Translate this page into:
A Case Report of Misdiagnosis of Psychotic Symptoms Predominant Wilson's Disease
Address for correspondence: Dr. Bhupendra Shah, Department of Internal Medicine, B.P. Koirala Institute of Health Sciences, Dharan, Nepal. E-mail: doctorbhupen@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Wilson's disease is an autosomal recessive disease of abnormal copper metabolism. Psychosis is a rare manifestation of Wilson's disease. Few cases of misdiagnosing Wilson's disease as an etiology of psychosis were reported in the literature. We report a case of a 42-year-old patient, who was diagnosed with a schizoaffective disorder and treated with antipsychotics for 3 years with no significant improvement. On reevaluation, we the patient was diagnosed to have Wilson's disease. The patient's symptoms improved significantly with chelation therapy.
Keywords
Misdiagnosis
psychosis
Wilson's disease
INTRODUCTION
Wilson's disease first described by Kinnier Wilson as lenticular degeneration is a rare autosomal recessive disease of abnormal copper metabolism occurred due to mutation in ATP7B gene in chromosome 13.[1] In a retrospective study done by the Bem et al., the predominant symptoms of Wilson's disease at presentation were hepatic symptoms (38.9%) followed by the mixed symptoms (hepatic and neuropsychiatry symptoms in 30.6%) and neuropsychiatry symptoms (25%).[2] Wilson's disease presenting as the psychotic disorder is a rare phenomenon which often goes undetected and mismanaged with antipsychotic without chelating therapy.[3] We report the case of Wilson's disease with predominant psychiatric symptoms misdiagnosed as a schizoaffective disorder for 3 years and treated with antipsychotics alone without significant improvement.
CASE REPORT
A 42-year-old patient was referred from psychiatry department to department of internal medicine for evaluation of tremor and inability to walk for 6–7 months. The tremor of the patient was progressively increasing in severity and occurs in both resting states and on activity. The patient also had a history of talking excessively mostly about sexual content and abusing relatives verbally for 3 years. There was a history of self-neglect, decreased food intake, muttering to self, and wandering aimlessly. The patient had visited the nearby hospital. Neuropsychiatrist made a diagnosis of schizoaffective disorder and prescribed sodium valproate and olanzapine. There was an improvement in symptoms of excessive talk and muttering to self, but symptoms of wandering aimlessly remained static. Olanzapine was tapered down, and risperidone was started. After 2–3 months of risperidone, the patient had a generalized body shaking. With the frustration, the patient discontinued risperidone and pursues homeopathic medicine. The patient presented to psychiatry outpatient department (OPD) of our institute with symptoms of generalized body shaking, self-neglect, muttering to self, drooling of saliva, and inability to stand. The patient had no family history of psychiatric illness. The diagnosis of psychotic disorder with differential diagnosis of schizoaffective disorder was made and was referred to medical OPD for evaluation of generalized body shaking and work-up for Wilson's disease. On motor examination, hypertonia was present in the limbs. Resting and action tremor was present in all limbs. The speech was dysarthric. The sensory and cranial nerves were normal. On ocular examination, there was greenish golden color deposit along corneoscleral junction which was confirmed to be Kayser–Fleischer (KF) ring as shown in Figure 1. By ophthalmologist, the patient had hemoglobin –12 g/dl, total bilirubin –0.8 mg/dl, aspartate transferase –32 IU/L, alanine transferase –25 IU/L, and alkaline phosphatase –75 IU/L. Serum ceruloplasmin was 17 mg/dl (20–35 mg/dl) and 24-urinary copper was 48.26 μg/24 h (15–70). The diagnosis of Wilson's disease was made on the basis of the decreased level of ceruloplasmin, the presence of KF ring, and 24-h urinary copper level of >40 μg/24 h. We prescribed zinc sulfate 50 mg TDS and olanzapine 7.5 mg OD. The psychotic symptoms and generalized body shaking decrease by 4 months. The course of the disease of the patient is shown in Figure 2.
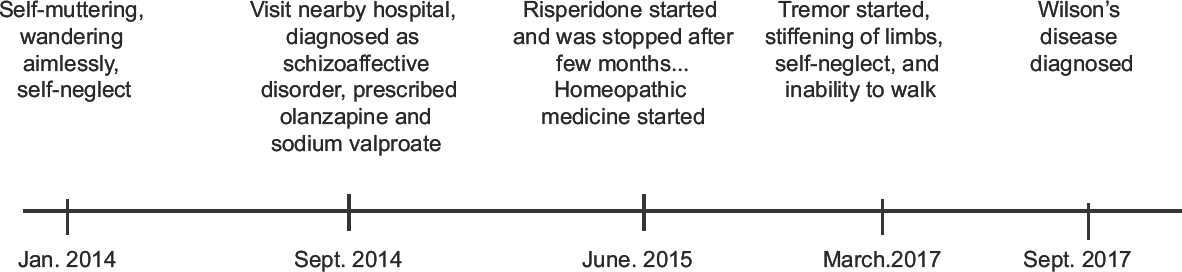
- Timeline showing course of the symptoms of patient with Wilson's disease

- Kayser–Fleischer ring in a patient’ with Wilson's disease along corneoscleral junction
DISCUSSION
Our patient had a history of self-neglect, wandering aimlessly for 3 years and a tremor for 6–7 months. The patient had visited the hospital frequently but was misdiagnosed as a case of schizoaffective disorder and treated with antipsychotics alone and with no improvement. On reevaluation, we diagnose the patient as Wilson's disease. The patient improved significantly with zinc sulfate and olanzapine.
Chakor and Santhosh reported that Wilson's disease patient may present with emotional lability, disinhibition, and severe agitation.[4] Similarly, our patient had the feature of disinhibition such as talking excessively and wandering aimlessly. In a study by Srinivas et al., only 3 had schizophreniform illness among 15 patients with psychiatric predominant manifestation selected from 350 cohorts of Wilson's disease.[5] As psychosis is a rare manifestation, we might miss the diagnosis of patient with wilson's disease having only psychotic symtoms. Bhagat et al. from central Nepal reported a case of a 21-year-old patient who was initially diagnosed with a bipolar affective disorder and later found to be Wilson's disease.[6]
Walshe and Yealland reported that the correct diagnosis of Wilson's disease at the time of presentation was made only in one-third of the total case and the mean delay in diagnosis of other cases was 13 months.[7] The delay in the diagnosis of Wilson disease may be due to the rarity of the disease, varied clinical presentation, lack of awareness among treating physician, not examining the patient properly, error in laboratory analysis of serum ceruloplasmin level, and 24-h urinary copper estimation. Our patient was misdiagnosed which may be due to lack of awareness among physician and not examining the patient properly.
Finding of KF rings in the ocular examination in our patient gave us a clue to diagnose Wilson's disease. Ocular examination of any patients with personality changes and unexplained neuropsychiatric manifestation is a must to diagnose Wilson's disease. KF rings can be appreciated in 85%–100% in a patient with neurological or psychiatry manifestation and 33%–86% with hepatic manifestation.[8]
Another diagnostic clue of Wilson's disease in our patient is the presence of tremor. Any patient with personality changes with unexplained tremor should alert the physician for suspecting Wilson's disease. This highlights the importance of analyzing the tremor which may be misinterpreted as a side effect of antipsychotics.
CONCLUSION
Missing diagnosis of Wilson's disease as an etiology of psychosis can occur in clinical practice that can be avoided by thoroughly examining KF rings in all patients with psychotic symptoms and tremor.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to acknowledge the patient for giving us consent for case report and Editors of Grammarly Application for English Language Editing.
REFERENCES
- Progressive lenticular degeneration: A familial nervous disease associated with cirrhosis of the liver. Brain. 1912;34:20-509.
- [Google Scholar]
- Wilson's disease in Southern Brazil: A 40-year follow-up study. Clinics (Sao Paulo). 2011;66:411-6.
- [Google Scholar]
- Mismanagement of Wilson's disease as psychotic disorder. Adv Biomed Res. 2012;1:61.
- [Google Scholar]
- Severe neuropsychiatric presentation of Wilson's disease. Indian J Psychiatry. 2011;53:170-1.
- [Google Scholar]
- Dominant psychiatric manifestations in Wilson's disease: A diagnostic and therapeutic challenge! J Neurol Sci. 2008;266:104-8.
- [Google Scholar]
- Bipolar disorder and Wilson's disease: A case report. 2015. J Psychiatry Assoc Nepal. 3:50-2. Available from: http://www.nepjol.info/index.php/JPAN/article/view/12399
- [Google Scholar]
- Wilson's disease: The problem of delayed diagnosis. J Neurol Neurosurg Psychiatry. 1992;55:692-6.
- [Google Scholar]
- Diagnosis of Wilson's disease: A comprehensive review. Crit Rev Clin Lab Sci. 2008;45:263-90.
- [Google Scholar]






