnett HJ, Stein BM, Mohr JP, Yatsu FM, eds. Stroke: Pathophysiology, Diagnosis, and Management (2nd ed). New York: Churchill Livingstone; 1992. p. :671-88.
- [Google Scholar]
- Dissecting aneurysm of superior cerebellar artery. Its association with fibromuscular dysplasia. Arch Neurol. 1983;40:120-2.
- [Google Scholar]
- Marfan's syndrome, with unusual blood vessel manifestations: Primary medio-necrosis dissection of right innominate, right carotid, and left carotid arteries. Arch Pathol. 1957;64:205-9.
- [Google Scholar]
- Three cases of spontaneous extracranial vertebral artery dissection. Stroke. 1990;21:618-25.
- [Google Scholar]
- Epidemiology, pathophysiology, diagnosis, and management of intracranial artery dissection. Lancet Neurol. 2015;14:640-54.
- [Google Scholar]
- Craniocervical arterial dissection: Spectrum of imaging findings and differential diagnosis. Radiographics. 2008;28:1711-28.
- [Google Scholar]
- Intracranial vessel wall imaging: Current applications and clinical implications. Neurovasc Imaging. 2016;2:4-8.
- [Google Scholar]
- Time course of symptoms in extracranial carotid artery dissections. A series of 80 patients. Stroke. 1995;26:235-9.
- [Google Scholar]
- Headache and neck pain in spontaneous internal carotid and vertebral artery dissections. Neurology. 1995;45:1517-22.
- [Google Scholar]
- Magnetic resonance angiography demonstrates vascular healing of carotid and vertebral artery dissections. Stroke. 1997;28:1993-7.
- [Google Scholar]
- MR angiography for the long-term follow-up of dissecting aneurysms of the extracranial internal carotid artery. AJR Am J Roentgenol. 2000;174:1137-40.
- [Google Scholar]






